Differences of Enamel Microhardness Post External Bleaching After Application with Casein Phosphopeptide Amorphous Phosphate (CPP-ACP) and 5% Sodium Fluoride (NAF)
Abstract
Background:
Bleaching is an effort to lighten the color of teeth through the application of chemicals. One of the side effects of bleaching is that it causes demineralization so that the hardness of the enamel will decrease. The hardness of the enamel can be returned back through the mineral laying process, namely remineralization.
Objective:
The purpose of this study was to determine whether there were differences in post-bleaching enamel hardness after Casein Phosphopeptide Amorphous Phosphate (CPP-ACP) or 5% sodium fluoride (NaF) application.
Methods:
In this in-vitro research, bleaching was applied to 30 lower premolars that were divided into three groups, the first group without remineralization, the second group remineralization with CPP-ACP, and the third group remineralization with NAF. Enamel microhardness was measured using Vickers Hardness Tester Machine before bleaching, immediately after bleaching, after application of remineralization pastes, and after 7 days. The teeth were bleached with 40% hydrogen peroxide and underwent remineralization for 7 days.
Results:
The results showed differences in enamel microhardness after using CPP-ACP or 5% sodium fluoride (NaF) application, and the highest post-bleaching enamel hardness was after 5% NaF application. The data were analyzed and tested using ANOVA to measure the differences in hardness between more than 2 groups, and using the post hoc student t-test to measure the differences in violence between the 2 groups. Natural remineralization can occur with saliva but not optimally; therefore, additional remineralizing agents are needed.
Conclusion:
The conclusion of this study was that 5% NaF used as a remineralization agent after in-vitro bleaching could increase enamel microhardness more than CPP-ACP after 7 days of application.
1. INTRODUCTION
Nowadays, public awareness of the importance of dental health is growing higher. Dentists are required to make some-one's smile look attractive, which is synonymous with white and clean teeth. One of the treatments to make teeth look white is bleaching [1, 2]. Bleaching was introduced in the mid-19th century as a non-invasive treatment for teeth whitening. This treatment uses a tooth whitening agent that is rubbed on the surface of the teeth for some time [2].
Bleaching of vital teeth can be done using in-office bleaching and home bleaching techniques. The in-office bleaching technique is performed in dentist's practice and usually uses high concentrations of hydrogen peroxide during a short time period of 20-60 minutes, while the home bleaching technique uses carbamide peroxide with a content of 10-16% (maximum 22%) and is used at night (approximately eight hours) for 2-4 weeks [2].
The effectiveness of hydrogen peroxide as a bleaching agent has been shown to optimally whiten teeth, but it has a negative impact on enamel. Hydrogen peroxide may cause decreased amounts of calcium and phosphate, morphological changes, and decreased enamel hardness [3-7]. Reduction in enamel hardness due to bleaching agents can extend to the inner surface of the enamel, therefore efforts are needed to minimize the potential for damage to the enamel caused by exposure to hydrogen peroxide. One of the efforts to overcome these problems is by applying a remineralizing agent to the tooth surface [8, 9].
Fluor is one of the most frequently used materials to remineralize enamel and has been shown to reduce the incidence of dental caries over the past 25 years. Topical fluoride will form fluorapatite with calcium and phosphate ions, but to configure one unit of fluorapatite [Ca10(PO4)6F2] requires two fluoride ions, ten calcium ions, and six phosphate ions. The availability of calcium and phosphate ions in saliva can be a limiting factor in the remineralization process [9, 10]. This has prompted the emergence of research on new materials that can provide important elements needed for remineralization, those are complex casein phosphopeptide amorphous calcium phosphate (CPP-ACP) and 5% sodium fluoride [10, 11].
