All published articles of this journal are available on ScienceDirect.
Effect of Maxillary Expansion Treatment Protocols On Maxillary Sinus Volume, Pharyngeal Airway Volume, and Hyoid Bone Position: A Prospective, Cone Beam Computed Tomography (CBCT) Study
Abstract
Aim:
This study aimed to investigate the changes in maxillary sinus volume, pharyngeal airway volume, and hyoid bone position in patients treated with Rapid Maxillary Expansion (RME) and Alternate Rapid Maxillary Expansion and Constriction (AltRaMEC) – Facemask therapy and compare between the groups.
Materials and Methods:
The records of 15 patients between the age group of 8-14 years with Class I and Class III malocclusion were collected, and the patients were assigned into two groups. The first group comprised of 8patients (4 girls and 4 boys) who were treated with Rapid Maxillary Expansion. The second group comprised 7 patients (5 boys and 2 girls) treated with expansion devices using Alt-RaMEC protocol followed by maxillary protraction using a facemask. Pre and post-treatment CBCT scans were obtained and analyzed for changes in the pharyngeal airway, maxillary sinus volume, and hyoid bone position. The maxillary sinus volume was calculated in 3 dimensions by measuring the craniocaudal height, anteroposterior depth, and mediolateral width. Measurements were taken before and after the procedure to compare the groups and between the groups. The data were analyzed using Paired t-test and an Independent t-test.
Results:
In the RME group, a significant increase in the total maxillary sinus volume (mean difference = 520±576.57mm3), especially in the craniocaudal height, was seen, but no changes were noted in the pharyngeal airway and hyoid position. The AltRAMEC group showed a statistically significant increase in the maxillary sinus volume (anteroposteriorly) and nasopharyngeal volume with a p-value <0.005. Comparing the maxillary sinus volume changes in RME and AltRAMEC groups showed a statistically significant increase in the volume of the maxillary sinuses in both groups, significantly higher in the RME group.
Conclusion:
RME and AltRAMEC protocol followed by facemask therapy caused a significant increase in the maxillary sinus volume, while no changes were noted in the nasopharynx, oropharynx, hypopharynx, and hyoid bone position. While comparing the treatment effects between the groups, RME showed a greater increase in maxillary sinus volume (p < 0.05), specifically in the anteroposterior dimension. Since there are no changes in airway volume and hyoid position with the skeletal expansion protocols, there will be no difference in nasal resistance to airflow.
1. INTRODUCTION
Rapid Maxillary Expansion (RME) occupies a unique forte in Orthodontics, commonly used as a nonsurgical expansion technique for correcting deficient maxillary transverse dimensions [1]. Rigid, fixed RME appliances produce heavy forces that separate the maxillary suture, resulting in maximum skeletal or orthopedic expansion with minimum orthodontic tooth movement [2].
The pharyngeal airway plays a vital role in breathing and swallowing [3] and is essential for cranial and facial bones [4, 5]. Anatomically, it is divided into the nasopharynx, oropharynx, and hypopharynx [3]. Superiorly it is bordered by the base of the skull, by the spine in the posterior region, anteriorly by the mandible and hyoid bone, and anteroposteriorly by the nasal septum [6].
According to Moss’s theory, while breathing, there is a continuous airflow through the nasal cavity, which provides continuous stimulation for lateral maxillary development and lowering of the palatal vault [7].
Assessment of the airway has been an influential diagnostic test in various specialties of dentistry [8], and it has been proven that increased airway resistance contributes to atypical growth of the naso-maxillary complex [9]. Several researchers have promoted RME for dental and rhinological purposes believing that it significantly decreases resistance to nasal airflow.
The growth and development of the sinus are aligned with maxillary structures and posterior maxillary teeth and are therefore affected by any form of skeletal malocclusion [10]. Hence, it can be hypothesized that any intervention correcting malocclusion would affect the maxillary sinus. Research has found that RME causes discernible changes in the maxillary sinus dimensions.
The hyoid bone is a small horseshoe-shaped bone located between the chin and the thyroid cartilage and plays a critical role in chewing, deglutition, speech, and airway patency. It is not articulated directly to any other bone but is connected through various muscles and ligaments to the pharynx, lower jaw, and cranium [11]. Therefore, any alteration in the upper airway dimensions will alter the hyoid bone position and vice versa.
Rapid Palatal Expansion, Functional Regulator(FR III), Protraction face mask, Chin cup etc., are commonly used appliances for the early intervention of treating class III patients. Globally, class III comprises 7% of all the malocclusions, and its frequency of expression differs in various racial/ethnic backgrounds [12]. Despite the low frequency of presentation, class III malocclusion poses one of the most difficult malocclusions to correct in orthodontics. Around 69% of Class III patients are orthognathic cases and require surgical correction [13]. So when the orthopaedic correction of Class III skeletal malocclusions is performed in an earlier stage of life, it can help reduce morbidity and complexity associated with surgical corrections [14]. In an effort to improve the treatment effects and to increase the maxillary prominence in Class III patients, a new orthopaedic treatment protocol was proposed by Eric Liou, which combined alternate rapid maxillary expansion and constriction (Alt-RAMEC) along with maxillary protraction springs [15]. Cephalometric studies have shown that Alt-RAMEC and Rapid maxillary expansion shows similar results [16].
