All published articles of this journal are available on ScienceDirect.
Potential Side Effects of Comprehensive Fixed Orthodontic Treatment: A Narrative Review
Abstract
Orthodontics is a specialty derived from dental sciences that starts by diagnosing, preventing, intercepting, modifying growth, and treating all dentofacial discrepancies. Medical interventions can cause harm besides their benefits. This review is done to evaluate the most common potential risks that can be caused by orthodontic treatment and detect the most common factor in the treatment that may lead to this hazard. The review was conducted based on PRISMA-S guidelines for literature search strategy for systematic reviews. Despite all the beneficial effects of orthodontic treatment, it also has negative effects on oral and peri-oral structures and social well-being. It is also important to obtain informed consent from patients before the initiation of any orthodontic procedure, especially in cases with a history of trauma or known adverse reactions.
1. INTRODUCTION
Knowing the potential side effects of any treatment or intervention is essential before deciding on a treatment plan for any given case. Adverse effects of treatment can harm various facets of the patients including their physical health, social status, and emotional well-being. Like any other dental or medical treatment, orthodontic treatment with its great advantages to the patients is also prone to cause some significant side effects and complications [1]. The decision to start orthodontic treatment requires evaluating the pros and cons of this intervention on the patient’s overall health [2]. Orthodontic treatment is a branch of dentistry that can improve the patient's oral health, function, and esthetics, and raise their self-esteem. However, orthodontic fixed appliances can cause significant harm to the hard and soft tissue structures of the oral cavity [3]. The increased chance of negative effects associated with comprehensive orthodontic treatment may limit the treatment options or reduce the expected treatment objectives [2]. It is important to make for each patient a full clinical examination and profile analysis, followed by obtaining signed informed consent. In case of any unwanted side effects, ignoring or failing to identify and manage them and ignoring to inform the patient regarding the same can be considered unprofessional behavior which could lead to patient dissatisfaction, malpractice complaints, and lawsuits [4]. However, most of the adverse effects could be prevented and effectively managed if the dental practitioner has better awareness and knowledge regarding them. This review aims to evaluate and mention the most common adverse effects that can be caused by orthodontic treatment and the risk factors that can increase the chance of these effects in addition to discussing the latest information relevant to this subject.
2. METHODOLOGY
The present study is a narrative review that used PRISMA-S, an extension of PRISMA guidelines for reporting strategies of literature search in systematic reviews [5]. A search for relevant articles was made in web-based databases: PubMed, Ovid Embase-I-Ovid Embase Classic, Cochrane library, Web of Science, Research gate, Google Scholar, and preprint databases including Researchsquare and Medrxiv. The keywords were used in multiple combinations which include ‘orthodontic treatment’, ‘adverse effects’, ‘side effects’, ‘dental side effects’, ‘root resorption’, ‘pain’, ‘periodontal disease’, ‘pulp vitality’, ‘temporomandibular joint disease (TMD)’, ‘risks’, ‘oral traumatic ulcer’, ‘tooth decalcification’. Only articles and preprints in the English language were included in the review. The abstracts of the articles were read and those that did not fulfill the requirements of the present study, animal studies, and non-clinical studies were excluded.
3. RESULTS
In the present study, a thorough literature search and review showed root resorption, loss of periodontal support, decalcification, temporomandibular joint diseases, traumatic ulceration, and pulpal death to be significant adverse effects of comprehensive fixed orthodontic treatment. The current review has found that:
1. All types of orthodontic treatments are associated with root resorption.
2. Orthodontic treatment is associated with oral ulceration, particularly traumatic ulcers.
3. It is approved that pulpal death it is not associated with orthodontic treatment and may be related to other trauma.
4. Orthodontic treatment is the main cause of plaque accumulation and decalcification of the enamel.
5. There is no increase in the prevalence of TMJ diseases concerning comprehensive orthodontic therapy, even with extraction or non-extraction approaches.
4. DISCUSSION
4.1. Root Resorption
Root resorption is a very common consequence of fixed orthodontic treatment. Usually, about 1mm of root length will be resorbed. Sometimes, lateral root resorption is associated with a fixed orthodontic appliance, and its degree is unpredictable [6, 7]. Orthodontic-related root resorption rarely jeopardizes the prognosis of teeth. Anterior maxillary teeth were found to be more likely to undergo root resorption in response to fixed orthodontic treatment when compared to other teeth [8].
