All published articles of this journal are available on ScienceDirect.
Antimicrobial agent containing absorbable gelatin sponge to prevent dry socket: A systematic review
Abstract
Background:
The use of absorbable gelatin sponges (AGSs) as a hemostatic surgical material resulted in a reduction of dry sockets occurrence. The systemic use of antibiotics and antimicrobial agents can also reduce the infection of extracted teeth, and therefore, it may show pain-relieving effects on the dry socket as well.
Objective:
Given the high prevalence of dry sockets in the extracted teeth, the main objective of this review was a brief overview of AGSs, including antimicrobial agents to prevent dry sockets.
Methods:
The electronic search of the literature was done on the Pubmed and Google Scholar databases with the MESH keywords of Antimicrobials, Gelatin sponge, Gelfoam, Dry socket, Antibiotics, Alveolar osteitis. Only papers published in English were investigated. No limitations were put on the publication date.
Results:
Of the 279 electronic papers, 79 articles were found relevant to the study. All abstracts were reviewed, and only desired articles were selected. The final electronic and manual search led to 15 articles for use in this study. Among these studies, 5 studies were related to AGSs, including antimicrobial agents to prevent dry sockets.
Conclusion:
The reviewed literature showed that the systemic/topical use of antibiotics and antimicrobial agents can reduce infection and, therefore, may show pain-relieving effects on the dry socket. Besides, antimicrobial-loaded AGSs can be helpful in curing or preventing dry sockets. There were a limited number of clinical trials that used antimicrobial loaded AGSs for dry socket. More clinical studies are needed, especially in subgroups of patients with a high risk of infectious conditions, to validate the effectiveness of antimicrobial-loaded AGSs for dry socket.
1. INTRODUCTION
Given the high prevalence of dry socket following dental extraction, many researchers have tried to find successful methods to prevent its occurrence [1-5]. The term was first titled in scientific papers in 1896, and since then, it has been called by other words such as alveolitis, alveolar osteitis and, localized osteitis [6, 7]. This complication is one of the major problems after tooth extraction, especially after the removal of the mandibular third molar. In various scientific texts, the prevalence of dry socket after extraction of teeth has been reported to be 5% and while in the lower third molar is about 37% [8]. The main etiology of this complication is still unclear, and it can be affected by many factors, including surgical trauma, lack of dentist's clinical experience, systemic diseases such as diabetes, oral contraceptive use, gender, tobacco consumption, bacterial infection, single tooth extraction, local anesthesia with a vasoconstrictor and not using suture [6-10]. There are some comprehensive reviews about the suggested reasons for dry socket, and the factors that increase dry socket [11-15]. One main hypothesis is that the presence of bacteria may initiate dry socket or extend its period [16-19].
The prevention techniques include avoiding tobacco consumption before and after the surgery. Referring to a dentist or oral surgeon with experience in tooth extractions is also another technique to reduce the occurrence of dry socket [20]. There are some evidence showing that antibiotic administration after tooth extraction decreases dry socket occurrence [21-23]. A meta-analysis also showed that systemic administration of antibiotics before tooth extraction reduced dry socket occurrence [24]. The use of azithromycin can be considered in the reduction of dry socket incidence [20]. The experiences of dentists have also shown that by rinsing with mouthwash and reducing the bacterial flora in the oral cavity, the incidence of dry sockets can be reduced. Numerous studies have shown that the usage of CHX mouthwash before or after surgical treatment of the third mandibular molar significantly decreases the incidence of the dry socket [25-27]. Besides, the systemic use of antibiotics and antimicrobial agents can reduce infection [28-32]. Therefore, it may show pain-relieving effects on dry socket as well [33]. Topical use of CHX or antibiotics has also been used inside the extracted tooth socket, but in some cases, they may show negative effects and may lead to severe reactions [34].