At Children’s Hospital Los Angeles (CHLA), this technique was modified to use the standard orthodontic appliances (Hyrax expander) and reverse headgear [17]. The Alt-RAMEC technique uses a two-hinged expander and intraoral springs for maxillary protraction. The following technique had failures such as anterior open bite and multiple breakages of intraoral springs and the two-hinged expander. Therefore, the intraoral springs and the two-hinged expander were substituted to overcome the failure with a Hyrax expander, Class III elastics, and reverse-pull headgear. Before maxillary protraction, 8 weeks of maxillary sutural loosening were applied with the Hyrax maxillary expander, alternating a week of maxillary expansion with a week of maxillary constriction. The maxillary constriction and/or expansion rate were set at 1 mm/day. This protocol was followed by the full-time wear of Class III elastics and nighttime wear of reverse-pull headgear to protract the maxilla [18].
Studies on the effects of RME on 2D radiographs have shown a decrease in maxillary sinus width [2] and a significant change in the hyoid bone position [19]. Celikoglu et al. [16], in the cephalometric study, reported an increase in airway volume and a change in the vertical position of the hyoid bone following maxillary protraction with Alt- RAMEC. This study evaluated changes in maxillary sinus volume, pharyngeal airway volume, and hyoid bone position in patients treated with two Rapid Maxillary Expansion protocols using Cone Beam Computed Tomography to overcome the limitations of 2D radiography.
2. MATERIALS AND METHODS
This was a prospective, non-randomized study carried out from October 2017- October 2019 in the Department of Orthodontics and Dentofacial Orthopaedics, Manipal College of Dental Sciences, Mangalore, after obtaining approval from the Institutional Ethics Committee (reference number 17117). The study was conducted per the Helsinki declaration guidelines as revised in 2013.
2.1. Sample Size Calculation
The key article [2] shows the expected standard deviation is 548. With an alpha error of 5% and a power of 90%, and keeping an effective difference to show a clinically significant difference of 522, a sample of 12 numbers was required.
Sample size calculation:
2.2. Study Sample
The sample size comprised 15 growing patients, including 8 (4 girls and 4 boys) treated with RME and 7 (5 boys and 2 girls) treated with AltRAMEC protocol followed by facemask therapy. Young adolescent patients between 8-14yrs of age, with unilateral/ bilateral crossbites or with maxilla-mandibular, transverse, and sagittal discrepancies were included in the study. Patients with prior orthodontic/orthopaedic treatment, systemic diseases, craniofacial deformities or TMJ disorders, and those with obstructive airway anomalies were excluded from the study. Subjects in the RME group had a mean age of 12.5±1.3 years, and that of the Alt-RAMEC group was 10.4 ± 1.8 years.
In the RME group, the subjects were treated with a bonded rapid maxillary expander consisting of a hyrax screw (Leone Orthodontic Products, Sesto Fiorentino, Italy) acrylic cap and metal framework (Fig. 1). The activation schedule of the Hyrax screw in the RME group was one turn twice a day (0.25 x 2=0.5 mm/day) until the desired expansion for each patient was achieved.

In the Alt-RAMEC group, the patients were treated with a bonded RME appliance consisting of a hyrax screw (Leone Orthodontic Products, Sesto Fiorentino, Italy), an acrylic cap, and a metal framework with hooks for engaging extraoral elastics.
The activation protocol of the Hyrax screw in the AltRaMEC group was 1 mm per day (2 turns twice a day, 0.5mm x 2 = 1mm) for 1 week; in the succeeding week, the screw was closed with the same rate as the expansion schedule. Following this, the patients were asked to wear a Petit Face mask for maxillary protraction for a minimum of 14 hrs/day. The protraction in the Alt-RaMEC sample was considered completed when a full-cusp Class II molar relationship was achieved to account for relapse.
On average, the total treatment time was 6 months with a retention period of 5 months in Group I and 10 months with a retention period of 3 months in Group II. In both groups, two sets of CBCT images were acquired using Planmeca ProMax 3D Mid CBCT (Planmeca, Helsinki, Finland), one before initializing the treatment (T0) and one after completion of treatment (T1).
The three-dimensional scans were acquired using a CBCT scanner (Planmeca ProMax 3DMid; Planmeca, Helsinki, Finland) at 90kV, 5.6mA and a field of view of 200 mm × 170 mm. The CBCT scan of each patient was acquired with the patient in a standing position and asked to keep their jaws in maximum intercuspation. The CBCT data was stored in DICOM format and was exported to Planmeca Romexis Viewer v.5.2.0 software for further analysis. The 3D reconstruction of the subject’s radiographic data was oriented in the midsagittal plane and adjusted to the skeletal midline of the craniofacial structures, the axial plane was adjusted to show the Frankfort horizontal (FH) plane, and the coronal plane was oriented to pass through the level of the root bifurcation area of the permanent upper 1st molar to make the necessary measurements.