CPP-ACP is a complex nano milk protein that is able to remineralize teeth and prevent dental caries [12, 13]. CPP-ACP stabilizes calcium and phosphate ions by forming amorphous nano complexes, releasing calcium and phosphate ions to the pellicle and then diffused into the enamel and dentin [14, 15]. Bayrak (2009) showed that CPP-ACP significantly increased enamel hardness after the application of a bleaching agent using 38% hydrogen peroxide compared to fluoride gel [10, 16]. CPP-ACP increases enamel hardness by depositing calcium and phosphate concentrations in saliva and causes remineralization [14, 17]. The use of CPP-ACP will make the tooth enamel structure stronger for 7 days due to its calcium deposition effect as well as neutralizing the adverse effects on the enamel surface when applied for a week after whitening and minimizing the side effects of the whitening treatment [17].
Sodium Fluoride (NaF) is a fluoride-containing solution that is used topically in dentist clinics. NaF plays a role in preventing demineralization, increasing enamel remineralization, and increasing enamel hardness by forming fluoroapatite, which is an acid-resistant mineral, making it more resistant to caries [11, 15, 18].
Based on research by Da Cunha (2018), the use of high concentrations of fluoride, such as 5% sodium fluoride found in 3M Clinpro White Varnish, after bleaching, can increase enamel strength and reduce enamel roughness without affecting the effectiveness of the bleaching itself [19]. The strength of the enamel is obtained due to its remineralization properties from the tricalcium phosphate content in Clinpro TM 5000 [19]. Clinpro White Varnish contains 50 mg of sodium fluoride (NaF) and based on the research of Hande Kemaloglu (2014), a concentration of 2.1% NaF can reduce the risk of demineralization in post-bleaching teeth [20].
Based on the above background and the controversy regarding the difference in remineralization ability between the two materials, the authors are interested in examining the differences in the increase in enamel hardness after the application of CPP-ACP and 5% sodium fluoride (NaF).
2. MATERIALS AND METHODS
Preparation of enamel specimens thirty extracted, non carious, with no cracks, permanent lower premolar were used in this study. Teeth were cleaned with a scaler to remove any surface debris or contaminants and were stored in 0.9% NaCl solution for 5 minutes at room temperature prior to the experiment.
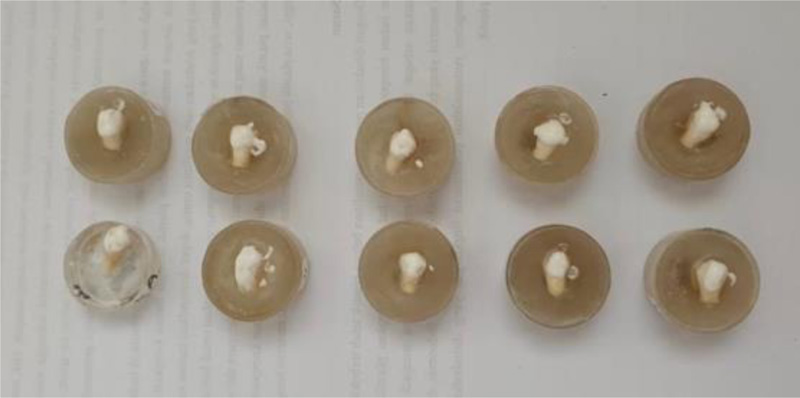
The teeth roots were trimmed to the level of the cementoenamel junction using a carborundum disc. Specimens were randomly divided into three equal groups (n=10), and each specimen was individually embedded in an acrylic resin cylinder with the enamel surface exposed. Enamel surface is leveled and smoothed using a silicon carbide paper grit for the preparation of accurate measurements using the Vickers Hardness Tester Machine shown in Fig. (1).

Treatments – Enamel surfaces were dried with cotton pellets and bleached with 40% Hydrogen Peroxide office bleaching gel (OpalescenceTM BoostTM). A 1-mm layer of gel was applied to the enamel surfaces with a syringe using the nozzle included with the bleaching kit. For optimum effectiveness, bleach was allowed to remain on tooth surfaces for 20 minutes (according to the manufacturer's instructions). The bleaching substance was carefully removed with a soft toothbrush and air-water spray for 10 seconds, and the bleaching procedure was repeated three times during the same day (according to the manufacturer's instructions). Between bleaching treatments, specimens were stored in the artificial saliva in an incubator at room temperature, (Fig. 2).