Absorbable gelatin sponges (AGSs) are known as a surgical material, planned for application to bleeding surfaces as a hemostatic [35-37]. Some reports have shown that the use of an absorbable gelatin sponge (AGS) resulted in a decrease in the incidence of dry sockets within the extracted tooth due to the retention of the clot by the gelatin sponge in the extracted tooth [38, 39]. Reports also demonstrated that the occurrence of dry socket substantially decreased with the gelatin sponge, including antimicrobial agents [40]. Then, this review has focused on AGSs, including antimicrobial agents to cure or prevent dry socket.
2. MATERIALS AND METHODS
The electronic search of the literature was done based on title and abstract searching on the ‘Pubmed and Google Scholar’ databases with the MESH keywords of Antimicrobials, Gelatin sponge, Gel-foam, Dry socket, Antibiotic, Alveolar osteitis. Only available published English papers performed by valid procedures were selected. No limitations were put on the date.
A complete procedure was used for this review in which the analysis and eligibility criteria were stated according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [41]. In this study, Population, Intervention, Comparison, Outcomes and Study design (PICOS) criteria were considered as itemized below:
a) Population: All individuals of any age and gender who had undergone any tooth extraction with any degree of dry socket, regardless of the type of treatment received.
b) Intervention: The studies that assessed the efficacy of any type of administered antibiotics/antimicrobials at any dose, formulation (including antimicrobial loaded gelfoams), or regimen, and regarding comparisons.
c) Comparisons: Treatment of dry socket with commonly used methods.
d) Outcome: Reduction or treatment of dry socket.
e) Study design: All experimental/clinical studies were performed by valid procedures.
The collected data were analyzed by the authors independently.
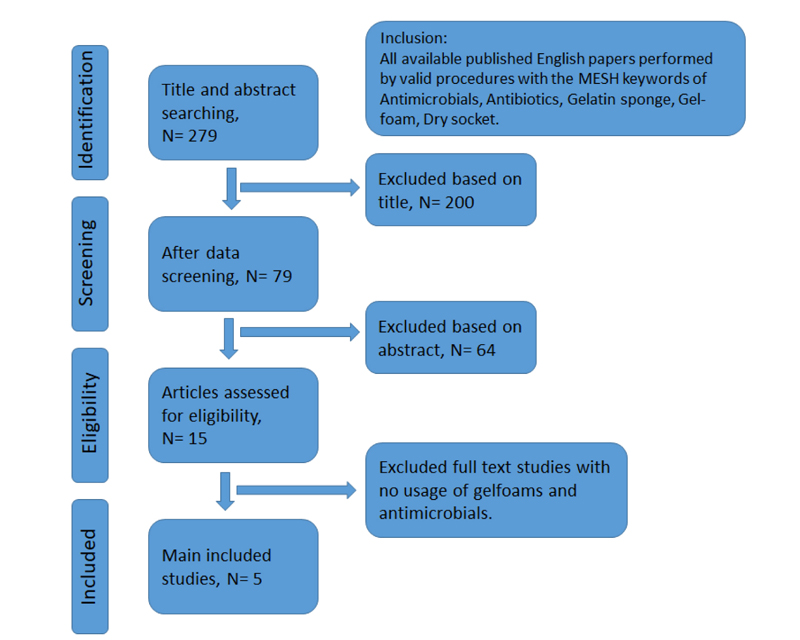
After title and abstract searching, data screening was performed. The papers was excluded according to the title and abstract reading. Then, the full text of papers were read and the papers with no usage of AGSs and antimicrobials were excluded. Inclusion and exclusion criteria and study flow for the review were shown in (Fig. 1).
3. RESULTS
Of the 279 electronic search results, 79 articles were deemed relevant to the current study. All abstracts were reviewed, and only needed articles were obtained. The final electronic and manual search resulted in 15 research articles for use in this study. Among these studies, the descriptive analysis was done for 5 studies related to the use of AGSs, including antimicrobial agents to prevent dry socket. Table 1 shows the details of 5 research articles matched by using the criteria for this review.
