All published articles of this journal are available on ScienceDirect.
Prevalence and Cause of Enamel Hypoplasia in Primary Teeth among 1-year-old Japanese Children
Abstract
Objective:
In this study, the prevalence and underlying cause of enamel hypoplasia in one-year-old children were examined. Additionally, to determine the association between enamel hypoplasia and exposure to sunlight based on the frequency of the mother’s outings during pregnancy.
Methods:
A total of 273 kids (139 boys) were involved in this study. Based on questionnaires surveys to mothers, oral examinations, and photographs of children's mouths, we looked at the connection between the circumstances of pregnancy and the occurrence of enamel hypoplasia. The presence of enamel hypoplasia was assessed using logistic regression analysis differed among the results of the questionnaire.
Results:
The prevalence of enamel hypoplasia was 38.5%. In the medium and low groups, enamel hypoplasia was more common than in the high group at the birth month of the child (adjusted odds ratio: 3.36, 95% confidence interval: 1.65–6.85, p = 0.001 vs. adjusted odds ratio: 3.76, 95% confidence interval: 1.89–7.48, p < 0.001, respectively). Enamel hypoplasia was knowingly higher among the children whose mothers went out less than 1–2 times a week during pregnancy (adjusted odds ratio: 2.41, 95% confidence interval: 1.04–5.61, p = 0.041). Enamel hypoplasia was significantly more prevalent when mothers used painkillers during pregnancy (adjusted odds ratio: 5.45, 95% Confidence interval: 1.74–17.08, p = 0.004).
Conclusion:
It was suggested that the use of antipyretic analgesics during pregnancy and frequency of outings and variations in sunshine hours according to the child's birth month could affect the occurrence of enamel hypoplasia.
1. INTRODUCTION
One of the basic tooth abnormalities with a high frequency is enamel Hypoplasia that (EH) easily experiences hypoplasia from a histological perspective, and there are several potential causes for its possibility, which are as follows: c. Ameloblastic vital energy or reproduction power is weaker than odontoblast, enamel organ fits outside of dental papilla and is easy to be affected by external obstacles, and enamel is easy to react subtly for stimulation [1]. EH shows more seldomly in primary teeth than in permanent teeth, and the causes of onset are still not fully understood.
When these abnormalities are present in the primary teeth, their parents frequently experience anxiety. Considering that they could easily develop dental caries or negatively impact and functionality of the permanent teeth [2]. According to certain research, children with EH of the primary teeth are more likely to develop caries in their permanent teeth than those without them [3, 4]. In addition, tooth sensitivity is also increased in children with EH due to lower enamel mineralization and exposed dentin [3]. It is crucial to identify abnormalities in the primary teeth and offer the proper treatment and advice to prevent caries in not only the primary but also the permanent teeth.
Recent research has linked calcium homeostasis as a cause of EH [5], and vitamin D (VD) is a crucial player in calcium metabolism. VD, whose main sources are sunlight, dietary, and supplemental intake; has been identified to be one of the nutrients required for tooth development. Rickets, which is caused by a deficiency in VD, is reported to be related to EH [6, 7]. The prevalence of EH in children's permanent teeth was observed to be decreased in those whose mothers got high-dose VD replacement during pregnancy [8]. Another earlier study also demonstrates that the range of EH decreased with increasing serum VD concentrations during pregnancy. These suggest a modifiable relationship between maternal and neonatal factors on prenatal calcium homeostasis in EH [9].
According to reports, certain types of medications used during the development of permanent dentition are linked to EH in permanent teeth [10]. Previous in vitro research revealed that the phase of enamel organs were influenced by the use of medications such as acetaminophen and that its suppression appeared to alter amelogenesis and result in hypo calcification [11, 12]. In other words, the association between medications taken by pregnant mothers during the formation of primary teeth and EH should also be discussed.
To the best of our knowledge, there are few studies in Japan on EH or white spot lesions in primary teeth [13-15]. According to a previous study in 1990 [13], 22.4% of children in primary dentition had EH. Although another research in 1990 [14] examined the causes of EH, it did not address the prevalence or risk factors. Further, a prior study in 2015 [15] found that 12.9% of primary dentition-age children had leukoplakia, but that study did not distinguish between EH and early caries in that study, and the exact prevalence of EH incidence was not clear. The most recent study on early tooth decay and EH in Japan was performed over 30 years ago, therefore it was unable to provide updated information due to numerous climatic, dietary, lifestyle, and other changes. Due to these factors, it is unclear how common EH has become in Japan in recent years, EH of primary teeth in Niigata has not been subjected.
