All published articles of this journal are available on ScienceDirect.
Pulse Oximetry and Three-Dimensional Analysis in Evaluating Immature Permanent Teeth Apexogenesis: Two Case Reports
Abstract
Background:
Apexogenesis is a vital pulp therapy that aims to preserve pulp vitality and maintain root formation in not-fully-formed permanent teeth with exposed pulp from trauma or caries. To achieve success, reliable diagnostic tools are required to assess the pulp health and tooth development stage, design an appropriate treatment plan and evaluation, and follow-up. Pulse oximetry is a non-invasive method for monitoring pulp oxygen saturation, which corresponds to pulp vitality.
Case Presentation:
This case report describes the successful apexogenesis of two pulp exposure-immature permanent teeth treated with acemannan, an implantable natural biomaterial extracted from aloe vera. Based on pulp oxygen saturation level, clinical evaluation, and radiographic examination, the teeth were asymptomatic with preserved pulp vitality and continued root development.
Conclusion:
Therefore, as an auxiliary tool, pulse oximetry could be useful for diagnosis, treatment, and follow-ups of apexogenesis therapy.
1. INTRODUCTION
The goal of apexogenesis is to preserve a vital pulp in not-fully-formed permanent teeth exposed pulp from trauma or caries to continue root development until apical closure [1]. The success of this technique is multifactorial, including accurate diagnosis, suitable capping materials, an appropriate treatment plan, and follow-up, and cooperative patients and parents.
The real-time, reliable, objective pulp status is required to achieve the correct diagnosis and treatment plan. Although the conventional thermal and electric pulp test (EPT) provides high specificity and positive predictive value in mature permanent teeth, it is not applicable for deciduous and incompletely-formed permanent teeth [2]. False-positive responses are seen in emotional and anxious pediatric patients anticipating pain. Young myelinated nerve fibers Rashkow’s plexus at the dentin-pulp border, nerve rupture, and ischemic injury produce a false negative response in immature teeth. Therefore, pulse oximetry, a painless, reliable, objective tool for chair-side screening, has been proposed for assessing pulp vitality [3]. The advantage of this tool is its ability to determine the oxygen level (oxygen saturation) in the blood supply of the dental pulp [4]. This is critical because the blood supply is the most determinant factor for tissue vitality, especially in vital pulp therapy; therefore, determining tissue oxygen levels is superior to other evaluation methods [3].
Based on these findings, the present report describes the successful apexification of two not-fully-developed permanent teeth with pulp exposure using acemannan as a pulp capping material and evaluating the use of pulse oximetry as an integrated auxiliary tool for diagnosis, evaluation, and follow-ups.
2. CASE REPORTS
2.1. Case no. 1
An 8-year-old girl was referred to the Department of Endodontics, National Hospital of Odonto Stomatology, Hanoi, Vietnam, for an accidental crown fracture of the upper left central incisor (tooth #21). The accident occurred one hour prior to admission. Her medical history was non-contributory, and the traumatized tooth had no previous dental treatment or caries.
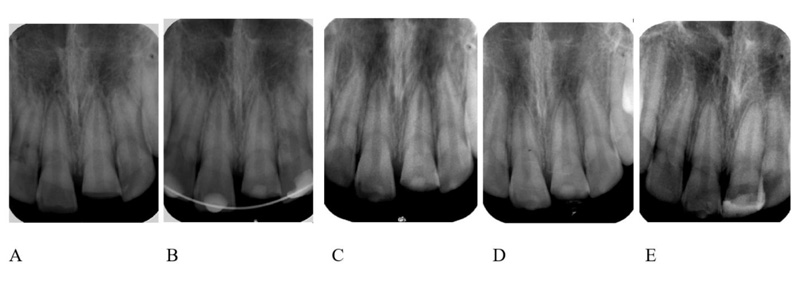
A clinical examination revealed an oblique crown fracture of tooth #21 with pulp exposure. Tooth #11 was mobility grade II. Teeth #11 and #21 were slightly tender to percussion and showed a negative response to the cold test. These teeth were examined using pulse oximetry (sat801+, Bitmos, Germany). The oxygen saturation levels of tooth #11 and tooth #21 were 87% and 84%, respectively. The preoperative radiograph revealed a crown fracture of tooth #21 with pulp exposure and immature root development. No pathological signs were observed on the radiograph (Fig. 1A and 1B). Based on the clinical and radiograph findings, the maxillary left central incisor was diagnosed with reversible pulpitis. The apexogenesis treatment plan using acemannan was designed with the informed consent of the patient’s parents.