4. DISCUSSION
The search results showed that the use of CHX as a mouthwash and as a rinse before gingival surgery has shown a significant reduction in the amount of oral microbial populations [45]. A 50% decrease in the prevalence of dry socket was observed in patients who experienced 12.12% of CHX solution for 30 seconds. The use of 0.2% CHX biochemical gel decreased the incidence of dry socket compared to the 0.2% CHX mouthwash, and no adverse effects were observed [25, 26]. The use of 0.12% CHX for two weeks postoperatively reduces the incidence of dry socket [26].
The search results also showed that systemic use of antibiotics and antimicrobial agents can reduce the infection of extracted teeth [28, 31, 32]; therefore, it may show pain-relieving effects on the dry socket as well [33]. For example, Sanchis et al. used systemic tetracycline to reduce the incidence of dry sockets and demonstrated that systemic tetracycline showed good effects in reducing the incidence of the dry socket [33]. In a similar study, Shanghai et al. found that systemic metronidazole was effective in decreasing the occurrence of the dry socket [46]. Rood et al. reported a significant decrease in the incidence of the dry socket with systemic metronidazole administration as well [34]. However, systemic antibiotics can also have various side effects that need to be considered.
| Tested Material | The Method | The Main Results | Refs. |
|---|---|---|---|
| AGS (Gelatamp; roeko, Langenau, Germany) including 0.2% CHX | The efficacy of intra-alveolar AGS containing 0.2% CHX in preventing dry socket and postsurgical pain intensity on 80 randomly selected sockets of a total of 160 impacted mandibular third molars. | • The occurrence of dry socket substantially decreased with the use of CHX containing AGS from 32.6% to 11.3% (P ≤ .001). • Moreover, it led to a significant decrease in postoperative pain of all the patients (P ≤ .001). |
[40] |
| AGS (Gelfoam; Pharmacia&Upjohn Comp., Kalamazoo, Michigan, USA) saturated with sterile lincomycin solution | The efficacy of lincomycin-loaded AGS for dry socket under controlled, double-blind conditions in subjects who had undergone extraction of impacted mandibular third molars. | • The lincomycin-loaded AGS reduced the incidence of the dry socket to acceptable levels. | [42] |
| AGS (Gelfoam; Pharmacia&Upjohn Comp., Kalamazoo, Michigan, USA) or SaliCept patches (Carrington Laboratories, Irving, Texas, USA) containing acemannan | The incidence of dry socket in patients treated with either clindamycin-soaked AGS or SaliCept patches containing acemannan were tested on 607 patients (1,064 sockets). | • The incidence of dry socket was decreased in both groups. In the AGS group, 78 of 975 sites (8.0%) developed dry socket, while in the SaliCept-treated group, the percentage was only 1.1% (11 of 958 sites) | [43] |
| Ciprofloxacin/AGS (Gelfoam; Pfizer, New York City, New York, USA); group 6, Double-antibiotic-paste/AGS (Gelfoam; Pfizer, New York City, New York, USA); and group 7, Modified triantibiotic-paste/AGS (Gelfoam; Pfizer, New York City, New York, USA). | The revascularisation effect of necrotic mature teeth was examined in a dog model. Periapical infection was persuaded in 54 mature premolars. | • The results demonstrated that double-antibiotic paste/AGS and Ciprofloxacin/AGS exhibited efficient vascularity, cementum formation, corono-apical tissue ingrowth, and lower inflammatory intensity (P < 0.05). | [44] |
| AGS contains 5% tetracycline and 0.001% hydrocortisone | A comparative clinical study of the surgical removal of 200 impacted mandibular third molars was done to find the incidence of dry socket, pain and trismus. | • The patients who were administered intra-alveolar tetracycline had less pain and trismus and consumed fewer analgesics than the patients who received no such treatment. | [33] |