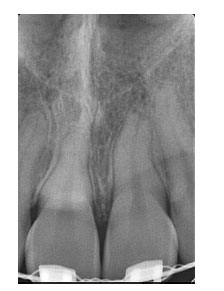
Vertical bone resorption due to active periodontal diseases can cause a significant loss of attachment and decrease the periodontal support than the resorption around the tooth apex (Fig. 1). The underlying pathological mechanism of orthodontic-related root resorption is undefined. Microscopical root resorption is a characteristic feature of all permanent teeth undergoing fixed orthodontic treatment. It is radiographically apparent but clinically insignificant [9]. Some theories include excessive force and the formation of hyalinized tissue of the periodontal ligament which leads to undermined resorption. There is no reported direct cause that can be pointed out, but it is clear that some risk factors are associated with cases of severe resorption [3]. Apart from the treatment-related factors like range of movement, the magnitude of applied force, duration of treatment, and type of appliance used, factors specific to individuals also have been found to be potential risk factors [10-15]. The individual factors that could improve the incidence of root resorption in response to orthodontic treatment include root morphology [10, 11, 16-18], history of trauma to teeth [10, 11, 19-21], the vitality of teeth, patient habits [22, 23], systemic diseases [11], genetic factors, and age [10, 24-26] (Table 1).
| 1 | Root morphology | • Pipette-shaped roots show a greater amount of resorption than other root forms 11, 16. • Deviating root form, narrow roots converging apical root canal are more prone to resorption 10, 17. • Short roots and long roots are more at risk of resorption than average-length roots 10, 11, 18. |
| 2 | History of trauma to teeth | Teeth with a history of root resorption from previous orthodontic treatment, have an increased risk of further resorption 10, 11, 19, 21. Anterior teeth with a history of trauma have a higher risk of root resorption 20. |
| 3 | Quality of endodontic treatment of teeth | Teeth with shorter fillings of the root canal that do not reach the apex undergo resorption of the part without filling 10, 11. |
| 4 | Duration of treatment | Increased length of treatment increases the risk of root resorption 11-13. Length of treatment with rectangular wires was found to be a risk factor for root resorption 14. |
| 5 | Excessive orthodontic force | Heavy forces applied during orthodontic treatment are associated with root resorption 15. |
| 6 | Patient habits | Thumb sucking and chronic bruxism may increase the risk f root resorption 22, 23. |
| 7 | Systemic diseases | Hypothyroid individuals have low bone turnover and are at higher risk of root resorption 11. |
4.2. Periodontal Disease
Gingivitis, periodontitis, and loss of periodontal support comprise periodontal disease [27, 28]. In cases where fixed appliances have been placed, gingival inflammation is frequently observed due to the decreased access to maintain proper oral hygiene which causes an increase in the volume of dental plaque [6]. The bacteria in the dental plaque are responsible for causing periodontal disease [29]. Periodontal tissues can be affected by some diseases like gingivitis, resorption of the alveolar bone as the active periodontitis, and loss of periodontal attachment during orthodontic treatment [27] (Fig. 2) presence of plaque is an important risk factor for the development of periodontal disease during orthodontic treatment [30]. The oral soft tissue reaction toward the metallic orthodontic appliances can be caused by several factors, like the patient’s immunity, the presence of any systemic diseases, and the presence and composition of calculus. Although, general health factors, such as smoking, can lead to compromised periodontal health. Furthermore, some potential side effects can be seen with the uncontrolled diabetic patient on periodontal tissue when the orthodontic treatment is established like, increasing the possibility of periodontal breakdown [31].

After placing the fixed orthodontic brackets, some patients can suffer from mild gingival inflammation, and in most cases, it’s temporary and doesn’t cause loss of attachment [3]. Some investigators reported that metallic orthodontic brackets can change the type of oral cavity bacterial flora. So, orthodontic intervention with metallic brackets may cause some types of localized gingivitis, with a very weak chance to develop into periodontitis [32].
4.3. Decalcification
White spot lesions or demineralization of the enamel is a common side effect of using metallic orthodontic appliances. Decalcification is the beginning sign of the caries process. White spot lesions can occur in about 50% of orthodontic patients with the upper anterior teeth as the most affected teeth in the mouth (Fig. 3). In addition, these side effects can be seen within one month, which is the usual time for orthodontic visits [33]. The presence of orthodontic brackets can elevate the accumulation of dental plaque.

Usually, these spots decrease in size after the removal of the appliance. Some of these lesions could be permanent lesions on the enamel [6, 34]. Usually, the orthodontic patient will have some disturbance in the oral cavity flora, like a revival in Streptococcus mutans counts and increased food stagnation with a difficulty in maintaining good oral hygiene [3]. If the orthodontist observed the decalcified areas on the enamel after the debonding procedure, he should not direct his treatment toward invasive measures like intensive fluoride application or enamel microabrasion. The orthodontic patient should be seen in a regular follow-up visit to allow these areas to be re-mineralized. In these circumstances, the orthodontist should instruct the patient to maintain good oral hygiene, with the help of a prescribed daily fluoride-containing mouthwash. Fluoride varnish application on these lesions should be avoided at the debonding visit because high fluoride concentration will prevent the mineralization process [33].
4.4. Temporomandibular Joint Diseases (TMD)
Some old theories are indicating that orthodontic intervention can lead to TMD. On the other hand, other authors recommend orthodontic therapy to control or prevent TMD [6, 35].