Local anesthesia (4% articaine with 1:100,000 epinephrine (Septanest, Septodont, France)) was delivered, and a rubber dam was placed on the tooth and flushed using 0.12% chlorhexidine. Access to the pulp exposure was obtained using a diamond fissure bur. Pulp horn bleeding was observed; thus, a partial pulpotomy procedure was performed. The inflamed pulp tissue was gently removed (1.5–2 mm deep) using a high-speed abrasive diamond bur and sterile normal saline. The healthy pulp was flushed with 2% NaOCl, and hemostasis was obtained by placing moist cotton pellets over the pulp stumps (2 min light pressure). An acemannan sponge (1 mg in a 2.5x2.5x2 mm3) was prepared as previously described [5], and gently placed over the remaining healthy pulp. The cavity was lined with glass ionomer cement (Base cement, Shofu, Japan) and restored with a permanent composite restoration (Filtek Z350XT, 3M ESPE, St Paul, MN, USA). Teeth #12, #11, and #22 were splinted together with a composite splint. The patient and parents called on day 1 and day 7 post-surgery about any pain adverse reactions due to the treatment. We found that the patients experienced only mild pain after 24 h. After taking paracetamol for pain relief, no adverse effects were reported.
The patient was evaluated 28 days after surgery. When the patient had a successful evaluation, their composite splint was removed. The patient was evaluated at 3-, 6-, 9- and 12-months post-treatment follow-up visits. Tooth #21 was asymptomatic, and the color of the crown did not change. A cold test and pulse oximetry test were performed at each follow-up visit and the results were within the normal range (Table 1). The continuity of the periapical ligament space and absence of a pathological lesion at the periapical area and root surface were observed at 6-, 12-, and 24-months post-treatment (Fig. 1C-E). Continued root development and a narrowed root apex were observed. Apexogenesis treatment success was confirmed.
2.2. Case no. 2
An 8-year-old girl was brought to the Department of Endodontics, National Hospital of Odonto Stomatology, Hanoi, Vietnam, with a chief complaint of food impaction pain at the right lower posterior teeth. Her medical history was non-contributory. Clinical examination revealed that tooth #46 had a deep carious lesion, which caused food impaction. No pathologic mobility or periodontal pocket was detected. A cold test and pulse oximetry demonstrated vital pulp responses within normal limits (Table 1). The tooth was asymptomatic to percussion. The radiographic examination revealed that the tooth had immature apices with deep caries located on the occlusal surface near the pulp chamber (Fig. 2A). The treatment options, including either indirect pulp capping if there was no pulp exposure or partial pulpotomy if pulp exposure occurred during caries removal, were explained and informed consent of the patient’s parents was obtained.
