Restoration of Root Filled Teeth; Current Opinions and Techniques
Abstract
Purpose:
To examine current decision-making preferences of Jordanian dentists when Restoring Root Filled Teeth (RFT).
Materials and Methods:
834 Jordanian general dentists, prosthodontists and endodontists were invited to participate in a validated online survey with a 62% participation rate. Respondents were invited to answer 24 questions about their preferences for techniques and materials they use to restore RFT. The questions aimed at exploring restorative strategies commonly employed by Jordanian dentists when managing root filled teeth with extensive loss of tooth structure.
Results:
A minority of dentists consider direct resin restoration as the sole restoration for RFT with extensive loss of tooth structure. Full coverage metal-ceramic and all-ceramic crowns are more popular than endocrowns when restoring RFT with indirect restoration. Fiber posts are the most popular type of posts, followed by prefabricated metal posts. Glass ionomer is the most preferred cement for luting metal posts, while conventional dual resin cement with separate etch and rinse bonding strategy is the most employed when bonding fiber posts. The majority of dentists tend not to pretreat fiber posts. Loss of post/core retention or fracture of coronal tooth structure are the two most common reasons observed by dentists when RFT fail.
Conclusion:
Use of post and core is still preferred over more conservative approaches when restoring RFT with extensive loss of coronal tooth structure. Longevity of restorations can be enhanced by training practicing dentists on evidence-based adhesive strategies.
1. INTRODUCTION
Root canal treatments are normally indicated when pulpal health has been jeopardized beyond repair and removal of the pulp tissue is needed. The primary goals of endodontic treatment are to relieve pain or discomfort, clear or prevent infection, and to restore normal occlusion, function and aesthetics [1]. Usually Root Filled Teeth (RFT) suffer from substantial loss of coronal tooth structure resulting from the presence of primary or secondary caries, restorations, trauma and access cavity preparation [2]. There are also changes in the structural and mechanical properties of dentine that occur following endodontic treatment [3, 4] and the accompanying loss of coronal tooth structure [5]. Hence the prognosis of the RFT is highly dependent on the design of the final restoration [6, 7].
With improvements in bonding to tooth structures, RFT can be restored with direct resin composites or indirect restorations when cuspal coverage is deemed necessary. Endocrowns and partial crowns have also been suggested recently to restore RFT with extensive loss of coronal tooth structure [8, 9]. Nevertheless, intraradicular posts may be deemed necessary to improve retention of the restoration material to the remaining tooth structures particularly when incomplete ferrule is established. A wide range of posts and cement types are available on the market for restoring endodontically treated teeth.
Previous studies have shown that the prognosis of RFT depends not only on the remaining tooth dentine [10] but also on the periapical status and position of the tooth, the number of adjacent teeth and occlusal contacts [11]. It is further influenced by post-endodontic restoration [12]. This will leave the restoring dentist with decisions to contemplate to use a post or not, which post, how to prepare the post space, which cement, and many other aspects [13].
Several types of intraradicular posts are available, including cast metal post and prefabricated post [10, 14-17]. Glass fiber posts are currently the most popular [18]. Compared with metal post, glass fiber post has the following advantages, such as better aesthetics, similar modulus of elasticity and rigidity comparable to dentine. Glass fiber posts have a lower risk of root fracture than metal posts [19].On the other hand, glass fiber post normally fails due to loss of retention [20].
A wide range of restorative materials can be used as a core material or direct restorations such as composites, amalgam, glass ionomer and resin-modified glass ionomer [21]. The indirect restorative options could be ceramics, metal ceramics, gold alloys and base metal alloys, which can be produced using conventional techniques or CAD/CAM technologies [22].
Dentist-related factors like experience and postgraduate training can influence the decision-making process [23]. The skills of a dentist can be improved over time in clinical practice. However, the introduction of new materials in the market requires training and updating knowledge of dentists to ensure the best applications of the new materials [23-28].
Inadequate restorations adversely affect the prognosis of the tooth regardless of the quality of the endodontic treatment [6]. Despite the large amount of literature relative to the restoration of the RFT, dentists appear to slowly adapt to new knowledge and technologies. Lack of awareness among dentists regarding modern concepts and techniques could compromise the quality of dental care, especially in developing countries where financial resources might be limited.