The goal of this study was to learn more about the incidence and causes of EH in 1-year-old children in Niigata, Japan, as well as the connection between EH and exposure to sunlight based on the frequency of outings and prenatal drug use.
2. MATERIALS & METHODS
2.1. Participants
The participants in this study were 1-year-olds (12 months) who had taken part in a free oral health checkup program offered in Niigata municipal health clinics. All parents of children who have attained the age of one received a letter with information on free dental health examinations. Out of the 15 health centers in Niigata city, we chose three for the current study that have dental hygienists on staff. Between October 2018 and July 2019, a total of 12 investigations were conducted over four seasons (fall, winter, spring, and summer) at three healthcare centers in Niigata city. All parents of children attending the dental health examinations received questionnaires. A total of 382 children participated in the dental health examination, of which 324 parents allowed their children (165 boys, and 159 girls) to participate in the study. The survey participation rate was 84.8%. Each participant provided their written informed consent before the study. 51 out of 324 participants were excluded because they were twins, their teeth had not erupted yet, or some data were missing. Finally, 273 children (139 boys and 134 girls) born at 37-41 weeks with complete data were evaluated.
2.2. Questionnaire
Prior to the study, we sent a questionnaire to the parents of the children, which we requested from them in advance. The questionnaire was enclosed with a letter informing the dental health examination. The questionnaire questions were as follows; the birthday of the child, gender, weeks of gestation, birth weight, the type of childbirth, postnatal disease, working status of the mother during pregnancy (yes or no), height and weight of the mother, disease during pregnancy (cold, anemia, impending delivery, or other), medication taken during pregnancy (nothing, folate supplement, iron agent, uterine contracture inhibitor, constipation drug, antipyretic analgesic, or other), morning sickness (not at all, mild illness, serious illness, or hyperemesis gravidarum), weight gain or loss during morning sickness (gain, loss, or no gain nor loss), hospitalization during pregnancy (yes or no), and frequency of outing during pregnancy (almost every day, 3-5 days a week, 1 or 2 days a week, 2-3 days a month, or less than once a month). We gathered the questionnaires on the day of the dental health assessment and inquired about any missing parts.
2.3. Oral Examination
All oral examinations were performed by two trained dentists, who also recorded the findings in a protocol. When the calibration was done before the investigation, a 95.7% rate of agreement was reached and the diagnosis of EH was attained. We diagnosed EH based on inspection and palpation after drying the surface of the teeth with cotton rolls. Additionally, we examined the teeth for location, color (white opacity, yellow/brown opacity), and enamel defects related to EH. Teeth with EH were categorized according to the degree of EH and the highest score was recorded (Table 1).
Additionally, we used a digital oral photographing apparatus to take mouth pictures, and then we set up color charts for image correction and added color tone correction to the images. Following the oral examinations, one trained dentist re-evaluated the outcomes based on intraoral photographs with a protocol.
2.4. Statistical Analysis
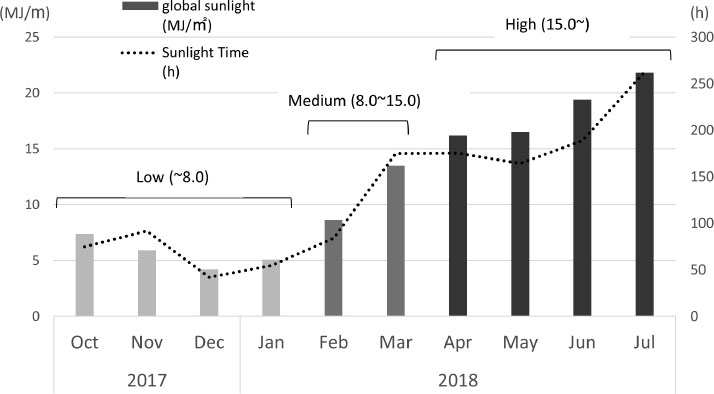
To assess the prevalence of EH and the differences in location between teeth, cross-tabulation was used. The existence of EH was defined as the dependent variable and the answer contents from the questionnaire were independent variables. Additionally, postnatal diseases, pregnancy-related illnesses, the gender of the child, and hospitalization during pregnancy were evaluated as co-variants. Analysis was carried out by dividing their month of birth into the following groups depending on the total solar radiation in Niigata (Fig. 1): low (8.0 MJ/m2 or less); medium (8.0 MJ/m2–15.0 MJ/m2); and high (15.0 MJ/m2 or more). STATA 14 (Stata Corporation, College Station, TX, USA) was utilized for all statistical calculations, with values of p < 0.05 taken as indicating statistical significance.
