All published articles of this journal are available on ScienceDirect.
Thermocycling Stain Challenge and Colour Stability of two Current Zirconium Silicate-filled Indirect Composite Restorative Materials
Abstract
Aim:
This study compares the colour stability of two zirconium silicate-filled indirect composite materials CM and its improved formulation CMD using an in vitro thermocycling stain challenge model with 2 immersion solutions. The rationale of the thermocycling stain challenge model is to replicate the intraoral conditions that the indirect composite materials may be exposed to during a clinical service, water or saliva absorption and cyclical exposure to staining food colourant at varying temperature extremes.
Materials and Methods:
Ten discs each from shade A1 subtypes of CM and CMD indirect composites (Dentine Body A1B, Incisal 58, and Translucent HVT) were subjected to a thermocycling stain challenge following final polishing, which consisted of static immersion in 37°C of distilled water, followed by 500 thermocycles in 5°C of tea and 55°C of soy sauce and finally a 10-minute cleaning using an ultrasonic device. L*, a* and b* colour coordinates were measured, and the mean colour difference expressed as Delta E (ΔE) at different time points of the experiment were calculated and compared.
Results:
CM and CMD indirect composites had a significant color difference at all experimental time points (F=37.818, p<0.001). ΔE for CM subtypes and CMD subtypes in descending order, respectively, were Translucent HVT>Incisal 58>Dentin Body A1B and Incisal 58>Translucent HVT>Dentin Body A1B.
Conclusion:
CMD indirect composite showed improved colour stability compared to CM indirect composite.
Clinical Significance:
Limiting the usage of translucent shades and polishing according to the manufacturer’s recommendation may improve the overall colour of prostheses made using indirect zirconium silicate-filled composite materials.
1. INTRODUCTION
Indirect composite material has been introduced into the dental market to improve composite restoration's marginal integrity and wear resistance for moderate to large defects. The marginal integrity of indirect composite restoration is improved as most of the polymerization shrinkage of the bulk composite material takes place outside the mouth due to external curing. Any shrinkage that occurs is limited to the thin layer of the luting cement used to cement the restoration, which reduces the polymerization stress during the restoration's curing, which may lead to debonding and microleakage. In addition to this, the degree of conversion of the methacrylate double bond from cross-linking of polymers is improved concertedly with a reduction in the plasticizing effect of uncured methacrylate. This results in improved wear resistance of the restoration in the short-term which is material dependent. In terms of aesthetics, fabrication outside the mouth gives better control to the operator or dental technician to develop the morphology and contacts of the restoration [1].
Indirect composite materials are mainly used by the dental technician in the laboratory for the veneering of metal framework for fixed or removable prostheses as well as for the fabrication of metal-free restorations, including inlays, onlays, crowns and fiber-reinforced short-span bridges [2]. The second generation of indirect composites consists of micro-hybrid fillers embedded in resin matrix consisting of conventional monomers such as BisGMA, TEGDMA and UDMA or polyfunctional monomers. Most systems have a laboratory curing unit that may allow heat application [3]. More recent indirect composites consist of nano-filled or nano-hybrid fillers embedded in methacrylate-based monomers. Examples of nanofilled indirect composites include Ceramage and Ceramage Duo, consisting of 73% and 75% zirconium silicate fillers respectively embedded in a UDMA-based resin matrix. The filler and resin matrix composition claimed by the manufacturers has been concurred by an in vitro investigation using thermogra-vimetric analysis and infrared absorption spectroscopy (FTIR) [4]. The high filler loading of these nano-filled indirect composites increases mechanical properties such as hardness and flexural strength [5]. A recent in vitro study reported the highest flexural strength following 40,000 cycles of thermocycling for Ceramage compared to the other indirect composite resins tested in the study. The superior mechanical property was attributed to the combination of filler weight, matrix composition, silanization of the filler particles and polymerization [6].
Despite the improvement in polymerisation shrinkage, handling and mechanical properties, colour stability or discolouration remains a problem for the current indirect composite materials [6]. Other disadvantages of indirect composites compared to ceramics or tooth material include poor abrasion resistance that is material-dependent, which may lead to the poor occlusal wear resistance of a prosthesis made using the material in the long run [7]. Discolouration of indirect composites may be attributed to intrinsic and extrinsic staining. Intrinsic staining may occur through oxidation of unreacted polymer sites following water sorption or due to degradation of unused photoactivator such as camphorquinone or other chromatic degradation products over time that may be material dependant [8, 9]. Water sorption depends on the type of monomers present in the composite, whereby BisGMA and TEGDMA-containing composites may exhibit higher hydrophilicity and water sorption compared to composites containing UDMA. Color changes following water sorption may lead to some colour changes in the composite resin material but at a level below the threshold of clinical acceptability, which is Delta E (ΔE) value of 3.3 [10].