There is no one etiological factor that can be palmed to cause TMD because it is a multifactorial condition. Some investigators reported that some dental malocclusion can be considered in some cases as a causative factor, but it is not the sole etiological factor. Dentofacial vertical deformity that manifested as an anterior dental open bite, deep overbite, or sagittal discrepancy with increased overjet can be related to osteoarthritic TMD disorders [36], there is no evidence-based research that pinpointed the increased overbite or overjet as the main factor in the pathological mechanism of these diseases. The loss of posterior vertical support because of early loss of molar teeth can be correlated with TMJ osteoarthrosis depending on its severity. Furthermore, unilateral, and bilateral posterior crossbites do not aggravate the TMJ signs and symptoms.
Shah and Santner [37] stated that some occlusal factors can be related to TMD in some groups. The increases in the potential risk to develop TMD with open bite malocclusion, unilateral scissor bite, increased sagittal overjet of more than 7 mm, more than 5 lost molars teeth, and centric occlusion (CO) centric relation (CR) shift of more than 2 mm. The overall percentage of related occlusal factors in the development of TMD is only about 10–20% with 80–90% related to other variables [36]. This systematic review which was done in 2010 evaluating orthodontics as a causative factor in the development of TMJ disorders, stated that there is no increase in the prevalence of TMJ diseases concerning comprehensive orthodontic therapy, even with extraction or non-extraction approaches [38].
4.5. Traumatic Ulceration
The oral cavity is covered with a very thin epithelial mucosal membrane that can be easily ulcerated or damaged. These traumatic ulcerations are easily developed from sharp tooth edges, traumatic biting, and hard food parts. After the mucosa is injured, it becomes exposed to be superimposed by infections from the normal oral flora [39, 40] Metallic orthodontic appliances can increase the chance of tissue ulcerations [4]. Traumatic ulcerative lesions can occur during orthodontic therapy with both fixed brackets and removable appliances. It is not uncommon to observe the relationship between fixed appliances and oral ulcerations [6]. During orthodontic treatment, intra- and soft tissue ulcerations or even allergic reactions may appear. For the intra-oral lesions, the pathological mechanism can be summarized as the direct contact of oral soft tissues and the orthodontic appliances. Another iatrogenic factor could be related to the improper handling of the instruments during treating orthodontic patients. The clinical presentations of these lesions usually could be seen as oral ulcers on the buccal or labial mucosa or traumatic keratosis that can be resulted from the friction between the orthodontic brackets and the checks. (Fig. 4). Also, the lingual mucosa and the tongue could be affected by these lesions.

Some symptoms like burning pain can be associated. The first option for the orthodontist to deal with these side effects is to use orthodontic wax on the sharp or most prominent part of the appliance. If the patient has very bad oral hygiene or does not take good hygienic care of the removable appliance, he could develop a fungal infection caused by Candida albicans [37]. Around 60 to 80% of all oral ulcers are traumatic ulcers, while about 8 to 30% of the cases are diagnosed with aphthous ulcers [41].
4.6. Pulpal Death
Uncontrolled orthodontic apical movement can reduce apical blood perfusion and lead to pulp damage [6, 42]. Dental pulp reacts minimally to the orthodontic force. These reactions are usually temporary with some inflammatory response, with no permanent damage. There is very weak evidence about the loss of pulp vitality during orthodontic therapy [43]. The history of trauma was linked to pulp death as a risk factor during orthodontic treatment. Comprehensive pre-treatment clinical and radiographic examination with periapical radiographs of traumatized teeth is an important part of such cases. In addition, heavy uncontrolled orthodontic forces with back-and-forth movement may lead to pulp death. Therefore, light-controlled forces should be considered during the treatment of these cases [44]. The non-bacterial pulp death cannot be correlated clinically or even experimentally to the orthodontic intervention. If the orthodontist faced sudden pulp necrosis during the orthodontic treatment, the history of trauma should be ruled out and the orthodontic movement should be discontinued [43].
CONCLUSION
Orthodontic treatment is like any other medical or dental intervention that can cause negative side effects. The clinician should be aware of these consequences and how to deal with them. Informed consent obtained is a very critical measure to take before starting the treatment, especially in cases with a history of trauma or allergic reactions. Moreover, with all the beneficial effects of orthodontic treatment, it has also a negative effect on the oral and peri-oral structures and social well-being.
LIST OF ABBREVIATIONS
| TMD | = Temporo Mandibular Joint Disease |
| CR | = Centric Relation |
| CO | = Centric Occlusion |
AUTHORS’ CONTRIBUTIONS
The author contributed to conducting this research and writing and editing the final manuscript.
*Saud Alotaibi is the only and corresponding author.
CONSENT FOR PUBLICATION
All the images used in this article were obtained from my patients with their consent.
STANDARDS OF REPORTING
PRISMA- S guidelines were followed for this study.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The corresponding author would like to thank the Deanship of Scientific Research at Majmaah University for supporting this work.