The number of qualified dentists per capita in Jordan is probably one of the highest in the Middle East. Although a small percentage of dentists enroll in advanced education or training in restorative dentistry or prosthodontics, most practicing dentists lack further formal education beyond their basic dental degree. In addition, more than half of general practitioners obtain their educational qualifications from various schools worldwide; therefore, considerable variations in education background and clinical experiences exist among Jordanian dentists.
Surveys are an important tool for discerning dentists’ understanding of treatment attitudes and their knowledge about RFT which is gained by sharing experience between practitioners [29].
National and multinational surveys regarding the restoration of RFT have been carried out in many countries, including the USA, Northern Ireland, Sweden, Switzerland, Saudi Arabia, Germany, Brazil, India and New Zealand [29-37]. No research of this kind has been carried out in Jordan. The purpose of this study is to investigate the current concepts, opinions, techniques and materials used among dentists practicing in Jordan with regard to the restoration of RFT.
2. MATERIALS AND METHODS
This research project was approved by the ethics committee of the school of dentistry, the University of Jordan(201/2019), and carried out between June and September 2019. The required information was collected through an anonymous questionnaire. The questionnaire was adopted from a previous study [37] and modified to suit the requirement of the present study. Dentists who gave their consent to participate could access and complete the questionnaire via the online link. All responses were anonymous.
The questionnaire was first piloted among 10 specialist dentists and 20 general dental practitioners. Feedback was sought regarding the completeness and clarity of the questions and the questionnaire was amended accordingly. The final format of the questionnaire consisted of two parts, demographic information and multiple choice type questions. The demographic part of the questionnaire consisted of six questions regarding dentists’ personal information; age, gender, highest qualification, country of the professional dental degree, workplace and experience.
The second part contained 24 questions focused on the treatment opinions of post-endodontic restoration, materials and techniques used. The dentist was permitted to choose more than one answer in 6 out of 24 questions. The questions covered the following topics:
2.1. Frequency of Using Intracanal Post and Opinions
The participants were asked how frequently they require placing posts and their opinions whether the RFT has become more susceptible to fracture, the timing of the restoration of the tooth after endodontic therapy and whether every RFT must receive a post. The participants were also asked about the important factors that should be evaluated on the radiograph before restoration of RFT, their opinion about the function of the post and the possibility of using pins instead. They were also asked about whether a ferrule effect increases fracture resistance or not and the most important factor to increase successful retention of a post.
2.2. Definitive Restoration
The participants were questioned about the frequency of using posts depending on tooth location and restoration modalities of different situations, such as the type of restoration of RFT when used as an abutment for fixed partial denture for a single crown. They were asked about the frequency of planning indirect restorations for RFT.
2.3. Material Preferences
The participants were asked regarding commonly used post systems, post design, restorative materials used to construct core and cement used, and solutions used to rinse canal before cementation.
2.4. Causes of Failures
In addition to the frequency of encountering RFT with cracked coronal tooth structure and RFT with root fracture, the participants were asked about the most frequent causes of failure of posts.
A list of general dental practitioners and specialist dentists registered with the Jordanian dental association with a valid e-mail address and telephone number was provided to the investigators. From this list, a random sample of 834 general and specialist dentists was selected using computer-generated random sampling. The questionnaire was prepared in both Arabic and English languages, and each dentist was allowed to choose either version. Both versions were given to ensure an understanding of the dental terms.
Statistical analysis was performed using SPSS for Windows release 16.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were generated and a Chi-square test was used to examine differences between the groups. The significance level was determined at P < 0.05.
3. RESULTS
3.1. Demographics
The questionnaires were completed and returned by 534 respondents. Twenty-two questionnaires were unanswered; therefore, the final material consisted of 512 answered questionnaires. The answers were provided by 384 general dental practitioners, 94 prosthodontists, and 34 endodontists. Of the general practitioners, 54.4% were females, compared to 43.6% and 41.2% of the prosthodontists and endodontists, respectively. The majority of general practitioners (53.2%), prosthodontists (61.7%), and endodontists (67.6%) had a clinical experience of more than 10 years.
The respondents’ data related to primary location of clinical practice and the country where the professional dental degree has been received are shown in Table 1.