Extrinsic staining occurs mainly due to surface staining from an exogenous substance that is adsorbed onto the surface or absorbed into the subsurface of the indirect composite material [11]. Exogenous substances that may extrinsically stain resin composite materials include melanoidins from coffee, theaflavin from tea, cumin from curry, tannins found in red wine, and carotene from dairy products or carrots. Other than dietary compounds, oral hygiene products that contain cationic antiseptics such as chlorhexidine may worsen staining by binding to and precipitating anionic dietary compounds such as tea and coffee onto resin composite materials [6, 12]. Discolouration of micro-hybrid 2nd generation indirect composite showed worsening over time following exposure to staining agents due to increased surface roughness from toothbrushing and deposition of extrinsic stains [13, 14]. However, extrinsic staining of resin composite materials from dietary colourants may be readily removed by professional cleaning and polishing [6, 12].
The type of staining solution used to assess colour stability may affect the discolouration of 2nd generation indirect composite materials, whereby colour and polarity of dyes in a staining solution may affect staining even more so than the pH of the solution. Coffee that is polar and contains yellow pigments may cause more staining compared to cola despite its lower pH [15]. An indirect composite material used in restoration or prosthesis is persistently exposed to the oral cavity, and thus any in vitro study on colour stability must take into account the cyclic temperature extremes that the restoration may be exposed to during function. Experiments that record the colour changes of composite following static immersions in one single staining solution at 37°C do not take into account the temperature changes that occur in the mouth, the interaction of more than one dietary colourant that may occur during eating or drinking, and represents discolouration that mostly occurs due to extrinsic staining. In addition, static immersion in a staining solution cannot differentiate the discolouration of the composite due to intrinsic staining from extrinsic staining and whether the overall staining can be removed by cleaning [16].
Thermocycling resin composites in dye has been shown to increase the material's color changes compared to static immersion. The reason for this has been attributed in large to the increase of diffusion co-efficient of the staining fluid, which leads to an increase in the amount of dye that diffuses across the unit area of the composite material per unit of time, and to a small degree due to development of microcracks through pre-existing micro gaps or interfacial gaps between fillers and the resin matrix that provides a penetration pathway for stains [17]. Thermocycling is an in vitro ageing test that alternates the restorative material in warm and cold temperatures, and it represents the thermal stress that a restoration may be exposed to during function. Thermocycling at temperature intervals between 5°C and 55°C has been deemed appropriate temperature intervals for an accelerated ageing test by international standards such as ISO [18]. In vivo, validation of 5°C and 55°C temperature intervals using interproximal restorations exposed to hot and cold drinks showed that the temperature recorded was within these two temperature extremes [19].
Table 1.
| Technical Specification | CM (Ceramage, Shofu Inc., Kyoto, Japan) | CMD (Ceramage DUO, Shofu Inc., Kyoto, Japan) |
|---|---|---|
| Filler | Zirconium Silicate (PFS - Progressive Fine Structured Fillers) |
Zirconium Silicate (iPFS – improved Progressive Fine Structured Fillers) |
| Nano sized fillers | Nano sized fillers | |
| Particle distribution of filler | Spherical nanoparticles 20 ~ 40 nm Nanoclusters 0.5 ~ 2 μm |
12 nm ~ 7 μm |
| Filler loading (wt%) | 73 | 75 |
| Resin type | UDMA (Urethane dimethacrylate) UDA (Urethane diacrylate) |
PUDA (Phenylene-included-Urethane diacrylate) DMA (Dendritic multifunctional acrylate) UDMA (Urethane dimethacrylate) |
| Polymerization method | Light Curing | Light Curing |
| Vickers Hardness (Hv0.2) | 74 | 97 |
| Flexural Strength (MPa) | 146 | 202 |
| Flexural Modulus (GPa) | 10.7 | 13.1 |
| Compressive Strength (MPa) | 354 | 445 |
| Diametral Tensile Strength (MPa) | 62 | 72 |
| Toothbrush Abrasion (%) | 0.43 | 0.32 |
The purpose of this study was to investigate the colour changes that an indirect composite material may go through following polishing, water sorption, thermocycling in staining solutions and following stain removal using an ultrasonic device, all of which constituted as a thermocycling stain challenge model to simulate the conditions or challenges that an indirect composite may go through during a clinical service. This may better represent the dynamic staining process of an indirect resin composite during function and has never been done to date. The aim is to compare the color stability of a zirconium silicate-filled indirect composite and its improved formulation following a thermocycling stain challenge. These indirect composite materials have been widely used in Asia. Information regarding the colour stability of these materials will guide clinicians in terms of material selection and application for aesthetic longevity.