| - | Preop | 3 months | 6 months | 9 months | 12 or 14 months | |
|---|---|---|---|---|---|---|
| Case 1 | Treated (tooth #21) |
84 | 83 | 81 | 82 | 82 |
| Control (tooth #11) | 87 | 84 | 78 | 83 | 84 | |
| Case 2 | Treated (tooth #46) |
80 | 78 | 76 | 77 | 79 |
| Control (tooth #36) | 79 | 80 | 78 | 78 | 79 | |
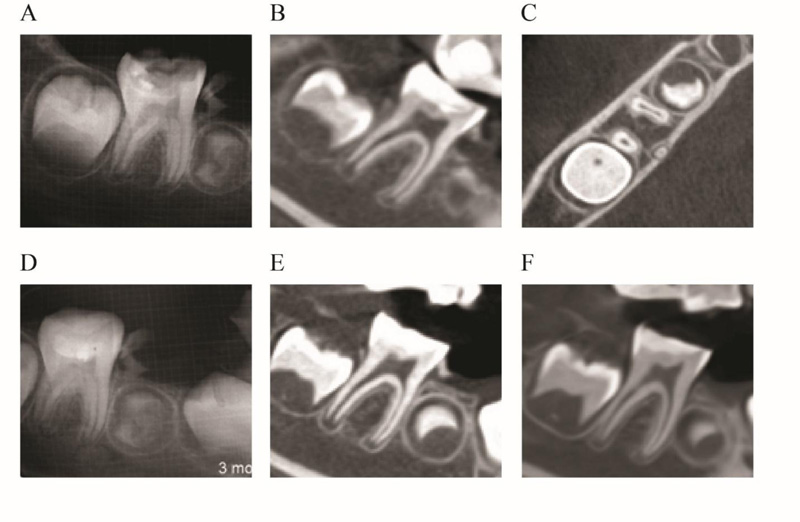
Under local anesthesia (4% articaine with 1:100,000 epinephrine; Septanest, Septodont, France) and rubber dam isolation, the caries was removed using a round carbide bur. After completely removing the caries tissue, a pinpoint pulp exposure was observed at the deepest caries area, and partial pulpotomy treatment was selected. The inflamed coronal pulp tissues were removed to a 2 mm depth using a sterile high-speed round diamond bur under sterile water cooling. The remaining healthy pulp was rinsed with 2% NaOCl and moist cotton pellets were placed over the pulp stumps with light pressure for 2 minutes for hemostasis. An acemannan sponge was placed over the pulp, and the cavity was lined with glass ionomer cement (Base cement, Shofu, Japan). Finally, the tooth was restored with a composite resin (Filtek Z350XT, 3M ESPE, St Paul, MN, USA). Because the periapical radiograph suggested the presence of an unusual three-rooted lower first molar, an immediate post-treatment CBCT radiograph was taken. CBCT showed the complicated and rare anatomic characteristic of tooth #46 with three (mesial, distal, and distolingual/radix entomolaris) roots and four (mesiobuccal, mesiolingual, distal, and distolingual) root canals (Fig. 2B-C). Paracetamol was prescribed if the patient developed post-treatment pain. Follow-up phone calls to the patient and her parents were placed on day 1 and day 7 post-treatment concerning any adverse effects from the operation. Due to no post-operative pain, the patient was not prescribed any medicine.
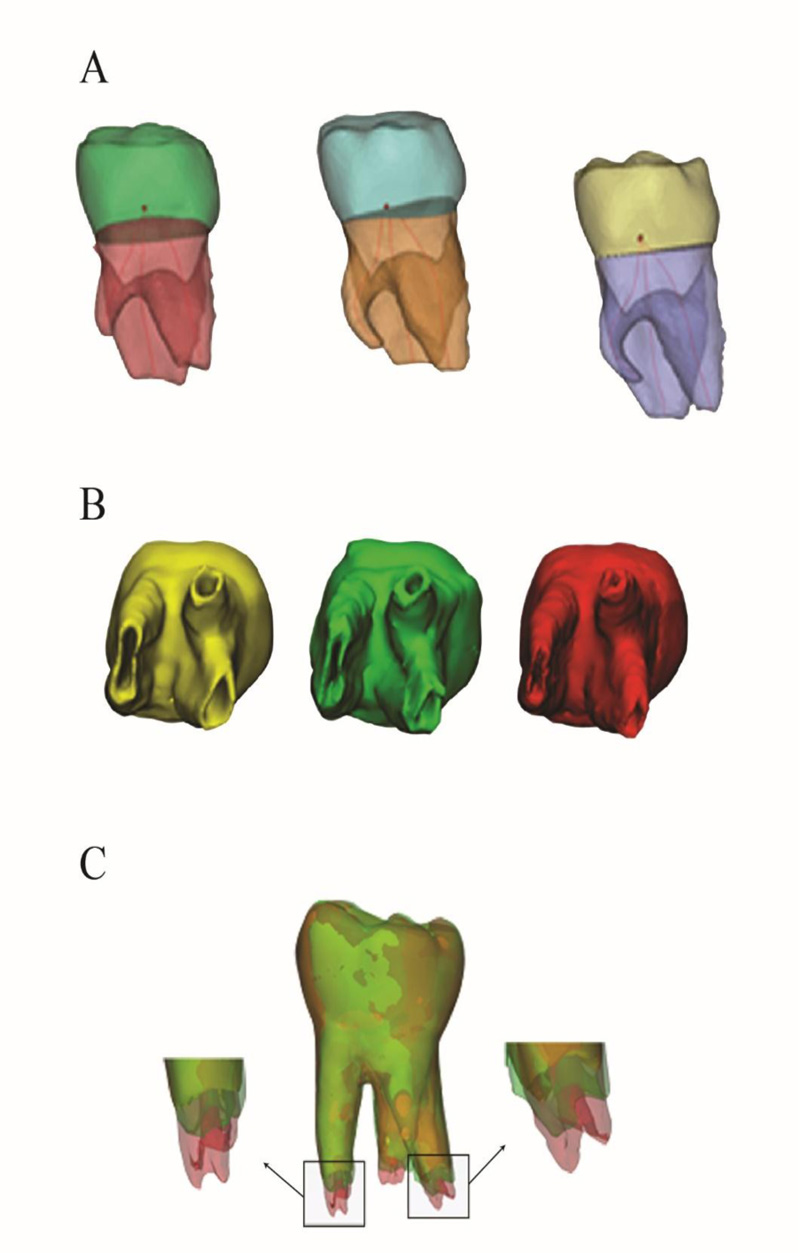
The patient was evaluated 3-, 6-, 9-, and 12-months post-treatment. At these follow-ups, the patient was asymptomatic, and pulp vitality tests (including the cold test and pulse oximetry test) were within normal limits (Table 1). The periapical radiograph demonstrated a continuous periapical ligament space and absence of a periapical lesion at 3-months post-treatment (Fig. 2D). However, the continued root formation could not be evaluated by a periapical radiograph. Due to a painful/uncomfortable experience, while