3.2. Beliefs and Frequency of Use of Posts
Of the GDPs, 37.8% restored more than 20 RFT per month compared to 29.8% and 52.9% of the prosthodontists and endodontists, respectively.
A significantly higher percentage of GDPs believe that RFTs are more susceptible to fracture compared to teeth with vital pulps compared to prosthodontists and endodontists (P = 0.002). The gender of respondents or their length of experience or country of graduation did not affect this belief; however, significantly less percentage of respondents practicing at universities held that belief (P= 0.001). Although a higher percentage of GDPs believed that every RFT must receive a post compared with prosthodontists and endodontists, the difference did not reach statistical significance (Table 2). The latter belief was significantly held by a higher percentage of those who practiced at the Ministry of Health (P= 0.043), had more than 15 years of clinical experience (P= 0.002), and those who graduated from other Arab countries or Asian countries (P= 0.024).
As shown in Table 2, prosthodontists and endodontists believed that the main advantage of posts is to provide retention to the core material, while GDPs believed that posts reinforce RFT and provide retention to core material (P<0.001) Table 2. The belief that posts reinforce RFT was held by a higher percentage of males (P= 0.022), those who graduated from other Arab or Asian countries (P<0.001), those who practiced at Ministry of Health and private clinics (P= 0.002), and those who had more than 15 years of clinical experience (P<0.001). Significantly more GDPs believe that pins should be used instead of a post for the retention of a core material (P = 0.002).
| - | General practitioners % |
Prosthodontists % |
Endodontists % |
|
|---|---|---|---|---|
| Clinical practice | Ministry of Health | 87.5 | 7.8 | 4.7 |
| Royal Medical Services | 63 | 30.5 | 6.5 | |
| Private | 81.4 | 13.6 | 5 | |
| University-based | 46.2 | 38.8 | 15 | |
| Country of professional degree | Jordan | 77.9 | 16.2 | 5.9 |
| Other Arab countries | 85.1 | 8 | 6.9 | |
| Asian countries | 86 | 11.6 | 2.3 | |
| West Europe & USA | 31.4 | 54.9 | 13.7 |
| Question | Response | General practitioners % |
Prosthodontists % |
Endodontists % |
P-value |
|---|---|---|---|---|---|
| Do you believe that RFT are more susceptible to fracture compared to teeth with vital pulps? | Yes | 93.8 | 83 | 85.3 | 0.002 |
| Do you believe that every RFT must receive a post? | Yes | 5.5 | 1.1 | 0 | 0.072 |
| Do you believe that a post will reinforce an RFT and reduce the chances of fracture and/or provide retention for the core material? | Reinforce | 7.3 | 3.2 | 2.9 | <0.001 |
| Provide retention | 48.8 | 78.7 | 79.4 | ||
| Both | 37.5 | 13.8 | 11.8 | ||
| None | 6.3 | 4.3 | 5.9 | ||
| Do you believe that pins should be used instead of a post for the retention of a core material? | Yes | 12.3 | 2.1 | 0 | 0.002 |
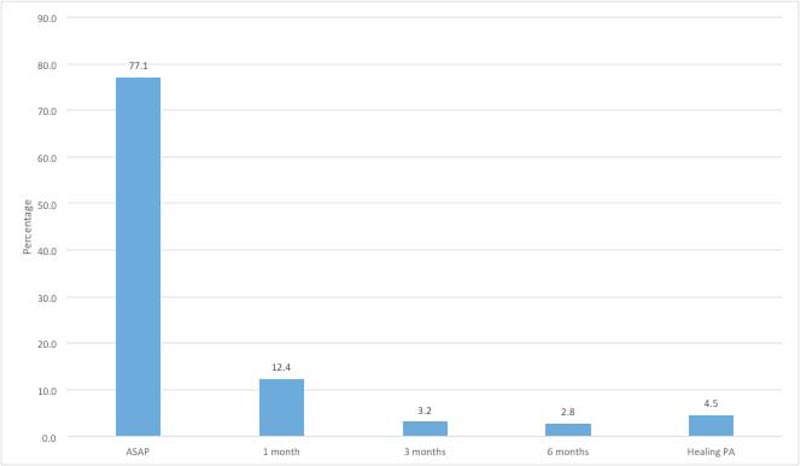
When asked when should an RFT receive a final restoration, the majority of respondents (77.1%) believed that RFT should receive a final restoration as soon as possible after endodontic therapy (Fig. 1). Significantly, a higher percentage of GDPs (P= 0.004), graduates of Asian countries (P<0.001), and who had more than 15 years of experience (P=0.001) believed that RFT should receive a final restoration at least one month after obturation.