2. MATERIALS AND METHODS
This in vitro study was carried out at the Research Laboratory of the Faculty of Dentistry, University Technology MARA (UiTM) between the period of 2019 to 2020. The indirect composites used in the study were Ceramage (CM) (Shofu Inc., Kyoto, Japan) and Ceramage DUO (CMD) (Shofu Inc., Kyoto, Japan). The specific compositions, physical properties and polymerization method of these indirect composites are listed in Table 1. This in-vitro study was divided into a pilot experiment to evaluate the effect of polishing of specimens on the staining of the indirect composite, which subsequently determined the specimen preparation protocol for the main experiment, which consisted of the thermocycling stain challenge.
2.1. Pilot Study
CM indirect composite (shade, Dentine A1B) was selected for the experiment. Composite discs, n=10, with a dimension of 15.0±0.1-mm-diameter and 1.0±0.1-mm-depth were prepared using a customised mold. During preparation, the indirect composite material was overfilled into the mold. The mold was covered with cling film (100μm in thickness) and a perspex plate on either side using finger pressure for 1 minute to remove excess composite material and voids. The perspex plates were then clamped with 4 finger screws, and the composite discs were cured using a laboratory curing unit, Solidilite V (Shofu Inc. Kyoto, Japan), that contains 4 halogen lights (110 V 150 W, light spectrum 400-500 nm) for 3 minutes on each side of the composite discs.
The composites were randomly divided into 2 groups for polish, n=5 and unpolished, n=5 interventions. All composite discs were manually subjected to flash and irregularities removal using 1000-grit abrasive paper on a flat table. Following this, the polish group was polished using Ceramage Polishing Kit (Shofu Inc. Kyoto, Japan) in four sequences from coarse to superfine, following the manufacturer’s instructions. The composite discs in the unpolished group were left as they were following the removal of flash and irregularities. The dimension of the discs was standardized using electronic digital calipers.
The colour of the composite discs was recorded using a dental spectrophotometer (Konica Minolta, Europe) according to the Commission Internationale de l’Eclairege L*a*b* (CIELAB) colour space. Whereby the CIELAB system is a chromatic and value colour space that measures the value and chroma on three colour coordinates: L*–the lightness of the colour measured from black (L*=0) to white (L*=100); a*–colour in the green (a*<0) and red (a*>0) dimensions; and b*–colour in the blue (b*<0) and yellow (b*>0) dimensions. The spectrophotometer was calibrated against a reference plate before each measurement. During all measurements, the L*a*b* values were recorded from the central portion of the disc, defined as the middle third of the disc away from the periphery with a measuring area of 3x3 mm in size. All measurements were made against a white background, and a cylindrical cover with black interior lining shielded the contact cap of the spectrophotometer from an external light source.
Colour measurements were made at the following time points, and the measurement was repeated 3 times for each composite disc:
1. Baseline, (T0/T1): Polished and unpolished indirect composite discs, n=10 following curing, were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
2. Static immersion in distilled water (T2): Following T0/T1, polished indirect composite discs, n=5 and unpolished indirect composite discs, n=5 in, were stored in separate test tubes containing distilled water at 37 ± 2 °C in a dark oven for 7 days to allow for complete equilibration in water. After 7 days, all discs were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
3. Static immersion in staining solution (T3): Following T2, polished indirect composite discs, n=5 and unpolished indirect composite discs, n=5, were stored in separate test tubes containing coffee solution (10 g Nescafe, Nestle Malaysia dissolved in 100 ml of distilled water) at 37 ± 2 °C in a dark oven. The coffee solution was changed every 2 days to maintain its chemical properties. After thermocycling, all discs were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
Mean L*a*b* values were tabulated in Microsoft Excel 2016, and the colour difference, (ΔE) between the experimental timepoints (T0/T1-T2 and T2-T3) was calculated for the polish and unpolish groups according to the formula, ΔΕ= √(L1-L2)2 + (a1 – a2)2 + (b1 – b2)2 [6]. Differences in mean (ΔE) between the polish and unpolish composite at the intervals of (T0-T1) and (T1-T2) were analysed using IBM SPSS software for an independent t-test with a significance level of p < 0.05.
2.2. Thermocycling Stain Challenge
The sample size for repeated measures ANOVA between factors was determined using G*Power 3.0.10 Software (Dusseldorf, Germany) whereby a sample size of 44 for 2 groups (CM and CMD) at 3 repetitions with an effect size of 0.25 and alpha level equal to 0.05 would result in 95% of the power. Based on the sample size calculation and for ease of groupings, ten discs were prepared for each subtype of A1 shade of CM and CMD (Dentin A1B, Incisal 58 and Translucent HVT), giving a total of 60 discs. The composite discs were prepared and polished according to the same methods used in the pilot test. All discs were subjected to the following interventions, which represented the thermocycling stain challenge followed by a corresponding colour measurement as per methods in the pilot study:
1. Baseline, T0/T1: Indirect composite discs, n=60 following curing, were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
2. Static immersion in distilled water, T2: After T0/T1, indirect composite discs, n=10 for each subtype (Dentin A1B, Incisal 58 and Translucent HVT) of shade A1 for CM and CMD were stored in separate test tubes containing distilled water and were stored at 37 ± 2 °C in a dark oven for 7 days to allow complete equilibration in water. After 7 days, all discs were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
3. Thermocycling in staining solutions, T3: After T2, indirect composite discs, n=10 for each subtype (Dentin A1B, Incisal 58 and Translucent HVT) of shade A1 for CM and CMD were thermocycled for 500 cycles between 5°C of tea (Lipton iced tea, Unilever, Australia) as supplied and 55°C of soy sauce as supplied (Sweet Soya Bean Sauce, Habhal, Malaysia). Exposure time was set for 20 seconds, and the transfer time between each staining solution was 5 seconds. All discs were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
4. Ultrasonic cleaning, T4: After T3, indirect composite discs, n=10 for each subtype (Dentin A1B, Incisal 58 and Translucent HVT) of shade A1 for CM and CMD were cleaned for 10 minutes using an ultrasonic machine (Jeio Tech Co. Ltd., South Korea). All discs were rinsed under running water for 1 minute and dried before L*a*b* values were recorded.