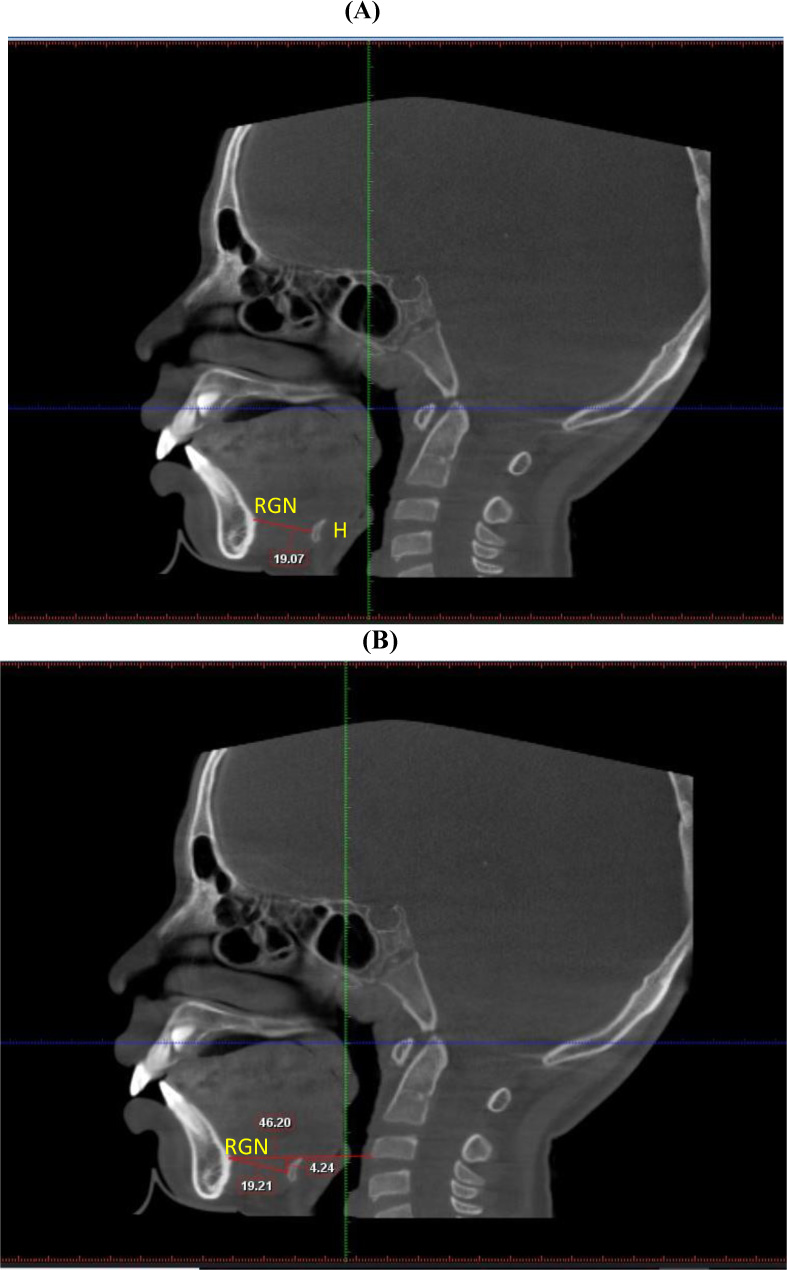
The position of the hyoid bone was assessed using previously reported methods on CBCT images [20]: 1. H-RGN: Horizontal distance amid the hyoid bone & retrognathion (Fig. 2A).
2. H – C3RGN: Vertical line connecting the hyoid bone to the line between points C3 and retrognathion (Fig. 2B).
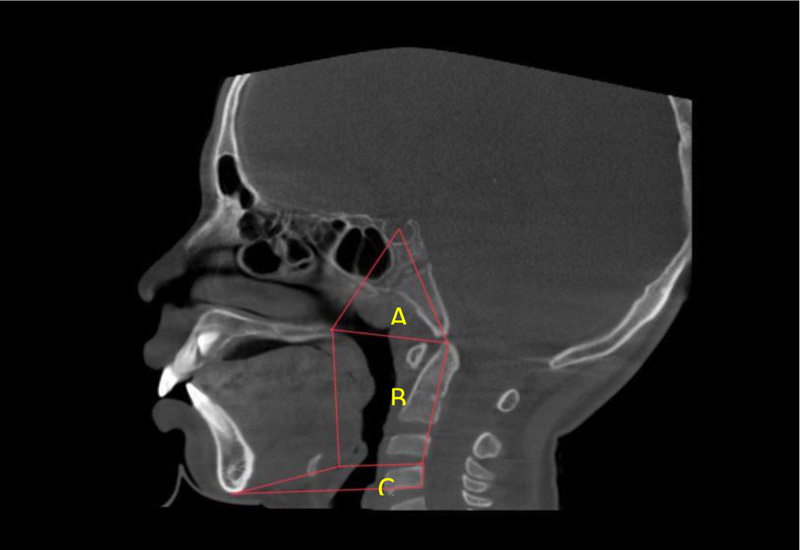
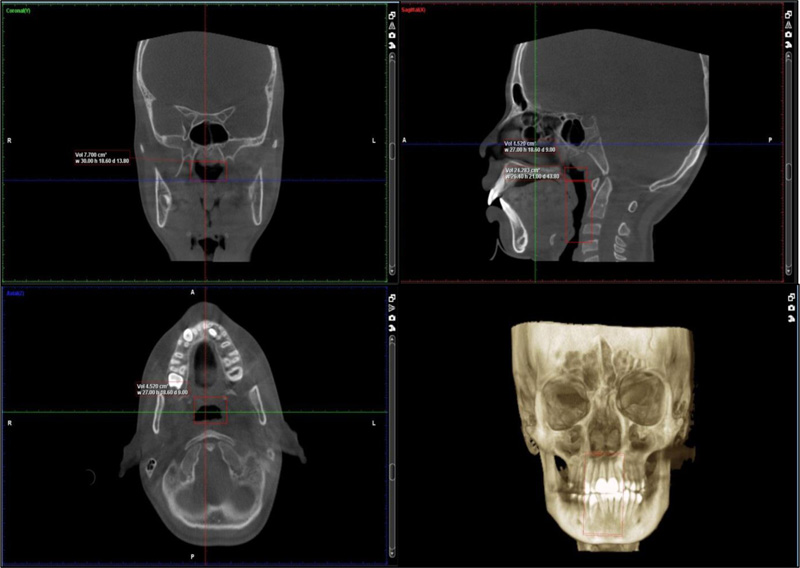
The pharyngeal volume was evaluated considering the landmarks previously reported by Smith et al. [21]. Boundaries of the pharyngeal airway divisions used for volumetric analysis are presented in Fig. (3). The landmarks and boundaries were determined and located on the sagittal section. To analyze the pharyngeal airway, the areas of interest were selected and matched in all 3 views: sagittal, coronal and axial sections (Fig. 4).