The treatment regime varied among groups, as follows, group I (n = 10) is a control group, where the teeth were bleached only. In group II (n = 10), the CPP-ACP treatment group, after bleaching, a CPP-ACP paste (GC tooth mousse) was applied to the enamel using an applicator brush. After 3 minutes, the paste was rinsed off with an air-water spray for 10 seconds. CPP-ACP application was repeated daily for 7 days, (Fig. 3) . In group III (n = 10), the Clinpro White Varnish treatment group, after bleaching, a 5% NaF (3M Clinpro White Varnish) was applied to the enamel surfaces using an applicator brush. After 3 minutes, the paste was rinsed off with air-water spray for 10 seconds. The Clinpro White Varnish was applicated only on day 1, (Fig. 4).
Microhardness measurements - Enamel hardness was measured using a Vickers Hardness Testing Machine (VHTM) with a load of 300 g for 15 seconds. For each specimen, three indentations were made on the top surface at a minimum distance of 1 mm from each other and from the specimen margin. Readings of the three indentations were averaged to determine the hardness value for each specimen. The enamel was examined before bleaching, immediately after bleaching, and after the application of CPP-ACP and NaF.
Statistical analysis - One way ANOVA was used to detect any significant differences (P< 0.05) in  VHN among groups. Post-hoc comparisons were made using the independent t-test statistic. Differences between mean enamel microhardness before bleaching and immediately after bleaching were evaluated using paired t-tests.
VHN among groups. Post-hoc comparisons were made using the independent t-test statistic. Differences between mean enamel microhardness before bleaching and immediately after bleaching were evaluated using paired t-tests.

3. RESULTS
Microhardness measurement for the enamel before bleaching is 336,4487 VHN and for the enamel after bleaching is 282,2900 VHN. Table 1 shows the mean value of microhardness changes before and immediately after bleaching.
 VHN).
VHN).| Group |  VHN VHN |
SD |
|---|---|---|
| Before bleaching | 336.4487 | 18.34 |
| Immediately after bleaching | 282.2900 | 16.80 |
| Before bleaching – immediately after bleaching | 54.1587 | 68.3275 |
 VHN between groups paired t-test p-value = 0.0002 (p < 0.05). There are significant differences between the hardness value of the enamel before bleaching and immediately after bleaching. The hardness of enamel immediately after bleaching was lower than before bleaching.
VHN between groups paired t-test p-value = 0.0002 (p < 0.05). There are significant differences between the hardness value of the enamel before bleaching and immediately after bleaching. The hardness of enamel immediately after bleaching was lower than before bleaching.
Microhardness measurement for the enamel after bleaching (Group I) on the first day immediately after bleaching is 258.1 VHN and on the seventh day is 292.6 VHN (Table 2).
 VHN).
VHN).| Group I |  VHN VHN |
SD |
|---|---|---|
| Immediately after bleaching (day 1) | 258.1 | 79.5 |
| After bleaching (day 7) | 292.6 | 47.8 |
 VHN between groups paired t-test p-value = 0.2549 (p > 0.05). There are no significant differences between the hardness value of the enamel immediately after bleaching on the first day and on the seventh day.
VHN between groups paired t-test p-value = 0.2549 (p > 0.05). There are no significant differences between the hardness value of the enamel immediately after bleaching on the first day and on the seventh day.
Baseline microhardness measurements on 30 tooth samples immediately after bleaching ranged from 258.1 VHN (Group I) to 308.8 VHN (Group III). Table 3 shows the mean value of 3 groups' microhardness immediately after bleaching.
 VHN).