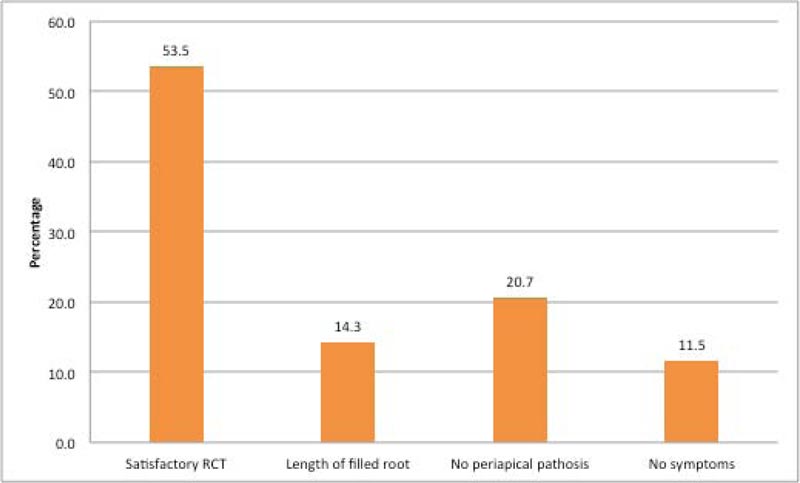
As shown in Fig. (2), respondents thought that satisfactory root canal filling is the most important factor that should be evaluated on a radiograph before canal preparation for a post. This belief was not affected by gender, place of practice, country of graduation, experience, or qualification of respondents.
When asked about the minimum vertical tooth structure required to provide an adequate “ferrule effect”, 64.2%, 23.5%, and 5.7% of respondents thought that it should be 2mm, 1mm, 0.5mm, respectively, while the rest thought that it is not mandatory to have a ferrule. This belief was not affected by gender, place of practice, country of graduation, experience, or qualification of respondents.
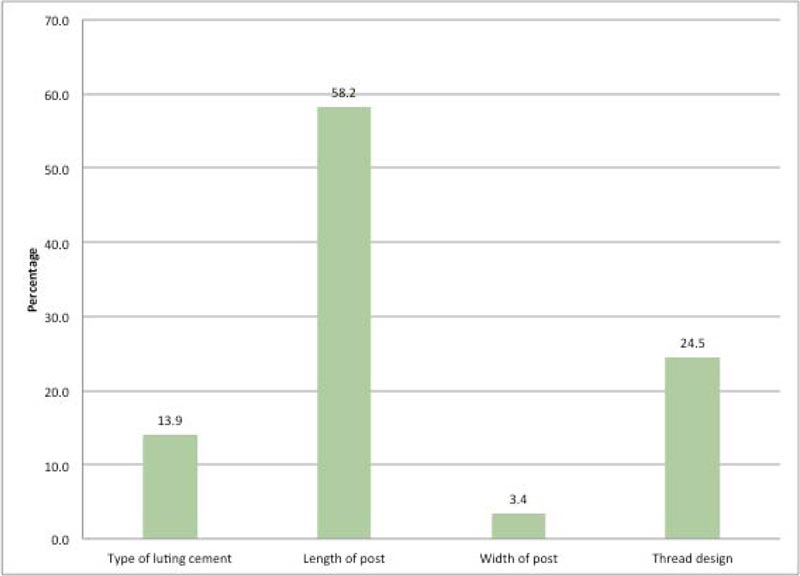
As shown in Fig. (3), respondents thought that the length of the post is the most important factor to ensure the successful retention of a post. However, respondents working at the Ministry of Health (51.6%), and the graduates of Asian countries reported that the thread design of the post is the single most important factor post retention.