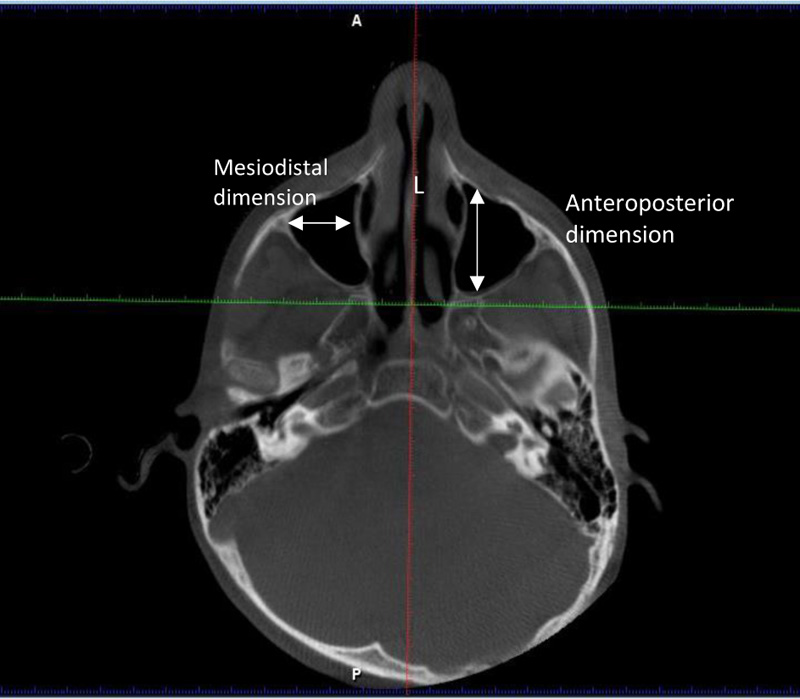
The maxillary sinus volume was measured using the following parameters [24].
Parameters for measuring Maxillary sinus volume [22]
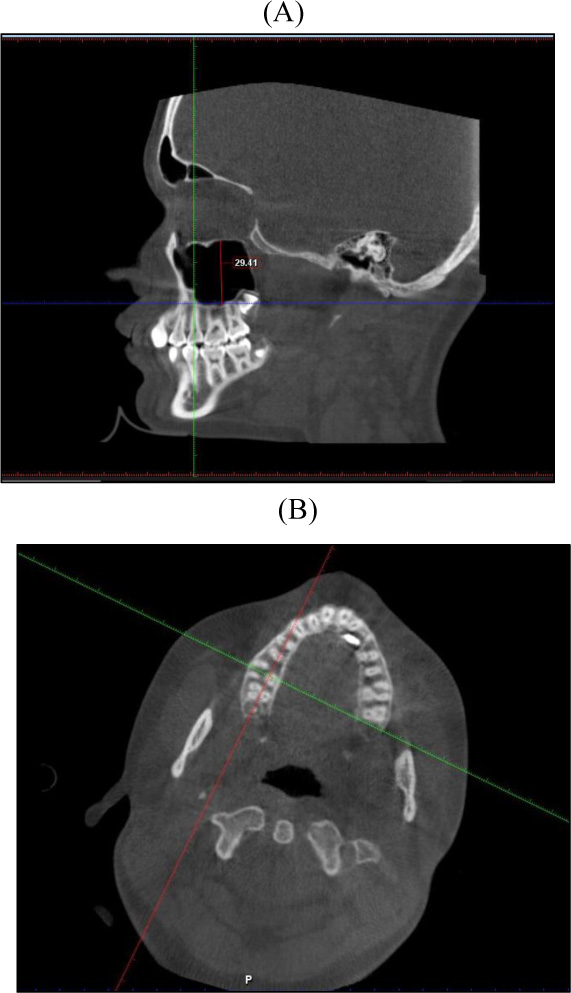
1. Craniocaudal height: The craniocaudal height was assessed by orienting the axial section parallel to the posterior occlusal plane of the upper arch at the level of the alveolar bone crest. The sagittal section was oriented such that it was midway between the buccal and palatal cortices (Fig. 5A). The axial image was rotated and oriented in the coronal section until the sagittal axis was perpendicular to the buccal cortex. The craniocaudal height of the maxillary sinus between the first and second molars was measured from the roof of the sinus to its base, as seen in the sagittal section. (Fig. 5B).