VHN).| Group |  VHN VHN |
SD |
|---|---|---|
| Group I | 258.1 | 79.5 |
| Group II | 27.9 | 45.1 |
| Group III | 308.8 | 52.7 |
 VHN between groups ANOVA p-value = 0.1944 (p > 0.05). There are no statistically significant differences in baseline VHN among groups (p > 0.05). The mean hardness value of the 30 samples immediately after bleaching was homogeneous. This homogeneous data means that the initial data of this study are the same so that the final results can be justified.
VHN between groups ANOVA p-value = 0.1944 (p > 0.05). There are no statistically significant differences in baseline VHN among groups (p > 0.05). The mean hardness value of the 30 samples immediately after bleaching was homogeneous. This homogeneous data means that the initial data of this study are the same so that the final results can be justified.
Baseline microhardness measurements on 3 groups samples after remineralization (except on Group I) ranged from 258.1 VHN (Group I) to 353.6 VHN (Group III). Table 4 shows the mean value of 3 groups' microhardness after remineralization.
| Group |  VHN VHN |
SD |
|---|---|---|
| Group I | 258.1 | 79.5 |
| Group II | 340.3 | 47.5 |
| Group III | 353.6 | 41.1 |
 VHN between groups ANOVA p-value = 0.0021 (p < 0.05). There are significant differences in baseline VHN among groups (p < 0.05). Thus, to find out which hardness is best, a further test was carried out using the independent t-test statistic. The results of the independent t-test analysis are shown in Table 5.
VHN between groups ANOVA p-value = 0.0021 (p < 0.05). There are significant differences in baseline VHN among groups (p < 0.05). Thus, to find out which hardness is best, a further test was carried out using the independent t-test statistic. The results of the independent t-test analysis are shown in Table 5.
 VHN VHN |
Group I | Group II | Group III | |
|---|---|---|---|---|
 VHN VHN |
258.1 | 340.3 | 353.6 | |
| Group I | 258.1 | |||
| Group II | 340.3 | 0.0117 | ||
| Group III | 353.6 | 0.0034 | 0.5109 |
From the data, the highest enamel hardness was in Group III (bleaching group + 5% NaF), but it was not significant.
Baseline microhardness measurements on 3 group samples after remineralization (except on Group I) after 7 days ranged from 258.1 VHN (Group I) to 308.8 VHN (Group III). Table 6 shows the mean value of 3 groups microhardness after remineralization after 7 days.
 VHN between groups ANOVA p-value = 0.0004 (p < 0.05). There are significant differences in baseline VHN among groups (p < 0.05). Thus, to find out which hardness is best, a further test was carried out using the independent t-test statistic. The results of the independent t-test analysis are shown in Table 7.
VHN between groups ANOVA p-value = 0.0004 (p < 0.05). There are significant differences in baseline VHN among groups (p < 0.05). Thus, to find out which hardness is best, a further test was carried out using the independent t-test statistic. The results of the independent t-test analysis are shown in Table 7.
| Group |  VHN VHN |
SD |
|---|---|---|
| Group I | 292.6 | 47.8 |
| Group II | 340.3 | 45.0 |
| Group III | 386.5 | 41.1 |
 VHN VHN |
Group I | Group II | Group III | |
|---|---|---|---|---|
 VHN VHN |
292.6 | 340.3 | 386.5 | |
| Group I | 292.6 | |||
| Group II | 340.3 | 0.0381 | ||
| Group III | 386.5 | 0.0002 | 0.0342 |
4. DISCUSSION
Hydrogen peroxide, which is the basic ingredient for bleaching, can cause demineralization because of its acidic nature (pH 5-6), which can dissolve calcium and phosphate from tooth enamel. Demineralization and remineralization have a significant effect on the hardness of enamel. Demineralization will cause the hardness of the enamel to decrease [21, 22]. The chemical reaction of dissolving enamel after bleaching can be seen from the reaction below:
 |
The results of this study were that there was an increase in post-bleaching enamel hardness after 7 days in artificial saliva, but the increase in hardness was very small and insignificant after being analyzed by independent t-test. Natural saliva plays a role in returning calcium and phosphate ions to tooth enamel, so as to create remineralization and prevent demineralization [23, 24].