Mean L*a*b* values for CM and CMD at T0/T1, T2, T3 and T4 time points were tabulated in Microsoft Excel 2016, and the colour difference (ΔE) between the experimental time points (T0/T1, T0/T1-T2, T2-T3, T3-T4) was calculated for CM and CMD according to the formula given above. Overall differences in mean ΔE for CM and CMD indirect composites and their subtypes (translucent HVT, Incisal 58 and body A1B) at the different experimental time points were compared using Repeated Measure ANOVA between group analysis on IBM SPSS 23 Software. Changes in the L*a*b* coordinates for CM and CMD at different experimental time points were compared using Repeated Measure ANOVA (within-group analysis of experimental effect) followed by pairwise comparison and confidence interval adjustment at a significance level p < 0.05.
3. RESULTS
3.1. Pilot Experiment
The colour difference (ΔE) of CM indirect composite following 1-week immersion in distilled water for the polish group (M = 1.81, SD = 0.74) and the unpolish group (M = 1.25, SD = 0.81) were not significantly different, p = 0.14. However, ΔE of CM indirect composite following 1-week static immersion in coffee for the polished group (M = 1.95, SD = 0.78) and unpolished group (M = 4.13, SD = 1.37) were significantly different, p = 0.01.
3.2. Overall Colour Difference (ΔE) of CM and CMD Indirect Composites during the Thermocycling Stain Challenge
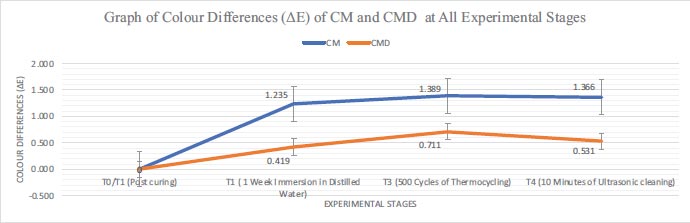
There was a significant difference in mean ΔE for all CM and CMD indirect composites (F=37.818, p<0.001) with differences at T2, T3 and T4 of the experimental time points. CM and CMD composites experienced the highest mean ΔE following immersion in distilled water (T0/1-T2), followed by a slight increase after thermocycling (T2-T3) and minimal reduction in colour change after ultrasonic cleaning (T3-T4) (Fig. 1).
3.3. Colour Differences (ΔE) within Translucent HVT, Incisal 58 and Dentine Body A1B Subtypes for CM and CMD during the Thermocycling Stain Challenge
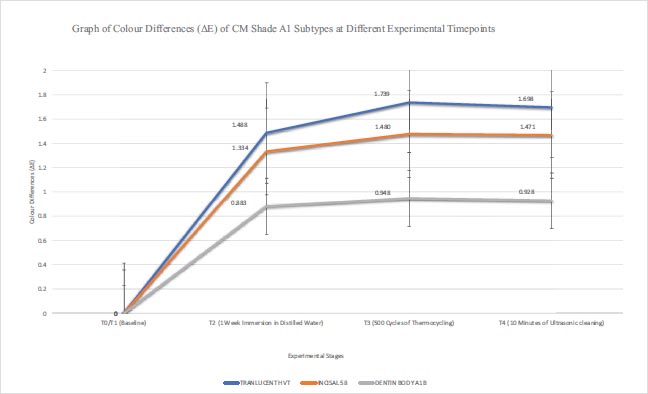
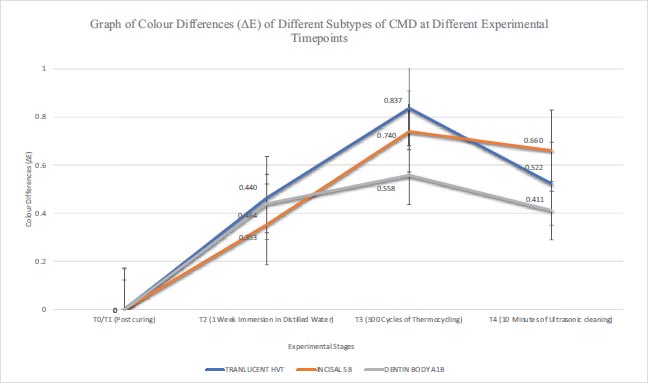
There were significant differences in mean ΔE for all the different subtypes of CM (F=4.817, p=0.001) and CMD at all the experimental time points (F=3.265, p=0.009). The greatest colour change following ultrasonic cleaning (ΔE, T3-T4) in descending order for CM and CMD shade A1 subtypes were Translucent HVT>Incisal 58>Dentin Body A1B and Incisal 58>Translucent HVT>Dentin Body A1B respectively (Figs. 2 and 3).
