All published articles of this journal are available on ScienceDirect.
Guided Bone Regeneration Prior to Implant Therapy in the Esthetic Zone: A Case Report
Abstract
Background:
Implant placement on the anterior maxilla requires a comprehensive concern of adequate alveolar bone and gingival biotype. Insufficient support for hard and soft tissues becomes one of the main causes of implant complications. To avoid this problem, pre-surgical treatment with Guided Bone Regeneration (GBR) is suggested with respect to the alveolar ridge defect.
Objective:
In this study, we reported the predictability of a sandwich technique of GBR prior to implant placement.
Case Presentation:
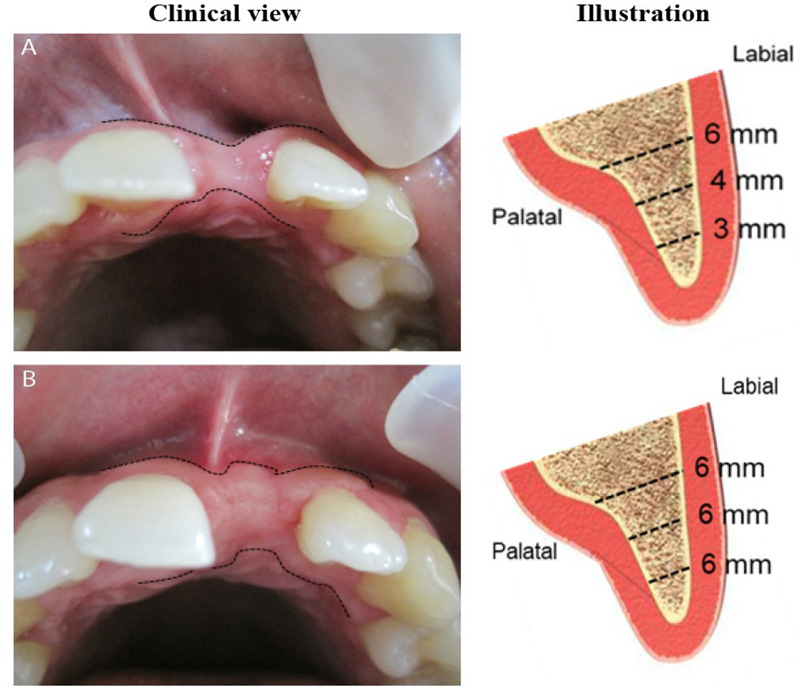
Case: Thirty-four-year-old male was referred with a chief complaint of missing teeth on area #21 accompanied by labial bone dehiscence due to trauma. Bone thickness measurement displayed was approximately 3/4/5 mm (coronal/middle third/apical third of the alveolar ridge). This case was diagnosed as soft and hard tissue deformity on area #21 prior to implant. Case management: GBR and implant placement were performed in two stages of surgery. GBR was executed by using a combination of Biphasic Calcium Phosphate (BCP) (consisting of 40% Beta-Tri Calcium Phosphate (β-TCP) and 60% Hydroxyapatite (HA)) and Demineralized Freeze-Dried Bone Allografts (DFDBA) bone graft materials. Alveolar ridge re-measurement five months after GBR showed significant bone augmentation, 6/6/6 mm (coronal/middle third/apical third of the alveolar ridge). Furthermore, a 3.5 mm (diameter) x 10 mm (length) bone-level implant was inserted accordingly. The two-year follow-up exhibited gingival stability and no sign of either recession or bone resorption.
Conclusion:
Herein, we demonstrated the effectiveness of BCP and DFDBA bone substitutes to obtain proper conditions for the long-termed stability and predictability of implant.
1. INTRODUCTION
Horizontal bone deficiency in the anterior maxilla is mostly due to periodontitis, trauma, or subsequent to dental extraction [1-3]. Moreover, El-Nahass et al. reported that the mean labial bone thickness at central incisors was less than 1 mm [4]. In cases where ridge preservation is not made right after tooth extraction, the bone dimension is often reduced or even collapsed within a few weeks after tooth extraction [5-7]. Indeed, this condition makes its further management more complex. Of interest to insufficient morphological anatomy to support implant placement, bone augmentation and/or soft tissue grafting therapy are often recommended [1, 3, 8-13].
Various surgical techniques and biomaterials have been developed for the optimization of implant placement in the resorbed alveolar bone. Buser et al. reported that autogenous graft is the best graft material since it exerts potent osseo-conductive and osseo-inductive properties [14]. However, the limited availability of this graft and additional donor site operations are some of the limitations. Interestingly, the combination of bone grafting materials, also named the sandwich technique, has been performed and shown to be beneficial in terms of horizontal or vertical bone gain and implant placement [3, 7, 15, 16]. Moreover, Wang et al. explained that the sandwich technique improved the composition of native bone [17]. Regarding the grafting material, the combination of alloplastic allograft and/or xenograft materials could mimic the natural characteristic of autologous graft [17, 18].
