All published articles of this journal are available on ScienceDirect.
Transbuccal vs. Intraoral Approach using an Angulated Screwdriver in Fixation of a Mandibular Angle Fracture
Abstract
Objectives:
This study aimed to evaluate surgical stability and cosmetic outcomes in patients with mandibular angle fractures (MAFs) using an angled screwdriver (ASD) versus transbuccal trocar (TBT) for single locking plate fixation.
Methods:
A prospective cohort clinical study was done on 44 male patients (88%) and 6 (12% females patients with MAFs, categorized into 2 groups. Group A patients were treated with strictly intraoral vestibular incision using an angulated screwdriver; group B was treated with TBT. Both groups placed a single locking 2.0 mm mini-plates at the inferior border. The main outcome variables were the perioperative complication rate.
Results:
There were no statistical differences between both groups regarding postoperative wound dehiscence, screw or/and plate looseness, infection rate, and inferior dental nerve injury. The study (ASD) approach took 28.10±3.3minutes, while the TBT approach took 37.40±1.75minutes, indicating a highly significant difference in operating time (P=0.001). Post-operative edema had decreased significantly in the ASD group.
Conclusion:
According to the present results, a strictly intraoral approach for ASD enabled stable fixation of MAFs using a single mini-locking plate. This can significantly reduce operation time and postoperative edema and prevent extraoral scarring.
1. INTRODUCTION
Mandibular fractures account for a considerable percentage (20-30%) [1] of all maxillofacial injuries due to their exposed location within the facial skeleton, as well as the fact that it is the most common target of interpersonal assault [2, 3]. Since mandibular angle fractures (MAFs) are biomechanically complex and have a high complication rate, treatment is challenging and unpredictable [1, 4, 5]. Open reduction and internal fixation (ORIF) are usually indicated to treat MAFs [6, 7]. Champy et al. defined applying a single small plate to the ideal line of osteosynthesis; as being adequate to withstand the forces that the mandibular bone is frequently subjected to [3, 8]. Others prefer to use heavier plates at the mandible's inferior border to counteract displacement forces, especially in unfavorable fracture types [9].
Transoral or extraoral skin incisions could be used to gain surgical access to the MAFs [10-12]. In many other cases, a transoral approach with heavy plates at the inferior border necessitates using a TBT through a small incision on the opposite side [1, 6]. The intraoral approach of the condylar fractures fixation [13, 14] was attempted in our department. However, its usage for angle fractures, particularly during fixation of the most posteriorly plate screws, was more successful than the outcomes of condylar fractures [6, 8]. These methods typically provide adequate access and visualisation of the operative field; however, they vary in terms of simplicity, access time, aesthetic outcomes, and the frequency of associated complications [9, 15]. Regarding fracture fixation stability, proper intraoperative vision, postoperative scarring, infection, and good aesthetic results, the benefits of these two approaches, the TBT approach versus angulated screwdrivers, should be evaluated.
There was no clinical investigation comparing the strictly intraoral approach using an angulated screwdriver in fixating MAFs with the TBT approach via small facial skin incision using TBT in respect of postoperative complications and visibility of the facial scar. Therefore, the authors conducted this clinical study to compare the intraoral alone approach using an angulated screwdriver in fixation of MAFs and the TBT approach considering postoperative complications, time of surgery and visibility of the scar.
2. PATIENTS AND METHODS
2.1. Study Population and Design
This clinical study recruited patients who had suffered from MAFs indicated for ORIF. Between April 2018 and January 2021, these were chosen from the Department of OMS, Al-Azhar University's outpatient clinics. Sample size calculated via open Epi software. On the day of surgery, a simple random allocation procedure was utilised with a computer software application that generates a random sequence to divide the patients into two groups. The transoral procedure, which involves an intraoral vestibular incision, was used in group 1 to treat MAFS. The angulated screwdriver device was used to secure the single locking 2.0mm plate. In group 2, an intraoral incision, a small facial skin incision, and a small facial skin incision were made, allowing TBT to be used to pass the drill and screwdriver through for the fixation of a single locking plate at the mandible's inferior border. All patients provided written informed consent per the Helsinki Declaration, and the local ethics review committee approved the study of Al-Azhar University's Faculty of Dental Medicine for Girls.