3. RESULTS
The prevalence of EH was 38.5%. Among them, score 1 was 93.3% while the others had a score of 2. The mean number of present teeth was 6.5 ± 2.5, and among the total number of present teeth (1,767), 219 teeth (12.4%) were influenced by EH. The maxillary left central incisor was affected by EH (34.3%), followed by the maxillary right central incisor (34.2%). The mandibular left lateral incisors were the least affected (0.9%) (Table 2). The average gestational age was 39.1 ± 1.1, and the average birthweight was 3094.7 ± 381.8 g. respectively. Antipyretic analgesics used during pregnancy significantly increased the risk of EH (p = 0.003) (Table 3). In all other findings, there were no significant differences.
The relationship between EH and solar radiation, frequency of outing, and use of antipyretic analgesic is shown by logistic regression analysis in Table 4 of the study. In Niigata, the prevalence of EH was substantially greater in the medium and low groups and significantly higher than that of the high group depending on the child's birth month (adjusted odds ratio (adjOR): 3.36, 95% confidence interval (CI):1.65–6.85, p = 0.001 vs. adjOR: 3.76, 95% CI: 1.89-7.48, p < 0.001, respectively). We evaluated the data statistical comparison between each variable and discovered no significant difference between the medium and low groups. Regarding the frequency of outings during pregnancy, EH was significantly higher when this was not more than 1-2 days a week (adjOR: 2.41, 95% CI: 1.04-5.61, p = 0.041). There was no significant difference between the medium and low groups, 3-5 days per week and 1-2 days per week or fewer when we performed a statistical analysis of the data for each variable. There was no significant difference between 3-5 days per week and 1-2 days per week or fewer when we compared the data statistically for each variable. Regarding medicine used during pregnancy, EH was significantly more predominant when antipyretic analgesics were used (adjOR: 5.45, 95% CI: 1.74-17.08, p = 0.004).
| Score | Findings |
|---|---|
| 0 | Without Enamel Hypoplasia (EH) |
| 1 | EH in less than one-third of the tooth on at least one surface |
| 2 | EH in one-to two-thirds of the tooth on at least one surface |
| 3 | EH in more than two-thirds of the tooth on at least one surface |
| The highest score was recorded. | |
| - |
Affected by EH
n (%) |
|---|---|
| Maxillary left central incisor | 75 (34.3) |
| Maxillary right central incisor | 74 (34.2) |
| Maxillary right lateral incisor | 24 (10.8) |
| Maxillary left lateral incisors | 22 (9.9) |
| Mandibular left central incisor | 12 (5.5) |
| Mandibular right central incisor | 10 (4.6) |
| Mandibular left lateral incisors | 2 (0.9) |
| Total | 219 |
| - | - | n=273 | - | - |
|---|---|---|---|---|
| Without EH n (%) |
With EH n (%) |
p-value | ||
| 168 (61.5) | 105 (38.5) | - | ||
| Gender | Male | 84 (50.0) | 55 (52.4) | 0.702 |
| Female | 84 (50.0) | 50 (47.6) | ||
| Weeks of gestation (mean ± SD) | - | 39.0 ± 1.1 | 39.2 ± 1.0 | 0.537 |
| Birth weight (mean ± SD) | - | 3072.1±363.0 | 3133.4±406.2 | 0.196 |
| Type of childbirth | Normal delivery | 134 (80.7) | 82 (78.9) | 0.377 |
| Postnatal disease | Nothing | 21 (12.5) | 14 (13.3) | 0.841 |
| Working status during pregnancy | Yes | 123 (73.2) | 70 (66.7) | 0.248 |
| Height of mother (mean ± SD) | - | 158.6±5.4 | 158.8±5.0 | 0.686 |
| Weight of mother (mean ± SD) | Prenatal | 52.3±8.5 | 53.3±8.6 | 0.354 |
| End of pregnancy | 62.4 ± 9.3 | 63.2 ± 9.0 | 0.500 | |