3.4. Changes in CIELAB Values (L*, a*, b*) for Translucent HVT, Incisal 58 and Dentine Body A1B during the Thermocycling Stain Challenge
As depicted in Table 2, a decrease in L* indicating an increase in darkness of the indirect composite that was significant for CM, shade A1 subtypes translucent HVT, (p=0.003) and Incisal 58, (p<0.001) respectively were seen following 1-week immersion in distilled water. All subtypes of shade A1 of CM underwent further darkening following thermocycling, which was significant for Incisal 58 (p=0.043) and Dentin Body A1B (p=0.003), respectively. An increase in brightness occurred for all shade A1 subtypes of CM following ultrasonic cleaning but at a level that was not statistically significant. In all shade subtypes of CMD, there was a significant decrease in the L* value (p<0.001) following 1-week immersion in distilled water. After thermocycling, there was further darkening for CMD shade A1 subtypes and a slight brightening after ultrasonic cleaning. However, these changes were not statistically significant.
There was an increase in a* value or redness following 1-week immersion in distilled water for all shade A1 subtypes of CM and CMD that were statistically significant (p<0.001), except for Incisal 58 of CMD. Following thermocycling, there was a colour shift towards the green dimension for all shade A1 subtypes of CM and CMD except for Dentin Body A1B, although these changes were not statistically significant. Ultrasonic cleaning did not significantly alter the a* parameter whereby a colour shift towards the green dimension was seen for all shade subtypes of A1 of CM and CMD except for Translucent HVT and Dentin Body A1B of CM (Table 3).
Following 1 week of immersion in distilled water, the indirect composite underwent a shift in colour towards the blue dimension depicted by a decrease in the b* that were significant for all the shade A1 subtypes of CM (p=0.001). Following thermocycling, there was a shift of colour towards the yellow dimension for all the shade A1 subtypes of CM that were statistically significant for Incisal 58 (p=0.02) and Dentine Body A1B (p=0.03). All shade A1 subtypes of CM undergo a colour shift towards the blue dimension following ultrasonic cleaning, although the values were not statistically significant. As for the CMD, following 1-week immersion in distilled water, there was a colour shift towards the blue dimension for all shade A1 subtypes that was statistically significant for Dentine Body A1B (p=0.004). Within the same time interval, there was a statistically significant colour shift towards the yellow dimension for CMD shade A1 subtype, Translucent HVT (p=0.012). There was a colour shift towards the yellow dimension for all shade A1 subtypes of CMD following thermocycling, and the values were statistically significant for Translucent HVT (p=0.005) and Incisal 58 (p=0.037). Following ultrasonic cleaning, there was a colour shift toward the blue dimension for all the shade A1 subtypes of CMD but at a level that was not statistically significant (Table 4).
Table 2.