3.3. Approaches to Treatment of RFT
As shown in Table 3, the most common approach used by respondents for the restoration of an anterior and premolar RFT was the fiber post and composite build-up, followed by all-ceramic crowns. For anterior teeth, practitioners at RMS used ceramic crowns more frequently compared to other groups, and those working at MH used composite build-up without post more frequently than the other groups.
| Question | Response | % | Gender | Qualification | Country of graduation | Practice location | Experience |
|---|---|---|---|---|---|---|---|
| P-value | |||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure)/ anterior tooth | Composite build-up with no post | 9.7 | NS | NS | NS | 0.01 | NS |
| Fiber post and composite build-up | 59.9 | ||||||
| Cast post and Core | 4.2 | ||||||
| Prefabricated metal post with a build-up | 4.9 | ||||||
| All-ceramic crown | 17 | ||||||
| Metal-ceramic crown | 3.2 | ||||||
| All-ceramic endocrown | 1.2 | ||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure)/premolar tooth | Amalgam build-up with no post | 4.4 | NS | 0.01 | NS | <0.001 | NS |
| Composite build-up with no post | 10.6 | ||||||
| Fiber post and composite build-up | 36.9 | ||||||
| Cast post and Core | 5.4 | ||||||
| Prefabricated metal post with a build-up | 12.4 | ||||||
| All-ceramic crown | 16.4 | ||||||
| Metal-ceramic crown | 10.4 | ||||||
| All-ceramic endocrown | 3.4 | ||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure)/molar tooth | Amalgam build-up with no post | 10.1 | 0.01 | <0.001 | 0.009 | <0.001 | NS |
| Composite build-up with no post | 10.5 | ||||||
| Fiber post and composite build-up | 20.6 | ||||||
| Cast post and Core | 6.1 | ||||||
| Prefabricated metal post with a build-up | 12.8 | ||||||
| All-ceramic crown | 9.9 | ||||||
| Metal-ceramic crown | 23.3 | ||||||
| All-ceramic endocrown | 6.7 | ||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure) for use as bridge abutment/anterior tooth | Composite build-up with no post | 6.6 | NS | NS | NS | NS | NS |
| Fiber post and composite build-up | 51.6 | ||||||
| Cast post and core | 10.1 | ||||||
| Prefabricated metal post and a build-up | 6.6 | ||||||
| All-ceramic retainer with any of the above | 20.9 | ||||||
| Metal ceramic retainer with any of the above restoration | 4.2 | ||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure) for use as bridge abutment/premolar tooth | Amalgam build-up with no post | 4 | NS | NS | NS | NS | NS |
| Composite build-up with no post | 8.4 | ||||||
| Fiber post and composite build-up | 39.1 | ||||||
| Cast post and core | 10.9 | ||||||
| Prefabricated metal post and a build-up | 12 | ||||||
| All-ceramic retainer with any of the above | 16.4 | ||||||
| Metal ceramic retainer with any of the above | 9.2 | ||||||
| Most common approach to restoration of an RFT (with extensive loss of coronal tooth structure) for use as bridge abutment/molar tooth | Amalgam build-up with no post | 11.2 | 0.001 | 0.002 | 0.03 | 0.003 | 0.03 |
| Composite build-up with no post | 8 | ||||||
| Fiber post and composite build-up | 26.3 | ||||||
| Cast post and core | 11.2 | ||||||
| Prefabricated metal post and a build-up | 13.9 | ||||||
| All-ceramic retainer with any of the above | 11.2 | ||||||
| Metal-ceramic retainer with any of the above | 18.3 | ||||||
| How frequently do you plan indirect restorations (e.g., crown) for RFT? | Always (100%) | 7.3 | NS | 0.017 | NS | NS | 0.028 |
| Almost always (more than 75%) | 36 | ||||||
| Often (more than 50% but less than 75%) | 33.9 | ||||||
| Occasionally (more than 25% but less than 50%) | 14.5 | ||||||
| Seldom (more than 0% but less than 25%) | 3.8 | ||||||
| Never | 4.4 |
In the case of premolars, GDPs tend to use composite build-up with or without post less frequently and prefabricated metal posts more frequently than prosthodontists and endodontists. In addition, practitioners working at MH use amalgam build-up without posts and metal-ceramic crowns and those working at RMS use ceramic crowns more frequently than other groups.