2. Linear measurements of the maxillary sinus width (anteroposterior dimension) and length (medio lateral dimension): These were along the roots of the zygoma on each side. The axial cut's orientation axis was adjusted to precisely pass along the inferior cortical boundary of the zygoma roots on both sides. (Fig. 6) Maxillary sinus volume was calculated using the following geometrical equation: Volume of Pyramid = Base Surface Area × 1/3 Height. Volume of maxillary sinus (Pyramid) = anteroposterior (width) × craniocaudal(height) × mediolateral (length)/3.
2.3. Statistical Analysis
The statistical analyses were performed using the SPSS software package for Windows (version 20.0; SPSS, Chicago, III). The parameters of maxillary sinus volume, pharyngeal airway volume, and hyoid bone position were compared before and after intervention using paired t-test. The Independent t-test was used to compare group 1: Patients treated with RME, and group 2: Patients treated with AltRaME protocol. The level of significance was evaluated at a p-value <0.05. The power of the study was evaluated at 90% with an alpha error of 5%.
3. RESULTS
Evaluation of the pre and post-treatment changes in pharyngeal airway volume, maxillary sinus volume, and hyoid bone position with the RME protocol showed a significant increase in the right maxillary sinus craniocaudal height and right maxillary sinus volume (p=0.011 and p=0.038 respectively). However, no statistically significant difference was observed in pharyngeal airway volumes and hyoid bone position (Table 1).
Comparing pre-treatment and post-treatment AltRAMEC protocols on maxillary sinus volume showed a significant increase in right maxillary sinus craniocaudal height and right maxillary sinus anteroposterior dimension, which subsequently increased the right maxillary sinus total volume (p=0.018). There was a statistically significant increase in left maxillary sinus volume and nasopharyngeal volume by 679.72 and 841.71mm3, respectively (Table 2).
In comparing maxillary sinus volume changes in the RME and AltRAMEC groups, the results showed a statistically significant increase in the volume of the maxillary sinuses in both groups but were significantly higher in the RME group (Table 3).
While comparing the pharyngeal airway volume changes between the groups, the oropharynx showed an increase in the volume in the AltRAMEC group (1503.86mm3), but it was not statistically significant (Table 4). On comparing the posttreatment hyoid bone positional changes between the two groups, the RME group showed a greater difference, but it was statistically insignificant (Table 5).
| - | - | N | Mean ± SD | Mean difference ± SD | t | P VALUE (*p < 0.05) |
| Pair 1 | Right max sinus cc pre | 8 | 23.9±2.27 | -1.51±1.25 | -3.41 | 0.011* |
| Right max sinus cc post | 8 | 25.4±2.21 | ||||
| Pair 2 | Right max sinus md pre | 8 | 23.72±2.22 | -0.45±1.46 | -0.87 | 0.411 |
| Right max sinus md post | 8 | 24.17±1.34 | ||||
| Pair 3 | Right max sinus ap pre | 8 | 33.74±1.01 | -0.73±1.7 | -1.22 | 0.263 |
| Right max sinus ap post | 8 | 34.47±1.39 | ||||
| Pair 4 | Right max sinus total pre | 8 | 6532.42±1039.19 | -520.33±576.57 | -2.55 | 0.038* |
| Right max sinus total post | 8 | 7052.74±755.09 | ||||
| Pair 5 | Left max sinus cc pre | 8 | 24.23±2.27 | -0.79±1.35 | -1.65 | 0.143 |
| Left max sinus cc post | 8 | 25.02±2.39 | ||||
| Pair 6 | Left max sinus md pre | 8 | 23.75±2.35 | -0.5±1.85 | -0.77 | 0.467 |
| Left max sinus md post | 8 | 24.25±1.37 | ||||
| Pair 7 | Left max sinus ap pre | 8 | 33.74±1.1 | -0.8±2.04 | -1.11 | 0.303 |
| Left max sinus ap post | 8 | 34.54±1.67 | ||||
| Pair 8 | Left max sinus total pre | 8 | 6490.28±1042.02 | -480.59±638.06 | -2.13 | 0.071 |
| Left max sinus total post | 8 | 6970.87±680.43 | ||||
| Pair 9 | Nasopharynx pre | 8 | 5426.75±1329.4 | -422.13±715.5 | -1.67 | 0.139 |
| Nasopharynx post | 8 | 5848.88±1676.72 | ||||
| Pair 10 | Oropharynx pre | 8 | 26240.63±7111.21 | -581.5±3634.94 | -0.45 | 0.665 |
| Oropharynx post | 8 | 26822.13±5919 | ||||
| Pair 11 | Hypopharynx pre | 8 | 3167.75±1367.07 | -173.75±1687.2 | -0.29 | 0.779 |
| Hypopharynx post | 8 | 3341.5±1926.98 | ||||
| Pair 12 | H-C3Rgn PRE | 8 | 7.15±3.4 | -0.08±1.22 | -0.19 | 0.853 |
| H-C3Rgn POST | 8 | 7.23±3.85 | ||||
| Pair 13 | H-Rgn PRE | 8 | 33.79±6.82 | -1.01±1.35 | -2.12 | 0.071 |
| H-Rgn POST | 8 | 34.8±5.83 |
Table 2.