2.2. Inclusion and Exclusion Criteria
The study included patients who fulfilled the following inclusion criteria: (1) patients with unilateral unfavorable MAFs indicated for ORIF; (2) fractures lasting more than 7 days; (4) patients' age ranging from 17 to 60; (5) No history of chemotherapy or radiation therapy; and (6) absence of systemic diseases that could affect the bone healing. The patients were not allowed to participate in the present study for one of the following reasons: Patients who were medically compromised; patients who had pan facial fractures; edentulous cases; patients who had angle fractures suggested for Champy superior border technique; and patients who were declined to participate in the research.
2.3. Study Variables
The surgical approach and fixation screwdriver were the key predictor variables. Complications following treatment were the key outcome variables. Complications included screw or plate fracturing or loosening, wound dehiscence or exposure of fixation plates, signs/symptoms of infection, malunion or/and nonunion of segments, and the need for plate/screw removal, and facial scarring. A junior staff member also kept track of the surgical time from the incision to the reduction and fixation of the MAFs. The time spent reducing and repairing the other comminuted fractures was not included in the estimation of the surgical time.
2.4. Data Collection
In each patient's medical chart, the following information was recorded: name, gender, and age, medical and dental history, etiology of fracture, intraoral abrasions, laceration, ecchymosis, hematoma or swelling in the mandibular angle region, pain and tenderness to palpation over the angular fracture, preoperative malocclusion, time interval between the fracture occurrence and treatment, surgical approach used (transoral combined with TBT or transoral only), postoperative fracture stability (based on manual palpation).
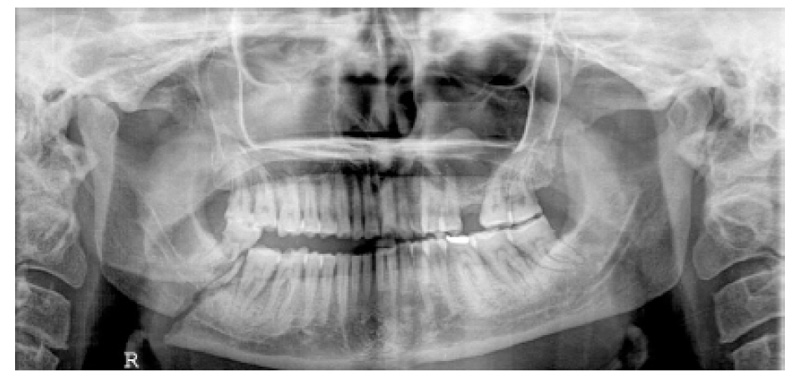
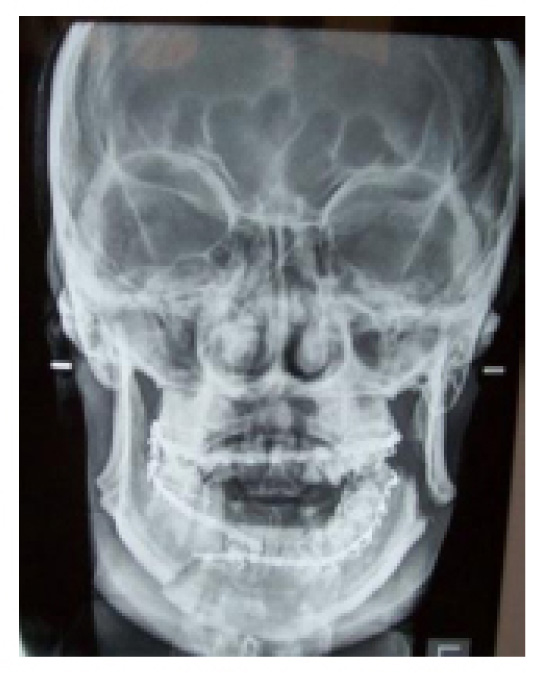
The main outcome variables were the perioperative complication rate which included postoperative wound dehiscence, screw or/and plate looseness, infection rate and inferior dental nerve injury, mouth opening, and the degree of external scar in the TBT group and all potential complications following treatment. Preoperative and postoperative evaluation for all patients included panoramic x-ray posters, anterior views, or CT scans to determine the number of fractures, their site, and the direction of fracture lines (Figs. 1, 2).