Topical use of CHX or antibiotics has also been used inside the extracted tooth socket [34]. Haraji et al. evaluated the effect of age, the surgery method, and CHX topical gel application on dry socket risk. The extraction socket treatment was classified into standard and experimental as a primary predictor variable. The patients were randomly selected; each had 1 third molar, and was packed with 0.2% CHX gel as an experimental treatment. The contralateral third molar was considered as the control socket and treated in the usual manner. On postoperative day 3, the primary outcome variable was dry socket status, recorded as present or absent. According to the Pederson scale, the other study variables were set as tobacco consumption, demographic, and surgical difficulty. Appropriate bivariate and multiple logistic regression analyses were utilized to determine the relationship between dry socket risk and CHX gel application, tobacco consumption, gender, age, surgical difficulty, and their interactions. The samples were composed of 90 bilateral extraction sockets among 45 patients (24 men; 21 smokers). According to the progression analysis, the use of CHX gel reduced the risk of the dry socket when other factors and their interactions were controlled (P = 0.004). Higher age (P = 0.030) was associated with an increased chance of dry socket. A similar relationship was also observed between increased level of extraction difficulty and dry socket risk (P = 0.051). Tobacco consumption did not show a significant effect (P = 0.4), whereas the effect of gender was significant (P = 0.091) [47]. In another study, tranexamic acid, as a medication to prevent heavy bleeding, was also applied to prevent bleeding, but it did not reduce the incidence of the dry socket [48]. The topical usage of a mixture of hydrocortisone and tetracycline oxide significantly reduces the incidence of dry socket after removal of the impacted mandibular third molar teeth [49].
Some reports have shown that the use of AGSs resulted in a decrease in the incidence of dry sockets within the extracted tooth due to the retention of the clot by gelatin in the extracted tooth [38, 39]. Ghavimi and his colleagues studied the use of AGS (Gelatamp; Coltene/Whaledent, Langenau, Germany) in preventing the treatment of dry sockets. According to their results, the assumption of a possible decrease in the incidence of dry sockets within the extracted tooth can be explained by the retention of the clot by the AGSs in the extracted tooth. Their results showed that the prevalence of dry socket in the experimental group was lower than the control group (2 vs. 7) [50].
Reports also demonstrated that the occurrence of dry socket substantially decreased with the AGSs, including antimicrobial agents [35]. The efficacy of intra-alveolar AGS (Gelatamp; roeko, Langenau, Germany) included 0.2% CHX in preventing dry socket, and postsurgical pain intensity on 80 randomly selected sockets of a total of 160 impacted mandibular third molars was examined in recent work by Haraji et al. at the first and third postoperative days. The contralateral socket was packed with a dry dressing as the placebo. The resulting data demonstrated that the occurrence of dry socket substantially decreased with the use of CHX containing AGS from 32.6% to 11.3% (P ≤ .001). Moreover, it led to a significant decrease in postoperative pain of all the patients (P ≤ .001) [40]. Goldman et al. also used AGS (Gelfoam; Pharmacia&Upjohn Comp., Kalamazoo, Michigan, USA) saturated with sterile lincomycin solution for dry socket under controlled, double-blind conditions. Their results revealed that lincomycin-loaded AGS reduced the incidence of the dry socket to acceptable levels in subjects who had undergone extraction of impacted mandibular third molars. The occurrence of dry socket was reduced to 1.1 percent in the patients who received topical lincomycin-loaded AGS, as compared to 7.8 percent when the AGS contained saline solution instead of lincomycin [42]. In a research done by Poor et al., they compared the incidence of dry socket in patients treated with either clindamycin-soaked AGS (Gelfoam; Pharmacia&Upjohn Comp., Kalamazoo, Michigan, USA) or SaliCept patches (Carrington Laboratories, Irving, Texas, USA) containing acemannan (an herbal antimicrobial agent from Aloe vera). The test was done on 587 patients (1,031 sockets) with clindamycin-soaked AGS and a trial in which 607 patients (1,064 sockets) had 2 SaliCept patches placed