Saliva plays an important role by neutralizing the acids and providing calcium and phosphate ions to aid in remineralization [25]. Rizvi et al. demonstrated that saliva's mineralization ability is insufficient to deal with dimerization caused by aerated drinks [26].
Several studies state that the effectiveness of saliva is the same as the effectiveness of remineralizing agents in its role in preventing the effects of demineralization after bleaching, but according to Hesmat et al. (2016), additional remineralization materials are needed after bleaching to prevent demineralization and also to increase enamel hardness [24, 27-29].
After seven days, the group remineralized using 5% NaF also showed a significant increase in enamel hardness when compared to those remineralized with CPP-ACP. When viewed from the mean hardness, the 5% NaF treatment group had the highest enamel hardness value on teeth that had been bleached.
Post-bleaching enamel hardness increased significantly after remineralization was carried out using either CPP-ACP or 5% NaF, with the effectiveness of 5% NaF being the highest in increasing enamel hardness. The hardness of the enamel increased significantly on the first day after the application and increased further after the 7th day. The results of this study are in accordance with the research conducted by Ivanoff (2012), which states that remineralization materials with high concentrations of fluor are more effective at restoring enamel hardness compared to CPP-ACP [21].
In this study, a remineralized paste was used topically applied with a high fluor content (22,600 ppm) with Clinpro White Varnish. The Clinpro White Varnish fluor content was greater than the study conducted by Ivanoff (2012), which used a remineralized paste topically applied with a fluor content of 12,300 ppm. This 12,300 ppm fluor was able to increase enamel hardness higher than CPP-ACP.
Another study stated that CPP-ACP was more effective at increasing enamel hardness compared to NaF 250 ppm because of its role as a reservoir for calcium and phosphate in increasing remineralization [10]. The fluor content used in this study was lower than that used in this study containing high concentrations of fluor, while CPP-ACP does not contain fluor.
At the time of demineralization, calcium and phosphate ions will be dissolved. The larger the crystal size of CaF2, the lower the solubility level. With the addition of fluorine, the precipitation of CaF2 crystals will occur. With this deposition, the size of CaF2 crystals becomes larger, thereby increasing resistance to solubility, so that the demineralization effect will be minimized [19]. Apart from having a role in improving enamel morphology, fluor also plays a role in maximizing and maintaining the bleaching effect itself [19, 30].
There are a few limitations; this study was conducted in vitro, and the experimental conditions did not reflect the dynamic conditions of the oral environment. Temperature, pH, saliva chemistry, food interactions, and the presence of microorganisms can all interfere with the remineralization process and bond strength. Because the measurements of the enamel microhardness were only taken for 7 days, longer measurements are required.
CONCLUSION
We can conclude that post-bleaching enamel hardness increased significantly after remineralization was carried out using CPP-ACP, enamel hardness increased from 292.6 VHN to 340.3 VHN. Post-bleaching enamel hardness also increased significantly after remineralization was carried out using 5% NaF, enamel hardness increased from 292.6 VHN to 386.5 VHN. There is a difference in enamel hardness after external bleaching remineralized with Complex Casein Phosphopeptide Amorphous Calcium Phosphate (CPP-ACP) and 5% sodium fluoride (NaF), and 5% NaF increased post-bleaching enamel hardness more than CPP-ACP with the highest increase in enamel hardness on day 7.
LIST OF ABBREVIATIONS
| CPP-ACP | = Complex Casein Phosphopeptide Amorphous Calcium Phosphate |
| NaF | = Sodium fluoride |
| VHTM | = Vickers Hardness Testing Machine |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No humans/animals were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this research are available from the corresponding author [I.I], upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