The objective of this case study was to correct bone and soft tissue deformities classified as Seibert class I prior to implant placement. Herein, we demonstrated that the GBR approach using the sandwich technique of BCP and DFDBA achieved an adequate alveolar ridge volume for anterior implant placement. Moreover, we have found that this therapy enforces long-termed stability of dental implants.
2. CASE
A 34 years old male was referred to the Department of Periodontology Clinic, Dental Teaching Hospital, Faculty of Dentistry, Universitas Indonesia, complaining about the anterior missing teeth followed with bone dehiscence. Patient sought to get a fixed prosthetic therapy, which was the dental implant. According to the dental history, tooth loss was caused by an accident that happened 2 years ago. The patient neither had systemic disease nor extra-oral abnormalities.
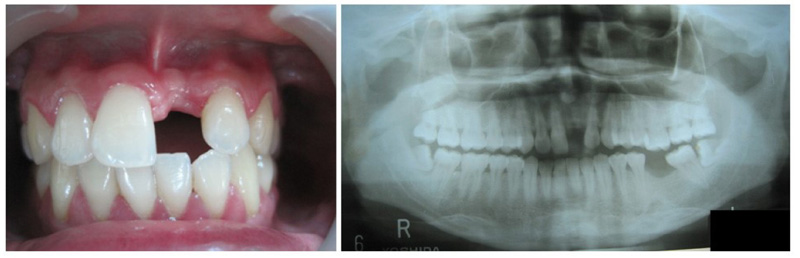
The intra-oral examination indicated relatively good oral hygiene (Silness and Loe) without any signs of inflammation [19]. Specific to area #21, the length of mesial distal was relatively ideal (8 mm), but not for the labial-palatal dimension. Bone thickness analysis illustrated a horizontal alveolar ridge defect class I according to Seibert classification [20], approximately 3/4/5 mm (coronal/middle third/apical third). Keratinized gingiva and gingival biotypes were 6 mm thick, respectively. Panoramic radiograph revealed no interproximal bone loss (Fig. 1). This case was diagnosed as soft and hard tissue deformity on area #21 prior to implant.
3. CASE MANAGEMENT
After a thorough analysis, we diagnosed this case as a mucogingival deformity and planned to do a GBR to augment the bone prior to implant placement with a good prognosis [21, 22]. The GBR and implant therapy were performed in two stages of surgery. Briefly, local anesthesia of 2% lidocaine (1:50,000 epinephrine) was administrated in the labial and palatal sides. Papilla preservation flap was made in this case. Vertical incisions were made on 2/3 of the mesial angle of adjacent teeth (Fig. 2A). Full thickness flap was elevated. Bone decortication was made using a slow-rotating small diameter bur (Fig. 2B). Then, GBR was conducted by using the sandwich technique of Biphasic Calcium Phosphate (BCP) (40% β-Tri Calcium Phosphate (β-TCP) and 60% Hydroxyapatite (HA)) on the upper part and Demineralized Freeze-Dried Bone Allografts (DFDBA) on the base (Fig. 2C). A long-termed resorbable collagen membrane was applied to cover the bone graft. Nylon 5.0 was used to suture the flap (Fig. 2D). Oral hygiene care instruction was given to the patient and an analgesic was prescribed. A removable denture was placed gently due to aesthetic reasons (Fig. 2E). Patient had consecutive monthly appointments for observation and follow-up. No adverse effect was found.
Five months after the GBR procedure (Fig. 2F), alveolar ridge thickness reassessment exhibited bone volume improvement into 6/6/6 mm (coronal/middle third/apical third of the alveolar ridge). This thickness was quite ideal for anterior implant placement. Then, at the second surgery, the flap was reopened, and a 3.5 mm (diameter) x 10 mm (length) of bone-level implant (Straumman) was inserted accordingly (Fig. 2G-2I). The tension-free flap was closed and sutured using 5.0 nylon (Fig. 2J, K). After the surgery, the patient was instructed to use chlorhexidine gluconate 0.12% mouthwash two times/day for 2 weeks and to take care of personal oral hygiene. Two weeks after the second surgery, no sign of rejection was noticed, after which the stitches were removed. A provisional crown made from the composite resin was screwed to the implant to create a better emergence profile of the gingiva; the final crown was placed later. Twelve months from baseline, the implant was stable without any sign of inflammation or implant tread exposure (Fig. 2L). On the top of that, patient is satisfied with the outcome.