| Mean Value of L* for CM Indirect Composite | ||||||
|---|---|---|---|---|---|---|
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | - | ||
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | 56.541 (0.35) | 60.731 (0.14) | 73.103 (0.27) | - | - | - |
| T2 | 55.411 (0.43) | 59.546 (0.14) | 73.121 (0.58) | - | - | - |
| T3 | 54.923 (0.14) | 59.305 (1.08) | 72.423 (0.32) | - | - | - |
| T4 | 54.993 (0.15) | 59.352 (0.14) | 72.569 (0.23) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of L* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | 1.130 (0.429, 1.831) |
0.003 | 1.185 (1.024, 1.346) |
<0.001 | -0.018 (-0.521, 0.485) |
>0.95 |
| T2 – T3 | 0.488 (-0.010, 0.986) |
0.056 | 0.241 (0.007, 0.475) |
0.043 | -0.698 (0.253, 1.143) |
0.003 |
| T3 – T4 | - 0.070 (-0.293, 0.153) |
>0.95 | -0.047 (-0.238, 0.144) |
>0.95 | -0.146 (-0.475, 0.183) |
>0.95 |
| Mean Value of L* for CMD Indirect Composite | ||||||
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | - | ||
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | 51.779 (0.39) | 61.898 (0.41) | 73.864 (0.20) | - | - | - |
| T2 | 51.340 (0.39) | 61.584 (0.41) | 73.633 (0.17) | - | - | - |
| T3 | 51.272 (0.45) | 61.631 (0.45) | 73.605 (0.18) | - | - | - |
| T4 | 51.326 (0.46) | 61.688 (0.44) | 73.661 (0.12) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of L* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | 0.439 (0.384, 0.494) |
<0.001 | 0.314 (0.258, 0.370) |
<0.001 | 0.231 (0.160, 0.302) |
<0.001 |
| T2 – T3 | 0.068 (-0.663, 0.799) |
>0.95 | -0.047 (-0.774, 0.680) |
>0.95 | 0.028 (-0.231, 0.287) |
>0.95 |
| T3 – T4 | -0.054 (-0.727, 0.619) |
>0.95 | -0.057 (-0.775, 0.661) |
>0.95 | -0.056 (-0.305, 0.193) |
>0.95 |
| Mean Value for a* for CM Indirect Composite | ||||||
|---|---|---|---|---|---|---|
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | -2.456 (0.05) | -2.088 (0.04) | -1.022 (0.08) | - | - | - |
| T2 | -2.034 (0.05) | -1.789 (0.01) | -0.622 (0.05) | - | - | - |
| T3 | -2.076 (0.04) | -1.804 (0.01) | -0.542 (0.16) | - | - | - |
| T4 | -2.063 (0.04) | -1.808 (0.01) | -0.509 (0.05) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of a* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | -0.422 (-0.459, -0.385) |
<0.001 | -0.299 (-0.332, -0.266) |
<0.001 | -0.400 (-0.437, -0.363) |
<0.001 |
| T2 – T3 | 0.042 (-0.003, 0.087) |
0.074 | 0.015 (-0.005, 0.035) |
0.204 | -0.080 (-0.097, 0.257) |
>0.95 |
| T3 – T4 | -0.013 (-0.071, 0.045) |
>0.95 | 0.004 (-0.020, 0.028) |
>0.95 | -0.033 (-0.231, 0.165) |
>0.95 |
| Mean Value for a* for CMD Indirect Composite | ||||||
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | - | - | - |
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | -1.715 (0.03) | -1.719 (0.03) | -0.876 (0.05) | - | - | - |
| T2 | -1.619 (0.03) | -1.265 (0.99) | -0.580 (0.04) | - | - | - |
| T3 | -1.642 (0.04) | -1.570 (0.03) | -0.512 (0.17) | - | - | - |
| T4 | -1.653 (0.04) | -1.576 (0.02) | -0.566 (0.05) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of a* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | -0.096 (-0.123, -0.069) |
<0.001 | -0.454 (-1.500, 0.591) |
>0.95 | -0.296 (-0.317, -0.275) |
<0.001 |
| T2 – T3 | 0.023 (-0.029, 0.075) |
>0.95 | 0.305 (-0.767, 1.377) |
>0.95 | -0.068 (-0.260, 0.124) |
>0.95 |
| T3 – T4 | 0.011 (-0.051, 0.073 |
>0.95 | 0.006 (-0.028, 0.040) |
>0.95 | 0.054 (-0.136, 0.244) |
>0.95 |
| Mean Value for b* for CM Indirect Composite | ||||||
|---|---|---|---|---|---|---|
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | -7.144 (0.33) | -2.480 (0.09) | 6.784 (0.21) | - | - | - |
| T2 | -7.912 (0.14) | -3.010 (0.14) | 6.143 (0.25) | - | - | - |
| T3 | -5.994 (1.89) | -2.688 (0.19) | 6.587 (0.22) | - | - | - |
| T4 | -7.666 (0.10) | -2.876 (0.12) | 6.356 (0.28) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of b* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | 0.768 (0.553 0.983) |
<0.001 | 0.530 (0.423, 0.637) |
<0.001 | 0.642 (0.509, 0.775) |
<0.001 |
| T2 – T3 | -1.918 (-7.124, 3.288) |
>0.95 | -0.322 (-0.596, -0.048) |
0.020 | -0.445 (-0.868, -0.022) |
0.038 |
| T3 – T4 | 1.672 (-3.515, 6.859) |
>0.95 | 0.188 (-0.081, 0.457) |
0.259 | 0.231 (-0.199, 0.661) |
0.627 |
| Mean Value for b* for CMD Indirect Composite | ||||||
| Time | Transluscent HVT | Incisal 58 | Dentin Body A1B | - | - | - |
| - | Mean (SD) | Mean (SD) | Mean (SD) | - | - | - |
| T1 | -7.145 (0.07) | -2.140 (0.14) | 6.430 (0.16) | - | - | - |
| T2 | -7.050 (0.10) | -2.148 (0.19) | 6.230 (0.20) | - | - | - |
| T3 | -6.711 (0.16) | -1.843 (0.19) | 6.508 (0.24) | - | - | - |
| T4 | -6.795 (0.15) | -1.921 (0.18) | 6.505 (0.22) | - | - | - |
| Repeated measures ANOVA within group analysis (time effect) on Mean Difference (MD) of b* | ||||||
| Comparison | Transluscent HVT | Incisal 58 | Dentin Body A1B | |||
| - | MD (95% CI) |
P-value | MD (95% CI) | P-value | MD (95% CI) | P-value |
| T1 – T2 | -0.095 (-0.169, -0.021) |
0.012 | 0.008 (-0.063, 0.079) |
>0.95 | 0.200 (0.065, 0.335) |
0.004 |
| T2 – T3 | -0.339 (-0.569, -0.109) |
0.005 | -0.305 (-0.594, -0.016) |
0.037 | -0.278 (-0.617, 0.061) |
0.133 |
| T3 – T4 | 0.084 (-0.182, 0.350) |
>0.95 | 0.078 (-0.205, 0.361) |
>0.95 | 0.003 (-0.243, 0.349) |
>0.95 |
4. DISCUSSION