2.5. Surgical Procedures
All procedures were done with nasotracheal intubation, and general anesthesia. 2 percent mepivacaine with 1:200,000 epinephrine was injected through the incision line to ensure sufficient hemostasis. The same surgical team conducted all medical procedures in a standardized manner. The fractured segments were immobilized with arch bars and 0.5 stainless steel wires for proper occlusion, and if the occlusion was not ideal, the fractured segments were manipulated after the fracture line was exposed. A mandibular vestibular intraoral incision extending from the premolar region to the third molar area was used in both groups.
A tooth would have to be removed if it was fractured in the fractured line, had excessive movement, or interfered with the reduction process. Aside from that, the tooth would be reduced rather than removed.
A 2mm locking miniplate inserted at the inferior border of the MAFs was secured with six bicortical 2-mm diameter screws. Two angulated handpieces (SCREWDRIVER 90º, SYNTHES) were used in the study to simplify the operation and save time; a 1.5 drill bit was connected to one angulated handpiece for drilling, and another was used as a screwdriver (Fig. 3). The first screw hole was drilled through the proximal segment with the angulated drill of the angular handpiece, and the first screw was secured to another angulated screwdriver before being inserted into its bed.
The first screw was not tightened until the second screw on the opposite side of the fracture was fully placed to prevent the plate from moving into an undesirable location; the fracture reduction was enabled by pulling the plate. The second screw was inserted in the distal segment via one of the holes in the locking mini-plate, and the remaining screws were inserted. However, in the TBT approach group, angular fractures were reduced and fixed using a TBT to allow a conventional cross-shaped screwdriver and drills to be passed through it; to allow for perpendicular screw insertion.
IMF was removed from both groups, and the occlusion and mandibular movement were tested for any inconsistencies in the opening, closing, and occlusion. The wound was reexamined for any bleeding points to maintain homeostasis. The incision sites were irrigated, and 3–0 absorbable interrupted Vicryl was used to close them. No drains were placed. All other patients with associated fractures were treated via double 2.0-mm mini-plates. After surgery, all patients followed a soft diet for four weeks and took oral antibiotics for seven days.

2.6. Statistical analysis
To summarize the demographic postoperative measurement results, the means, SD, range, and percentages were determined. The Pearson's Chi-Squares test was used to compare groups and analyze the key outcome variables changes in both groups. A statistically significant P-value of less than 0.05 was used. SPSS version 16 was used to perform all statistical calculations (SPSS Inc., Chicago, IL, USA).
3. RESULTS
A total of 50 patients composed the patient population, 44 (88%) males and 6 (12%) females with a male-to-female ratio of 7.3:1. At the time of surgery, the patients' ages ranged from 17 to 40 years old (mean 26.3±6.9years). Within one week of trauma, all patients underwent surgery.
Road traffic accidents (RTA) were the most common cause of fracture in 28 (56%) patients, followed by interpersonal violence (IPV) in 16(32%) patients and falls in 6(12%) cases. Just 19 (38%) had single angle fractures, 18 (36%) patients had concomitant parasymphyseal fractures, 9 (18%) patients had ipsilateral body and condylar fractures, and 2 (4%) patients had contralateral condylar fractures (Table 1).
| Study variables No/(%) | Categorial variables | Group A | Group B | P value |
|---|---|---|---|---|
| Gender: | ● Male 44 (88%) ● Female 6(12%) |
21 (42%) 4 (8%) |
23 (46%) 2 (4%) |
0.3 |
|
Age (years): 26.3±6.9 |
● Mean± SD (26.6±7.3) ● Range (17-40) |
25.40 ±7.20 17-40 |
27.80±7.50 18-40 |
0.1 |
| Etiology: | ● Fall (6/12%) ● RTA (28//56%) ● IPV (16/32%) |
6 (12%) 13 (26%) 6 (12%) |
0 (0%) 15 (30%) 10 (20%) |
0.2 |
| Affected side: | ● Right (38/76%) ● Left (12/24%) |
18 (36%) 7 (14%) |
20 (40%) 5 (10%) |
0.5 |
| Concomitant mandibular fractures | ● Isolated angle 19 (38%) ● Parasymphyseal 18 (36%) ● Ipselateral body and condylar 9 (18%) ● Contralateral condylar 2 (4%) ● Midface 2 (4%) |
12 (24%) 6 (12%) 5 (10%) 2 (4%) 0 (0%) |
7 (14%) 12 (24%) 4 (8%) 0 (0%) 2 (4%) |
0.1 |
| Preoperative NAMO in mm: 23.3±5.0 | ● Mean± SD ● Range |
22.8± 4.7 16-30 |
23.7±5.3 15-31 |
0.5 |
| Preoperative AMO in mm: 26.9±4.8 | ● Mean± SD ● Range |
28.5± 21-32 |
27.10± 18-35 |
0.60 |
3.1. Duration of Surgery
The angle fractures were adequately exposed through the intraoral vestibular incisions. Five of the third molars were extracted during surgery. The mean operating time (for angle fracture reduction and fixation) for the study transoral approach (angulated screwdriver) was 28.10±3.3 minutes, while the TBT approach took 37.40±1.75 minutes (Table 2), which showed a significant difference (P = 0.001).