| Disease contracted during pregnancy | Cold | 54 (32.1) | 31 (29.5) | 0.649 |
| Anemia | 45 (27.0) | 28 (26.7) | 0.960 | |
| Impending delivery | 27 (16.1) | 11 (10.5) | 0.194 | |
| Other | 23(13.7) | 15 (14.3) | 0.890 | |
| Medication was taken during pregnancy | Nothing | 55 (32.7) | 30 (28.6) | 0.469 |
| Folate supplement | 50 (29.8) | 37 (35.2) | 0.345 | |
| Iron agent | 36 (21.4) | 16 (15.2) | 0.205 | |
| Uterine contracture inhibitor | 19 (11.3) | 10 (9.5) | 0.641 | |
| Constipation drug | 14 (8.3) | 10 (9.5) | 0.735 | |
| Antipyretic analgesic | 6 (3.5) | 14 (13.3) | 0.003 | |
| Other | 38 (22.6) | 22 (21.0) | 0.746 | |
| Morning sickness | Not at all | 10 (6.0) | 8 (7.6) | 0.937 |
| Mild illness | 114 (67.9) | 68 (64.8) | ||
| Serious illness | 38 (22.6) | 25 (23.8) | ||
| Hyperemesis-gravidarum | 6 (3.6) | 4 (3.8) | ||
| Weight gain and loss during morning sickness | No gain or loss | 79 (47.0) | 49 (46.7) | 0.441 |
| Gain | 43 (25.6) | 21 (20.0) | ||
| Loss | 46 (27.4) | 35 (33.3) | ||
| Hospitalization during pregnancy | Yes | 21 (12.5) | 9 (8.6) | 0.313 |
| Frequency of outing | Almost every day | 112 (66.7) | 61 (58.1) | 0.136 |
| 3–5 days a week | 42 (25.0) | 27 (25.7) | ||
| 1 or 2 days a week | 10 (6.0) | 14 (13.3) | ||
| 2–3 days a month | 2 (1.2) | 3 (2.9) | ||
| Less than once a month | 2 (1.2) | 0 (0.0) |
| - | n = 273 | ||||||
|---|---|---|---|---|---|---|---|
| Total | Without EH | With EH | Crude OR (95%CI) |
Adjusted OR (95%CI) | p-value | ||
| - | 168 (61.5%) | 105 (38.5%) | |||||
| Solar radiation (MJ/m2) | High | 87 | 69 (79.3%) | 18 (20.7%) | 1.00 (Reference) | ||
| - | Medium | 82 | 45 (54.9%) | 37 (45.1%) | 3.27 (1.81–5.92) | 3.36 (1.65–6.85) | 0.001 |
| Low | 104 | 54 (51.9%) | 50 (48.1%) | 3.27 (1.81–5.93) | 3.76 (1.89–7.48) | <0.001 | |
| Frequency of outing | Almost every day | 173 | 112 (64.7%) | 61 (35.3%) | 1.00 (Reference) | ||
| - | 3-5 days per week | 69 | 42 (60.9%) | 27 (39.1%) | 3.27 (1.81–5.95) | 1.19 (0.64–2.20) | 0.583 |
| 1-2 days per week or less | 31 | 14 (45.2%) | 17 (54.8%) | 3.27 (1.81–5.96) | 2.41 (1.04–5.61) | 0.041 | |
| Antipyretic analgesic taken during pregnancy | Yes | 20 | 6 (30.0%) | 14 (70.0%) | 4.23 (1.57–11.38) |
5.45 (1.74–17.08) |
0.004 |
| Logistic regression analysis was conducted using postnatal disease, pregnancy disease, gender of the child, and the presence or absence of hospitalization during pregnancy as covariances. OR: Odds Ratio CI: Confidence Interval |
|||||||
4. DISCUSSION
To our knowledge, this is the first study to investigate EH in the primary teeth of 1-year-old children in Niigata. A systematic analysis found that the prevalence of EH will range from 15% to 49% in 2022 [16], compared to 22% in Asia in 1994 [17]. The prevalence of EH in this study (38.5%) was significantly higher than those in prior studies, because the actual prevalence of EH, which is recognized only after the completion of primary dentition, is likely to be higher than that observed in the present study as the participants were children aged 1 year which had un-erupted teeth. However, since each study's evaluation criteria are different, it is challenging to make general comparisons because diagnoses were made solely on oral examinations. In our study, the majority of the subjects with EH (93.3%) had an EH score of 1, and most cases were minor. If EH was diagnosed, it is possible to respond by offering standard dental health advice without making the parents or guardians feel anxious.