| - | - | N | Mean ± SD | Mean difference ± SD | t | P VALUE(*p < 0.05) |
|---|---|---|---|---|---|---|
| Pair 14 | Right max SINUS CC PRE | 7 | 18.97±2.23 | -1.22±0.79 | -4.10 | 0.006* |
| Right max sinus cc post | 7 | 20.19±2.14 | ||||
| Pair 15 | Right max SINUS MD PRE | 7 | 22.57±3.04 | -0.8±1.38 | -1.54 | 0.175 |
| Right max sinus md post | 7 | 23.37±2.83 | ||||
| Pair 16 | Right max SINUS AP PRE | 7 | 30.83±2.35 | -1.71±1.46 | -3.11 | 0.021* |
| Right max sinus ap post | 7 | 32.55±2.17 | ||||
| Pair 17 | Right max SINUS TOTAL PRE | 7 | 4490.99±1237.25 | -701.87±575.01 | -3.23 | 0.018* |
| Right max sinus total post | 7 | 5192.86±1198.36 | ||||
| Pair 18 | Left max SINUS CC PRE | 7 | 19.28±2.69 | -1.14±1.36 | -2.22 | 0.068 |
| Left max sinus cc post | 7 | 20.42±2.3 | ||||
| Pair 19 | Left max SINUS MD PRE | 7 | 22.51±2.72 | -0.81±1.6 | -1.34 | 0.228 |
| Left max sinus md post | 7 | 23.32±2.9 | ||||
| Pair 20 | Left max SINUS AP PRE | 7 | 30.75±2.4 | -1.62±2.22 | -1.93 | 0.102 |
| Left max sinus ap post | 7 | 32.38±2.11 | ||||
| Pair 21 | Left max SINUS TOTAL PRE | 7 | 4536.69±1258.68 | -679.32±551.99 | -3.26 | 0.017* |
| Left max sinus total post | 7 | 5216.01±1234.27 | ||||
| Pair 22 | Nasopharynx pre | 7 | 4907.29±1073.06 | -841.71±677.51 | -3.29 | 0.017* |
| Nasopharynx post | 7 | 5749±1245.61 | ||||
| Pair 23 | Oropharynx pre | 7 | 25446.14±5678.25 | -1503.86±1865.76 | -2.13 | 0.077 |
| Oropharynx post | 7 | 26950±5031.56 | ||||
| Pair 24 | Hypopharynx pre | 7 | 3032.29±817.31 | -748±1000.7 | -1.98 | 0.095 |
| Hypopharynx post | 7 | 3780.29±824.7 | ||||
| Pair 25 | H-C3Rgn PRE | 7 | 4.44±1.87 | 0.56±0.71 | 2.10 | 0.081 |
| H-C3Rgn post | 7 | 3.88±1.88 | ||||
| Pair 26 | H-Rgn PRE | 7 | 31.98±2.92 | -0.98±3.67 | -0.70 | 0.508 |
| H-Rgn POST | 7 | 32.95±2.12 |
| Parameter | RME(mm3) | AltRAMEC | P VALUE(*p < 0.05) |
|---|---|---|---|
| Right max sinus cc post | 25.4±2.21 | 20.19± 2.14 | 0.001* |
| Mean difference ± sd | -1.51±1.25 | -1.22±0.79 | |
| P VALUE | 0.011* | 0.006* | |
| RIGHT MAX SINUS MD POST | 24.17±1.34 | 23.37±2.83 | 0.517 |
| Mean difference ± sd | -0.45±1.46 | -0.8 ±1.38 | |
| P value | 0.411 | 0.175 | |
| Right max sinus ap post | 34.47±1.39 | 32.55±2.17 | 0.058 |
| Mean difference ± sd | -0.73±1.7 | -1.71± 1.46 | |
| P value | 0.263 | 0.021* | |
| Right max sinus total post | 7052.74±755.09 | 5192.86±1198.36 | 0.003* |
| Mean difference ± sd | -520.33±576.57 | -701.87±575.01 | |
| P value | 0.038* | 0.018* | |
| Left max sinus cc post | 25.02±2.39 | 20.42±2.3 | 0.002* |
| Mean difference ± sd | -0.79±1.35 | -1.14±1.36 | |
| P value | 0.143 | 0.068 | |
| Left max sinus md post | 24.25±1.37 | 23.32±2.9 | 0.429 |
| Mean difference ± sd | -0.5±1.85 | -0.81±1.6 | |
| P value | 0.467 | 0.228 | |
| Left max sinus ap post | 34.54±1.67 | 32.38±2.11 | 0.045* |
| Mean difference ± sd | -0.8±2.04 | -1.62±2.22 | |
| P value | 0.303 | 0.102 | |
| LEFT MAX SINUS TOTAL POST | 6970.87±680.43 | 5216.01±1234.27 | 0.004* |
| MEAN DIFFERENCE ± SD | -480.59±638.06 | -679.32±551.99 | |
| P VALUE | 0.071 | 0.017* |
| Parameter | RME(mm3) | AltRAMEC(mm3) | P VALUE(*p < 0.05) |
|---|---|---|---|
| Nasopharynx post | 5848.88±1676.72 | 5749±1245.61 | 0.899 |
| Mean difference ± sd | -422.13±715.5 | -841.71±677.51 | |
| P value | 0.139 | 0.017* | |
| Oropharynx post | 26822.13±5919 | 26950±5031.56 | 0.965 |
| Mean difference ± sd | -581.5±3634.94 | -1503.86±1865.76 | |
| P VALUE | 0.665 | 0.077 | |
| Hypopharynx post | 3341.5±1926.98 | 3780.29±824.7 | 0.571 |
| Mean difference ± SD | -173.75±1687.2 | -748±1000.7 | |