Colour is an important outcome for an aesthetic restorative material; at the time of placement and following function, the colour and translucency of the restoration must match the surrounding tooth structure, especially at the visible areas when restoring anterior teeth and premolars. As such, colour match that consists of colour, shade and translucency is an important criterion used for the clinical evaluation of a restorative material to indicate its success or failure. The ability of the resin composites to retain their colour indicates the colour stability of the material, which determines the aesthetic prognosis for the final restoration [20, 21]. Therefore, this study compared the colour stability of a zirconium silicate-filled indirect composite material and its newly improved formulation. In this experiment, the shade A1 subtypes (Dentine Body A1B, Incisal 58, and Translucent HVT) that are usually layered together during the fabrication of an indirect prosthesis were compared according to the color difference (ΔE), and changes that occurred in the L*a*b* coordinates of the CIELAB color system during a thermocycling stain challenge to assess their color stability.
Prior to the main experiment, a pilot study was conducted to evaluate the effect of polishing on one of the indirect composite materials (CM). The result revealed that the unpolished composite discs stained more (p<0.05), and the colour difference could be observed with the naked eye (ΔE = 4.13). The increase in staining of the indirect composite despite curing under an oxygen-inhibited condition in this experiment by using the Perspex plate may be attributed to the production of a resin-rich layer on the superficial surfaces of the indirect composite discs when cured under this condition. This resin-rich layer has been shown to discolour more when in contact with the oral environment in the long term, which may explain why the unpolished indirect composite in this experiment stained more than the polished specimens following static immersion in coffee solution [22, 23]. The result of our pilot experiment is comparable to a recent in vitro experiment that revealed an unacceptable colour difference, ΔE of more than 3.3 for unpolished indirect composite following static immersion in coffee for 21 days when compared to monolithic CAD/CAM zirconia [24]. Higher staining in coffee staining solution in the pilot experiment compared to following thermocycling in tea and soy sauce in the thermocycling stain challenge may also be attributed to the higher staining potential of coffee compared to tea and soy sauce due to absorption and ionic interaction between the coffee colourant and the amine groups of the resin material [25].
The type of food and beverage selected in this experiment is based on a nationwide dietary intake data conducted in Malaysia, MANS 2014, a nationwide cross-sectional study conducted on more than 7000 subjects aged between 18 to 59 years old. It was revealed that soy sauce is among the top 10 food consumed daily at a prevalence of 20.3%, while tea is the most frequently consumed beverage next to water at a prevalence of 70.3% [26].
The water ageing test has been used as an accelerated ageing test for composite resin, and it is a reliable tool to reflect the discolouration the composite will undergo during a clinical function. However, the colour change will mostly simulate the internal colour change that the resinous material would undergo following oxidation and exposure to clear fluids in the oral cavity [27]. While thermocycling in staining food and beverage was utilised in this in vitro experiment aimed to simulate the dietary consumption of warm and cold beverages during a clinical service [16]. Ultrasonic cleaning used in this experiment was not meant to represent a patient's toothbrushing practices but to remove extrinsic staining following the thermocycling to differentiate between colour changes caused by extrinsic and intrinsic staining of the indirect composite materials. It has been proposed that thermal cycles might occur between 20 and 50 times a day, whereby some 10000 cycles might represent a service year [28]. Therefore, the 500 cycles of thermocycling stain challenge employed in this study equals to 18 days of exposure to staining fluids.
The color difference of 2.6 on the CIE L*a*b* scale is visually perceptible to the naked eye and is regarded as unacceptable in the range of 3.3 to 5.6 [25, 29]. At the end of the experiment, CM (mean ΔE=1.366) experienced greater colour difference than CMD (mean ΔE=0.531). This indicates over 88% in the colour difference between CMD and CM following the experimental ageing using the thermocycling stain challenge model, indicating far superior colour stability for CMD. However, within the limits of this experiment, both composites showed colour changes within clinical acceptability. The colour changes of CM in our study are comparable to a recent study that evaluated the colour stability of direct and indirect composite material according to polymerisation procedures and static immersion in staining solutions. CM indirect composites showed an acceptable colour difference in the tea up to 21 days of static immersion; however, they showed an unacceptable colour difference from 21 days onwards [25].