| Complication Variables | Group A | Group B | P-value |
|---|---|---|---|
|
Postoperative edema ● Mild 38(76%) ● Moderate 12(24%) ● Sever |
23 (46%) 2 (4%) 0 (0%) |
15 (30%) 10 (20%) 0 (0%) |
0.008 |
| Loose screw or plate 1 (2%) | 0 (0%) | 1 (2%) | 0.3 |
| Infection 2(4%) | 0 (0%) | 2 (4%) | 0.1 |
| Inferior dental nerve injury 1 (2%) | 0 (0%) | 1 (2%) | 0.3 |
| Facial scar 9(18%) | 0 (0%) | 9 (18%) | 0.001 |
|
Operating time ● Mean± SD ● Range (min) |
28.10±3.3 22-34 |
37.40±1.75 35-40 |
0.001 |
|
Wound dehiscence /Exposed plate/ Malocclusion/ Nonunion |
0 (0%) | 0 (0%) | - |
3.2. Postoperative Clinical Results
At the initial postoperative visit, 38 (76%) patients experienced mild postoperative swelling, which had gone by the second week; all patients were pain-free, and edema had decreased significantly in the ASD group.
There was no wound dehiscence in both groups. In group B, two patients (4%) developed the infection at the intraoral incision line, followed by mild swelling, purulent drainage, and moderate pain. An extraoral incision, drainage, and a 10-day course of oral antibiotics were used to treat this infection (P=0.1). One patient of Group B had screw loosening A, which revealed no statistical difference with group B (P=0.3).
Paresthesia was observed in one patient (2%) in group B without any significant difference (P=0.3). All patients' conditions improved within three months of surgery. Nine patients (18%) in group B developed facial scars at the TBT incision sites (Fig. 4) but none of these patients' facial nerves were affected (P=0.02)(Table 2). All patients had adequate mandibular motion with an inter-incisal opening greater than 40 mm (Figs. 5, 6).


3.3. Postoperative radiographic results
The accuracy of healing, fracture reduction, and fixation stability was assessed based on orthopantomography (OPG) scans immediately postoperative. The fractured angles were perfectly reduced in all patients. The outcomes of this surgical technique using the transoral approach using angulated screwdriver system were favorable, and most patients were satisfied with their results (Fig. 7).
4. DISCUSSION
In the current study, a six-hole single mini locking plate with a thickness of 2.0 mm and screws of 9–12 mm length were used to reduce and fix the angle fracture at the inferior border of the mandible. The use of an angulated screwdriver facilitated the intraoral approach for managing MAFs by a single rigid plate at the inferior border, according to the findings of this study.


Our department used angulated screwdrivers to fix condylar fractures using an intraoral technique. However, the more accessible use of this tool was when we used it to fix angle fractures using locking plates at the inferior border of the mandible, which was accessed through intraoral incisions. The intraoral use of a single locking plate for MAFs fixation is difficult and usually necessitates extraoral incision as submandibular or retromandibular approaches [1]. However, using an angulated screwdriver handpiece, the intraoral approach was accelerated, and the extraoral trocar skin incision was avoided, which was needed to access the most posterior far screws in the control group. The result of the present study is contrary to Wan Kenneth et al., 2012 [6], who concluded that the TBT approach was less complicated than using the intraoral technique to manage an angle fracture. However, he does not use the angulated drills and angulated screwdriver.