| P value | 0.779 | 0.095 |
| Parameter | RME(mm) | AltRAMEC(mm) |
P VALUE *p < 0.05 |
|---|---|---|---|
| H-C3Rgn POST | 7.23±3.85 | 3.88±1.88 | 0.057 |
| Mean difference ± SD | -0.08±1.22 | 0.56±0.71 | |
| P-value | 0.853 | 0.081 | |
| H-Rgn POST | 34.8±5.83 | 32.95±2.12 | 0.444 |
| Mean difference ± SD | -1.01±1.35 | -0.98±3.67 | |
| P-value | 0.071 | 0.508 |
4. DISCUSSION
The treatment of choice for transverse skeletal discrepancies in pre-pubertal children has been using rapid maxillary expanders. The effect of RME is not just restricted to the correction of a narrow maxillary arch but also extends to contiguous nasal and craniofacial structures. Research has found that RME causes significant changes in the length and size of the maxillary sinus [2]. The effects of RME also extend into the field of otorhinolaryngology because it has been proven to decrease nasal resistance to airflow and increase nasal airway volume, which improves the respiratory efficacy in the individual being treated [23].
Guijarro et al. [24] have reported that Cone-beam computed tomography (CBCT) is an apt and predictable method of determining the airway. Similarly, CBCT is also an accurate method of evaluating the maxillary sinus. Hence, this study evaluated the effects of RME and AltRaMEC on the pharyngeal airway, maxillary sinus volume, and hyoid bone position using CBCT. The power of the study was evaluated at 90%, according to which a minimum of 12 subjects would be needed to satisfy the required power in this study, which was in accordance with Garrett et al. [2].
Cases were selected from a single orthodontist with a sample size of 15 subjects to restrict the intervention to a single observer. The subjects were split into 2 groups: 8 patients were treated with rapid maxillary expansion, and 7 were treated with AltRaMEC protocol and facemask therapy. Since the 2 groups were treated with different treatment protocols for expansion, the mean age between the groups varied slightly. The RME group was 12.5±1.3 years; in the Alt-RAMEC group, it was 10.4 ± 1.8 years. In Group 1 (RME), most patients were above 12 years of age to rule out any developmental changes in maxillary sinus volume, as reported by Schroeder et al. [25]. However, this could not be applied to group 2 patients since the AltRaMEC protocol, and facemask therapy are the treatment of choice in younger patients. The subjects in this study varied in their malocclusion and were treated accordingly. Therefore, the first group of patients belonged to angles’ Class I and Class II skeletal bases, whereas the second group had patients with Class III skeletal bases.
During the selection of patients, considerations were given to exclude oral breathers, patients with the deviated nasal septum, and patients treated with orthodontic treatment. The influences of breathing patterns on craniofacial growth have been described in numerous studies. Agacayak et al. [26] reported a significantly lesser volume of the maxillary sinus in mouth breathers than oral ones. Frankel [27] described a relationship between oral breathing and tongue posture, causing an alteration between the muscles of the hyoid bone leading to an altered position of the hyoid bone. Therefore, patients with habits such as mouth breathing, affecting normal respiration and pharyngeal airway were excluded. In accordance with the data obtained from previous studies [28], it was seen that deviated nasal septum has a significant impact on maxillary sinus volume. Hence, patients with deviated nasal septum were not included in our study.