The color stability of resin composite material may be affected by the complex interaction between filler loading and resin polymer content that may ultimately affect the water sorption of the indirect composite. Distinct changes in the CMD are the addition of two monomers (Phenylene-included Urethane Di-Acrylate (PUDA) and Dendritic Multifunctional-Acrylate (DMA)) in addition to urethane dimethacrylate (UDMA) monomer and filler loading of 75 wt% consisting of nanoclusters. CM contains urethane diacrylate (UDA), urethane dimethacrylate (UDMA) monomers, and predominantly nanosized fillers at 73 wt% filler loading. It is conceivable that the small increase of the filler load with a parallel reduction in the organic content and the addition of a dendritic monomer for the CMD would result in an overall net decrease in water absorption of the resin matrix and improvement in its colour stability [30, 31].
All the subtypes of shade A1 (Dentine Body A1B, Incisal 58 and Translucent HVT) for CMD exhibited greater color stability than CM. When individual subtypes were compared, Dentine Body A1B showed less stain retention as opposed to Translucent HVT and Incisal 58 for both indirect composites. This result is important to the clinician and laboratory technician, considering that all 3 subtypes within a composite shade, such as shade A1 if referring to this experiment, will be utilised in layers to fabricate an indirect composite restoration. The amount of translucent composites, such as Translucent HVT and Incisal 58, may be reduced for the restoration's aesthetics to be retained.
In most of the CMD and all of the CM subtypes, the greatest changes in L* occurred following 1-week immersion in distilled water, which may be attributed to the changes in the light diffraction properties of resin composites that occur following water sorption, mainly due to penetration of water at the resin matrix interface and the hydrophilicity of resin [31]. Following 1 week of immersion in distilled water, both CM and CMD subtypes exhibited *a colour shift towards the red dimension and b* colour shift towards the blue dimension. However, there was a predominant colour shift towards green and yellow dimensions for all subtypes following thermocycling in tea and soy sauce. A previous study conducted on direct resin composites revealed a similar shift of resin composite colour towards yellow (b*>0) following an in vitro thermocycling stain challenge between hot coffee and cold tea [16]. Tannin in tea and caramel in soy sauce may absorb light in the blue spectral region, resulting in the observed yellow discolouration. This effect may be more pronounced for tannin compared to caramel pigments [32]. Overall following ultrasonic cleaning and compared to baseline, CM and CMD composite subtypes became darker with a net red-blue shift in colour.
The data from the water ageing and thermocycling in stain forming the dynamic thermocycling stain challenge model reflects the changes the indirect zirconium silicate-filled composites would undergo as part of the internal discolouration process (intrinsic discolouration) and discolouration from exposure to dietary staining fluids (extrinsic discolouration). By incorporating both these tests, it was shown that most of the discolouration for both CM and CMD was due to internal discolouration of the indirect composites themselves rather than to the adsorption or absorption of staining fluids. Changes in colour that occurred following ultrasonic cleaning may be attributed to the removal of extrinsic stains. The limitation of the present study is the short duration of the thermocycles applied, and future research should include other types of conventional and CAD/CAM indirect composite materials.
CONCLUSION
CMD exhibited improved colour stability when compared to CM at all experimental stages. Within the limitations of this study, Translucent HVT and Incisal 58 exhibited the most colour change compared to Dentine Body A1B for both indirect composite materials. In terms of clinical application, limiting the usage of translucent shades and polishing according to the manufacturer’s recommendation will reduce staining and improve colour stability when using zirconium silicate-filled indirect composite materials.
AUTHORS’ CONTRIBUTIONS
ZHMK carried out conceptualisation, manuscript preparation and correction. MAFA and SR carried out data collection, analysis and paper writing. IHI and NDA carried out proofreading.
LIST OF ABBREVIATIONS
| PUDA | = Phenylene-included Urethane Di-Acrylate |
| DMA | = Dendritic Multifunctional-Acrylate |
| UDMA | = Urethane Dimethacrylate |
| UDA | = Urethane Diacrylate |
| UDMA | = Urethane Dimethacrylate |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No humans or animals were used for the studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
All authors report no conflict of interest, financial or otherwise.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study is available within the article.
FUNDING
None.
ACKNOWLEDGEMENTS
We sincerely appreciate Shofu Inc., Kyoto, Japan, for sponsoring the indirect composite and polishing materials used in the experiment. Our utmost gratitude also goes to the Dean and all faculty members of the Faculty of Dentistry, UiTM, who contributed to this research.