taking radiographs at the 3-month post-treatment evaluation, the patient refused to take a periapical radiograph at the 6-month follow-up. CBCT with an ultra-low dose mode was performed at 6- and 14-months post-treatment with the parent’s permission. For protection, the patient wore lead devices to protect her chest organs and thyroid gland. The CBCT radiograph revealed a non-pathologic tooth with normal root development and root apex formation (Fig. 2E-F). The 3D reconstruction was performed using Mimics software (Materialise, Leuven, Belgium) to evaluate treatment progress and explain the results to the patient and her parents. The 3D reconstruction images regarding immediate, six-month, and 14-month post-treatments demonstrated increased root length and apical foramen closure (Fig. 3A-C).
3. DISCUSSION
The purpose of vital pulp therapy is to preserve pulp vitality and maintain the tooth in the jaw. Apexogenesis addresses an important goal for treating an incompletely-formed permanent tooth with its pulp exposed by trauma or caries, and partial pulpotomy is generally regarded as the treatment of choice to achieve this objective [6]. Compared with a full pulpotomy, a partial pulpotomy has many advantages, including being a less invasive operation and preserving the cell-rich coronal pulp tissue dentinogenesis and apexification, which reduces crown fracture risk [7]. In the present report, case no. 1 was an immature central incisor with pulp exposure due to trauma, and case no. 2 was an immature lower first molar with extensive deep caries. Caries and trauma are the most common causes of pulp exposure [8].
Based on the WHO declaration, patients should receive the appropriate treatment without racial or economic restrictions. Although the modified portland cement (mineral trioxide aggregate) and calcium-silicate-based materials (Biodentine) are widely used as capping agents for partial pulpotomy [9], the cost of these materials is high for developing countries. Thus, scientists are looking for alternative materials at a reasonable cost. Acemannan is a natural polysaccharide with unique acetylated mannose residues extracted from aloe vera. In animal and clinical studies, acemannan induced osteo-dentin bridge formation with vital pulp tissue beneath it [10, 11]. Therefore, acemannan would be an alternative implantable biomaterial to promote pulp healing for vital pulp therapy similar to MTA and Biodentin [12].