With patients exercising practically daily while pregnant, the prevalence of EH in this study was noticeably decreased, and a seasonal variation in the incidence of EH was noted. This finding implies that EH is related to the synthesis of VD, in which VD promotes tooth formation and growth by regulating calcium metabolism. The daily recommended VD consumption is 5.5 μg for non-pregnant people and 7.0 μg for pregnant people, according to Japanese dietary intake standards [18]. The daily average VD consumption in Japan is 12.4 ± 8.1 μg for young women [19]. However, this benchmark quantity was determined by multiplying a synthetic amount from sunlight. The risk of VD insufficiency appears to be higher in Japan, where younger people consume less fish than older people do, and women in particular tend to avoid direct sunlight to prevent sunburn [20]. Conversely, according to the dietary intake standards in the USA, the estimated average necessary amount of VD calculated without considering sunlight is 10 μg/day, and the recommended amount obtained is 15 μg/day [21].
The National Institute for Environmental Studies, Japan [22] offers the ultraviolet irradiation time required to generate 10 μg of VD consumed in a meal which is insufficient when the face and hands are exposed at each observation point in Japan, and the closest observation point to Niigata is Tsukuba Observation Point. Thus, to reach the necessary levels in Tsukuba, it takes 9 minutes in mid-July and 50 minutes in mid-January. In comparison to Tsukuba, it takes longer in Niigata during the winter when the skies are more gloomy.
In other words, serum VD concentrations might not be enough even if the dietary intake standard is met and the chance of exposure to sunlight is small. A 2014 survey found that 60% of pregnant women reported that their serum VD concentration was below the reference value of 20 ng/mL and that they were in a serious VD-deficient condition; by contrast, serum VD concentrations were high among pregnant women who had prolonged exposure to sunlight in the summer [23]. Recent investigations have demonstrated that maternal serum VD concentrations in the latter half of pregnancy are lower than in the first half of pregnancy in Japanese pregnant women [24]. Enamel calcification occurs during tooth development from late in pregnancy until 2.5-3 months after birth. Half of the maxillary anterior teeth, which were frequent EH, were completed at birth on the crown side. Therefore, it is believed that the creation of VD from sunshine exposure after the late gestation period phase aids in the prevention of EH.
In addition, this poll did not take pregnancy-related meals into account. According to a thorough study by the Japanese Society of Pediatric Dentistry, there is little Molar Incisor Hypo-mineralization (MIH) in Hokkaido and Tohoku, and higher in Kyushu and Okinawa [25]. This is believed to be connected to consuming fish and shellfish rich in VD. A recent study demonstrated a strong correlation between inadequate maternal VD measured during pregnancy and the number of affected teeth in MIH patients [26]. In Japan, the use of VD supplements is not common and VD fortification of foods is uncommon [27]. When the amount of VD synthesis by sunlight is reduced, for example, in the latter half of pregnancy in winter or in cases where few opportunities for outing exist due to hospitalization, it is necessary to increase the intake of VD through meals.