This study determined the pretreatment and posttreatment effects of two different expansion protocols on maxillary sinus volume, pharyngeal airway volume, and position of the hyoid bone. Smith et al., in their study, found no significant change in the maxillary sinus volume post-expansion. This is contradicted by a study by Garrett et al. that showed a statistically significantly lesser maxillary sinus width. In our study, comparing posttreatment changes of RME, there was a significant increase in the maxillary sinus volume. This could be substantiated by Adkins et al. [29], who found buccal tipping of the molars and lateral movement of the alveolar process with expansion. The lateral movement of the alveolar process might have altered the lower border of the sinuses, which has resulted in a significant increase in maxillary sinus volume expansion
Brown et al. [30] assessed the changes in the oropharyngeal volume in patients treated with RME and showed a significant change in oropharyngeal airway volume. In the present study, we evaluated the airway post-expansion by dividing it into nasopharynx, oropharynx, and hypopharynx, and there were no statistically significant changes in airway volume. This was in accordance with the previous studies [31-33], which also found no effect of RME on pharyngeal airway volume. However, Smith et al., in their study, found that RME increased nasopharyngeal volume. The previous studies have used different landmarks for identification of the pharyngeal airway and alternate software such as Dolphin 3D to evaluate the airway, which could have caused the discrepancy in the findings compared to our findings. Jiang et al. reported a significant correlation between the upper airway dimensions and hyoid bone position. Similarly, our study showed no statistically significant changes in the airway volume and horizontal distance between the hyoid and retrognathion or vertical position of the hyoid bone.
In terms of evaluation of maxillary sinus volume in patients treated with AltRaMEC protocol (including facemask therapy for Class III correction), there was a statistically significant increase in the total maxillary sinus volume. This finding was in accordance with a previous study by Ozbilen et al. [34], which showed that maxillary sinus volume increased in patients treated with AltRaMEC followed by facemask therapy. This difference was attributed to the downward movement of the palatal plane in the Alt-RAMEC group.
In this study, the anteroposterior dimension of the maxillary sinus was also increased significantly. This might be due to the forward movement of the maxilla. As Ozbilen et al. has reported in their study that Alt-RAMEC produced statistically significant forward movement of the maxilla. Liou and Tsai [35] have also reported an increased advancement of A point with the Alt-RAMEC protocol.
On comparing the pharyngeal airway volumes, the nasopharynx showed a significant increase in volume, whereas oropharyngeal and hypopharyngeal volumes had increased but were nonsignificant. The above findings were in accordance with the results reported by Ozbilen et al., who also showed an increase in the upper airway volume again due to the forward movement of the maxilla, whereas no significant change was found in the lower airway volume.
It was seen that there was a dearth of evidence regarding the comparison of the treatment effects of RME and AltRaMEC protocol and facemask therapy on maxillary sinus volume, pharyngeal airway volume, and hyoid bone position. Comparing the craniocaudal heights, anteroposterior dimension, and total maxillary sinus volume between the groups, the RME group showed a higher value and was statistically significant. Increased changes in the maxillary sinus in the RME group could be attributed to the proven effects of RME as stated by Ozibilen et al. However, slight variations can be attributed to the age changes as reported by Lorkiewicz-Muszyńska et al. [36] since the RME group had patients with higher age group (approximately 2years)when compared to that of the AltRaMEC group.
Comparing the volumes of nasopharynx, oropharynx, and hypopharynx between the groups, the RME group showed a higher value except for oropharyngeal volume, which was higher in the AltRaMEC group but was statistically nonsignificant. However, Ozbilen et al. found no difference in pharyngeal airway volume between the RME and Alt-RAMEC groups. In their study, the subjects were treated with RME followed by facemask, while in our study, we had patients treated just with RME. On comparing the linear measurement Hyoid -C3Rgn between the groups, the RME group showed a higher value but was statistically nonsignificant. Comparing the linear measurement of Hyoid Retrognathion between the groups, the RME group showed a higher value and was statistically significant. These findings show a correlation between the pharyngeal airway and hyoid bone position.
CONCLUSION
Based on the observations of the study, the following conclusions were drawn:
1. RME significantly increased the maxillary sinus volume, while no changes were seen in the nasopharynx, oropharynx, hypopharynx, and hyoid bone position.
2. AltRAMEC protocol followed by facemask therapy caused a significant increase in the maxillary sinus volume. No changes were noted in the nasopharynx, oropharynx, hypopharynx, and hyoid bone position.
3. Comparing the treatment effects of RME and AltRaMEC groups, RME showed superior results with a greater increase in maxillary sinus volume, indicating that RME may help craniofacial development. The increase in pharyngeal airway volume was greater in RME compared to AltRaMEC but was not statistically significant. The forward posturing of the hyoid was seen in both groups, but the associated changes were not statistically significant.
LIST OF ABBREVIATION
| RME = | Rapid Maxillary Expansion |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was carried out from October 2017- to October 2019 in the Department of Orthodontics and Dentofacial Orthopaedics, Manipal College of Dental Sciences, Mangalore, after obtaining approval from the Institutional Ethics Committee (reference number 17117).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans used were in accordance with the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
Informed consent was obtained.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the finding of the study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