Evaluating the pulp status is an important step for selecting the appropriate vital pulp therapy. An ideal technique should be non-invasive, painless, reliable, standardized, and practical to perform. The traditional methods, including EPT and thermal tests, require sufficient numbers of mature neurons to reach an effective pulp response level. However, because deciduous and immature permanent teeth lack complete innervation, these methods are less reliable for pediatric patients [13]. In addition, EPT and thermal tests cause unpleasant stimuli, which may result in uncooperative children patients and compromise their responses to pulp testing [14].
The use of pulse oximetry in diagnosing pulp status, especially in vital pulp therapy, has been introduced and used on newly traumatized permanent teeth in which temporary nerve paresthesia reduces thermal test and EPT effectiveness and reliability [15, 16]. These results corresponded to case no.1, where the traumatized tooth had a negative thermal response but had a positive oxygen saturation level. Pulse oximetry may also be useful for the follow-up evaluations of apexogenesis treatment because it is effective in identifying oxygen saturation values in relation to the stages of root development [17]. However, to our knowledge, most reports have only studied using pulse oximetry in anterior teeth. This is mainly because of the greater frequency of traumatic injuries to these teeth and the difficulty in adapting the sensor to molar tooth anatomy [18, 19]. In the present report, we used oximetry in the upper central incisor and lower first molar (case no. 2) and obtained reliable results corresponding to the clinical follow-up and outcome radiograph. To perform our investigations, we used the pediatric probe, which is small, flexible, and adaptable to the buccal and lingual surface of the tooth.
Radiographs provide visually unobservable hard tissue and pathological lesion information, which plays a crucial role in diagnosis, treatment planning, and evaluation. We found no pathologic radiographic signs of external or internal resorption, abnormal root canal calcification, or periapical lesion during the follow-up period were detected, confirming successful apexogenesis. The results revealed an unusual three-rooted lower first molar containing a distolingual/radix entomolaris root in case no. 2. A radix entomolaris was first reported by Carabelli in 1844 and is most commonly found in lower first molars rather than lower second and third molars [20]. Certain ethnic and racial groups, such as Mongoloid traits: Eskimo, Chinese, and American Indians, have a higher prevalence compared with Caucasians [21]. This extra root is always superimposed on the distal root, resulting in an inaccurate diagnosis and treatment in endodontics and surgery [22]. CBCT allows for superior diagnosis and management of teeth with unusual anatomy without superimposed anatomical structures and produces undistorted 3D reconstructions of the maxillofacial skeleton and 3D images of the teeth and their surrounding tissues [23, 24]. However, the radiation dose for CBCT is much higher than intraoral radiography. The CBCT should be used only when the need for imaging cannot be met by lower-dose two-dimensional (2D) radiography [25].
CONCLUSION
From our limited data, pulse oximetry significantly contributed to the favorable diagnosis and treatment follow-up outcomes and can be regarded as a valuable integrated tool in vital pulp therapy of immature teeth. Based on these two case reports, we show that acemannan is a promising implantable natural biomaterial as capping material for partial pulpotomy of immature permanent teeth to induce continued root formation.
CBCT offers a 3D analysis that allows diagnosis and follow-up of vital pulp therapy especially for teeth with unusual anatomy.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Hanoi National Hospital of Odonto Stomatology, Vietnam (No. 217/HDDD-BVRHMTW).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from patients and their parents for treatment and publication.
STANDARDS FOR REPORTING
CARE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This work was supported by the Ratchadaphiseksomphot Endowment Fund of the 90th Anniversary of Chulalongkorn University Fund, TSRI Fund (CU_FRB640001_32_2), and the 100th Anniversary Chulalongkorn University Fund for Doctoral Scholarship.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this paper.
ACKNOWLEDGEMENTS
We thank Professor Dr. Visaka Limwong, Associate Professor Dr. Dolly Methatharathip, and Dr. Kevin Tompkins for their valuable suggestions and technical support.