Angle areas are challenging intraorally for rigid open fixation; however, trials of angulated screwdrivers performed in the condylar region gave contradictory results [16]. Most maxillofacial surgeons accepted the traditional extraoral incision used for access angle area through the extraoral approach. However, the intraoral approach was mostly used for body parasymphyseal and symphyseal fracture regions [1, 3]. In the present investigation, angle fracture fixation was extremely facilitated by using ASD in group A.
Angle fractures are the most difficult mandibular fractures to treat, particularly if they are unfavourably displaced, and the fracture line is angulated more posteriorly at the inferior border of the mandible [17]. Kim M-Y et al., 2016 [9] compare three methods for angle fixation. Gonzales et al. compare angle plate techniques as well. For displaced angle fractures, the Champy single plating method, which uses a small nonrigid plate at the superior border, may not be enough to achieve optimal fracture line stability. From his finite element analysis, Hasan Korkmaz [2] and Choi et al., 1995 [18] concluded that a double miniplate is more stable than a single plate. However, several researchers, including AO experts, prefer to use rigid plating fixation forms because they provide more stability without requiring additional MMF time; additionally, our approach is consistent with Elsayed et al.' study results [1].
Failure to achieve proper anatomical reduction under stable conditions of the fractured angle leads to infection, malocclusion, or nonunion that ranges from 0 to 32% [1, 19]. The advantage of using a single rigid plate at the inferior border of an angle fracture is that it reduces the occurrence of wound dehiscence and patient palpation of the plates and screws, as well as plate exposure and screw loosening, as seen in the current research and several other studies [8, 20].
We used a single plate that was applied away from the incision line and towards the inferior border of the mandible, which gave increased flap thickness covering the plate and reduced wound dehiscence, which agrees with Sugar et al. [21]. Many observations, however, contradict this theory, indicating that wound dehiscence occurs due to secondary infection [6].
Angle fractures on the right side predominated (76%), contrary to previously reported studies. The results of our study indicated that the bone plating complication rates decreased when right side angle fractures predominated, which would agree with the results of Bouloux et al. [22] and Ellis et al. [23].
In our study, both groups were fixated by the same single mini locking plate, which did not affect the operation time. Using a single plate technique may decrease the operation cost to the patient, although the 2.0 mini locking plates are still more expensive than non-locking standard mini-plates.
Monika Parmar et al., 2021 [24] reported that the most common cause of angle fracture is a fall, which contradicts our findings that RTA is the most common cause (56%), even though males are still more affected than females by angle fractures. Third, molar was extracted in 20% of the cases, which agreed with the protocol advised by Roccia Fabio et al. [25] and Segura-Pallerès et al. [26] in their multicenter study.
Only two cases (4%) with fractured third molar developed an infection and loose screws (2%) in group B. However, these differences were nonsignificant, which agrees with Siddiqui et al. [27], who said that third molar extraction did not affect infection.
The TBT method resulted in hypertrophic scars in nine patients (18%) in group B. Therefore, many surgeons do not prefer the TBT method for patients with a tendency for keloid growth in their wounds. However, other investigators [6, 21] observed that when the TBT approach is utilized, the risk of generating an unpleasant scar is extremely low, and facial nerve palsy is insignificant. However, they did not compare their outcomes to the ASD-assisted technique.
CONCLUSION
In the current study, the use of a single locking plate and angulated screwdrivers enabled stable angle fixation via an intraoral approach and avoided the difficulties experienced during drilling and screwing of the most posteriorly positioned screws, and this can significantly reduce operation time, postoperative edema and prevent extraoral scarring.
AUTHORS' CONTRIBUTIONS
HR, MA, AO, and SAE conceived and designed the study, conducted the research, and collected and organized data. EH, SM and EA analyzed and interpreted the data. SAE, HR, EA, and MA wrote the initial and final drafts of articles. All authors gave their final approval and agreed to be accountable for all aspects of the work
LIST OF ABBREVIATIONS
| MAFs | = Mandibular Angle Fractures |
| ORIF | = Open Reduction and Internal Fixation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by Al Azhar University ethical Committee (REC-PD-21-11).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans used were in accordance with the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all patients for publication of this study and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Data is available upon request from the corresponding author [S.A.H.E].
CONFLICT OF INTEREST
The authors have no conflicts of interest relevant to this article.
FUNDING
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
ACKNOWLEDGEMENTS
Declared none.