The outcomes revealed a high prevalence of EH in children whose mothers ingest antipyretic analgesics during pregnancy. Pain such as headaches and lower back pain can be a major stress for the mother, resulting in the use of antipyretic analgesics. For instance, psychogenic factors like anxiety and depression are known to be closely linked to the onset and progress of migraine and tonic headaches, and these can easily be accompanied by mental illnesses such as anxiety and emotional disorders [28]. The blood concentration of VD has been linked to sadness and stress in certain studies [29], and it is plausible that stress brought on by pain may cause a decrease in the blood concentration of VD during pregnancy and be linked to the development of EH. Chronic mental stress also stimulates thehypothalamus–pituitary–adrenocortical system and sympathetic nervous system, which suppress sex and growth hormones. As a result, it is also known that inflammatory cytokines are elevated, which ultimately causes a decrease in bone mass due to the stimulation of bone absorption and repression of bone production [30, 31]. Hence, a more multifaceted approach to EH is likely to be needed in the future.
Among the 20 mothers who had taken antipyretic analgesics in this study, 17 used acetaminophen, two used NSAIDs and the rest used both; thus, the overwhelming majority used acetaminophen. Acetaminophen passes through the placenta, but it is known to be safe for short-term use. However, several studies have revealed a link between long-term, high-dose use related to neurodevelopmental disorders, respiratory illness, reproductive damage, pulmonary disease, and neurodevelopmental abnormalities [32, 33]. Especially neurodevelopmental disorders, a Norwegian study of 12,973 mothers and children showed that the children of mothers taking acetaminophen continuously for 22 days or more during pregnancy were associated with higher rates of attention deficit hyperactivity disorder (ADHD), and a reverse correlation was found for those taking it for 8 days or less [34]. According to the 2022 review, there is a connection between acetaminophen use and neurodevelopmental outcomes such as autism spectrum disorder, intellectual quotient (IQ), ADHD, isolated language, attention and executive function, communication, behavior, and psychomotor development. Long-term use, increased dose, and frequency were associated with stronger associations [35]. As previously mentioned, numerous reports have observed that fetuses are susceptible to developmental abnormalities or ADHD, and some people have suggested that caution is required when using acetaminophen during pregnancy [36]. The underlying processes of these problems are yet unknown, and the requirement for long-term administration of acetaminophen administration may have an impact on the disease itself. Acetaminophen use during pregnancy is safe and has not been definitively linked to ADHD, according to the US Food and Drug Administration [37]. Antipyretic analgesic use during pregnancy was not documented in this study, and it is doubtful that it was used extensively. Clarifying the link between EH and the use of antipyretic analgesics are therefore quite challenging. All medications, including acetaminophen, should be used when necessary, during pregnancy only if required, and only after carefully weighing the benefits and hazards.
The present study had some shortcomings. First off, because this study was conducted on a convenience sample, all 1-year-old children were included in the study. In Niigata, we were able to confirm a typical prevalence of EH among 1-year-old children. Second, because many of their primary teeth have not yet erupted, it was not possible to determine the precise prevalence of EH in primary teeth for 1-year-old children in this study. Children with fully erupted primary teeth need to be the subject of more research in order to thoroughly examine this topic. Third, this study did not look at the food intake throughout pregnancy; this would have provided more reliable data on the relationship between EH and VD. Fourth, we did not consider mothers with chronic health problems or who had any complications during pregnancy; we should have also taken into account the mother's general condition during pregnancy for a more detailed study.
CONCLUSION
Our outcomes indicate that differences in sunlight hours according to the birth month of the child, use of antipyretic analgesics during pregnancy, and frequency of outings could influence the incidence of EH. Further studies are required to confirm this mechanism.
LIST OF ABBREVIATIONS
| EH | = Hypoplasia |
| VD | = Vitamin D |
| IQ | = Intellectual quotient |
| ADHD | = Attention deficit hyperactivity disorder |
| EH | = Enamel Hypoplasia |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Board of Niigata University (approval No. 2018-0077; date of approval: June 18, 2018).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the base of this research. The reported experiments were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants were given a written consent form and were assured of the confidentiality of the data.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [A.M] on special request.
STANDARDS OF REPORTING
STROBE guidelines were followed.
FUNDING
This study was supported by Japan Society for the Promotion of Science KAKENHI Grant Number JP19K10441.
CONFLICT OF INTEREST
The authors confirm that there is no conflict of interest related to the manuscript.
ACKNOWLEDGEMENTS
The authors wish to thank the staff of the Health Improvement Division of Niigata city for their support in the completion of this study.