immediately after extraction. All patients were treated by the same surgeon. Analysis of all extraction sites revealed that the incidence of dry socket was decreased in both groups. In the AGS group, 78 of 975 sites (8.0%) developed dry socket, while in the SaliCept- acemannan group, the percentage was only 1.1% (11 of 958 sites) [43]. In another work conducted by Fahmy et al., the revascularisation effect of necrotic mature teeth was examined in a dog model. Periapical infection was persuaded in 54 mature premolars. The samples were divided into 7 groups: group 1, double-antibiotic paste/blood clot; group 2, ciprofloxacin/collagen; group 3, double antibiotic paste/collagen; group 4, modified tri-antibiotic paste/collagen; group 5, Ciprofloxacin/AGS (Gelfoam; Pfizer, New York City, New York, USA); group 6, Double-antibiotic-paste/AGS (Gelfoam; Pfizer, New York City, New York, USA); and group 7, Modified triantibiotic-paste/AGS (Gelfoam; Pfizer, New York City, New York, USA). The healthy and infected teeth were considered negative and positive control groups, respectively (n=12 roots/group). The results demonstrated that the double-antibiotic paste/collagen and ciprofloxacin AGS exhibited efficient vascularity, cementum formation, corono-apical tissue ingrowth, and lower inflammatory intensity (P < 0.05). On the other hand, these groups exhibited increased levels of vimentin (P < 0.05). All groups showed connective tissue similar to the structure observed in bone and cementum and decreased inflammation in necrotic mature teeth with chronic apical periodontitis [44]. In another report, a comparative clinical study of the surgical removal of 200 impacted mandibular third molars was done to find the incidence of dry socket, pain and trismus. The dressing contains 5% tetracycline and 0.001% hydrocortisone-absorbable gelatin sponge, immersed in semiliquid gypsum powder and then compressed slightly and packed in a socket. The patients who were administered intra-alveolar tetracycline had less pain and trismus (without a significant effect on dry sockets) and consumed fewer analgesics than the patients who received no such treatment [33].
CONCLUSION
In this review, we concentrated on absorbable gelatin sponges, including antimicrobial agents, to cure or prevent dry socket. The reviewed papers revealed that using antimicrobial-loaded absorbable gelatin sponges can be helpful in curing or preventing dry sockets. Then, more clinical studies are needed to validate the effectiveness of antimicrobial-loaded absorbable gelatin sponges for different conditions, especially for dry socket.
THE LIMITATIONS OF THE STUDY
There were a limited number of clinical trials that used antimicrobial-loaded absorbable gelatin sponges for dry socket. More studies are needed in this regard, especially in subgroups of patients with a high risk of infectious conditions, in which preventive antimicrobial-loaded absorbable gelatin sponges may be more beneficial than in healthy patients.
LIST OF ABBREVIATIONS
| AGSs | = Absorbable Gelatin Sponges |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Met-Analysis |
AUTHORS' CONTRIBUTIONS
SHS, SS, SS, MG, AG and RN had contributions to the drafting of the manuscript. SHS, MG contributed equally to this work and should be considered co-first authors. SM, SS, and MG had a contribution to the revision of the manuscript. All authors read the final version of the manuscript and accepted it.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The raw/processed data required to reproduce these findings can be shared at this time.
FUNDING
The Vice Chancellor for Research at Tabriz University of Medical Sciences provided financial support.
CONFLICT OF INTEREST
Solmaz Maleki Dizaj and Simin Sharifi are the Editorial Board Members of the The Open Dentistry Journal.
ACKNOWLEDGEMENTS
This article was written based on a dataset from a thesis registered at Tabriz University of Medical Sciences, Faculty of Dentistry and Dental and Periodontal Research Center (number 63468). The thesis was supported by the Vice-Chancellor for Research at Tabriz University of Medical Sciences.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