4. DISCUSSION
In respect to implant placement in the esthetic area with mucogingival deficiencies, several issues must be taken into consideration, such as the height of hard tissue for support, the favorable crown/implant ratio, the amount of keratinized gingiva, and an adequate vascularization for either grafts or dental implant [15, 23, 24]. Herein, the case was diagnosed as Seibert class I ridge defect classification with approximately 3/4/5 mm (coronal/middle third/apical third) bone thickness. According to the guideline for implant therapy, it is important to have 2 mm of the bone surrounding the implant to overcome small bone resorption that might occur during the osseo-integration period [25, 26]. The long junctional epithelium without periodontal fibers is mainly constructed in peri-implant tissue, which is yet another concern [18, 27]. Therefore, the presence of keratinized gingiva as a mechanical barrier function is crucial to give a better peri-implant seal, thereby preventing bacterial invasion [23, 28-32]. This case exhibited an adequate keratinized gingiva with a thick gingival biotype. Therefore, we focused on improving bone volume with a bone graft, which corrects the soft tissue deficiency consequently.
In the present study, we performed GBR and implant placement in two-different operation times. We were concerned about the vascularization matter that affects the integration of either the bone graft to native bone or implant to native bone [6, 14, 16, 33, 34]. Therefore, GBR was established 5 months prior to the implant placement. On the contrary, recent studies demonstrated these procedures simultaneously and observed great precision and accuracy outcomes, thus saving time for the patient and clinician [24, 25]. Unlike our study, Mansour et al. conducted a sandwich osteotomy technique on the cortical bone using a carbide disc, then inserted the implant on the down-fractured segment up to the basal bone [25]. Xenograft materials were filled in the gap between fractured segment, bone, implant, and basal bone, accordingly [35, 36]. In respect to the study done by Mansour et al. [25], the risk of tissue necrotic, which might occur easily due to lack of vascularization and instability of the implant, was our main concern. Taken together, we propose that a less traumatic procedure, adequate blood supply, and healing capacity time through two step surgical phase are desirable.
Although autogenous bone graft remains the gold standard in alveolar reconstructive surgery [14, 16, 20], in this present study, we used a combination of allograft and alloplastic/synthetic grafting material to augment the bone. Briefly, DFDBA, a human allograft, was placed next to the native bone to promote osseo-inductive and conductive functions, while BCP, a mixture of 40% β-TCP and 60% HA, placed on the upper part was served as a scaffold. This idea suggests that its combination brings higher efficacy towards GBR.
Thus, a previous investigation conducted by Miyamoto et al. based on the clinical evidence suggests the goal of the GBR procedure is that peri-implant bone thickness should be more than 1.8-2.0 mm [37]. Moreover, experts recommend even greater peri-implant bone thickness to maintain the stability of the implant [2, 38, 39]. In parallel, the GBR procedure in our study improved the labial bone up to 2-3 mm significantly (Fig. 3). Interestingly, we noticed that this achievement was partly regulated by the membrane characteristics. A long-termed resorbable collagen membrane was used in the present study, in accordance with a previous study done by Sulijaya et al. [3]. It is known that bone regeneration needs at least 4-5 months until it matures, while soft tissue regeneration is relatively faster [13, 16, 40]. In some cases of GBR failure, granulation tissue formation and lack of bone callus formation were often found in this matter [3, 7]. Therefore, the longer resorption time of the membrane allows the bone grafts to regenerate and prevent them from soft tissue proliferation.
This case report has a limitation due to technical issue. The evaluation period is limited up to twelve months due to COVID-19 pandemic situation. The number of patient visits and aerosol generating procedures are reduced in the hospital. However, the evaluation shown here suggests that GBR procedure prior to implant placement is an effective option.
CONCLUSION
In conclusion, GBR with the sandwich technique could be served as a therapy to create an adequate condition for anterior implant placement. Thus, this approach enhances outcome predictability and long-termed implant stability. Longer observations on the stability of dental implants and different bone defect cases will be our consideration for further study.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All study protocols were approved by the local ethics committee of the Department of Periodontology, Faculty of Dentistry, Universitas Indonesia as the standard operational procedure (SOP) of the treatment.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study.
CONSENT FOR PUBLICATION
Informed consent has been obtained with respect to scientific purposes.
STANDARDS OF REPORTING
CARE guidelines were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
CONFLICT OF INTEREST
The authors have no conflicts of interest in this study.
FUNDING
No funding has been received for this study.
ACKNOWLEDGEMENTS
The authors thank the Periodontology Unit, Dental Teaching Hospital, Faculty of Dentistry, Universitas Indonesia for the support and facility in performing the case.