For molars, the most common approach used by respondents for restoration of RFT was metal-ceramic crowns, followed by fiber post and composite build-up. However, males, prosthodontists and endodontists, graduates from the Western Europe and USA, and practitioners working at private clinics prefer to use fiber post and composite build-up as their first choice.
When restoring anterior or premolar endodontically treated teeth with extensive loss of tooth structure for use as bridge abutments, respondents preferred mostly fiber post and composite build-up followed by all-ceramic retainers and fiber post and composite build-up followed by metal-ceramic retainers in case of molar teeth. However, in the case of molar teeth, graduates from Asian countries and those working at RMS and MH preferred metal-ceramic retainers as their first choice while the second choice was amalgam build-up with no posts of male practitioners and endodontists, and prefabricated metal posts and build-up of those who had 6-10 years of clinical experience.
As shown in Table 3, a high percentage of respondents were found to plan indirect restorations such as crowns for RFT. Indirect restorations were conducted more often by endodontists and prosthodontists compared to GDPs and by practitioners who had more than 15 years of clinical experience.
3.4. Material Preferences
The majority of respondents preferred fiber posts followed by all-ceramic posts when restoring RFT (Table 4). Fiber posts were used more frequently by graduates from the West Europe and USA, practitioners working at dental schools, and those who had less than 15 years of clinical experience compared to other groups. Graduates from Asian countries used composite cores and amalgam Nayyar cores and practitioners working at RMS used prefabricated metal posts more often than others.
| Question | Response | % | Gender | Qualification | Country of graduation | Practice location | Experience |
|---|---|---|---|---|---|---|---|
| P-value | |||||||
| How frequently do you use any of the following treatments for RFT? | All-ceramic posts | 19 | NS | NS | <0.001 | <0.001 | 0.001 |
| Fiber posts | 55.7 | ||||||
| Cast posts | 3.9 | ||||||
| Prefabricated metal posts | 8.7 | ||||||
| Core material (composite) only | 9.7 | ||||||
| Amalgam Nayyar core | 3.1 | ||||||
| Preferred prefabricated metal post design | Parallel-sided (passive) | 25.2 | NS | <0.001 | 0.002 | <0.001 | NS |
| Tapered (passive) | 32 | ||||||
| Parallel-sided (threaded) | 22.2 | ||||||
| Tapered (threaded) | 20.6 | ||||||
| Optimal length of a post | Equal to crown length | 16.8 | 0.003 | <0.001 | <0.001 | NS | NS |
| Greater than crown length | 15.2 | ||||||
| Half the length of root in bone | 8.6 | ||||||
| Removal of 2/3 of gutta percha filling | 39.1 | ||||||
| Preservation of at least 5 mm of gutta percha | 20.3 | ||||||
| Most frequently used core build-up material | Amalgam | 26.6 | NS | NS | NS | <0.001 | NS |
| Composite resin | 60.7 | ||||||
| Glass ionomer | 6.7 | ||||||
| Silver-modified glass ionomer | 1.8 | ||||||
| Resin-modified glass ionomer | 3.5 | ||||||
| Compomer | 0.6 | ||||||
| Cast post technique used | Direct pattern | 21.9 | NS | <0.001 | NS | NS | 0.004 |
| Indirect method | 28.6 | ||||||
| Not used | 49.6 |
Nearly half of the respondents reported not using cast posts and cores, and if used, a slightly higher percentage of them used the indirect technique for its construction. However, prosthodontists and those who had more than 15 years of clinical experience preferred the direct method for making castings.
With regard to post design, the most frequent type of prefabricated metal posts used by respondents was the tapered passive type (Table 4). However, the preferred type by prosthodontists and endodontists, those practicing at MH and dental schools, and graduates from the West Europe and USA was parallel-sided passive design. Graduates from Asian countries and those practicing at RMS preferred mostly parallel-sided threaded design.
The most common material used by respondents in constructing a core was composite, followed by amalgam. Only a few dentists used glass-ionomer or compomer. However, amalgam was the most common material used for constructing a core by MH practitioners.
3.5. Pre-treatment and Cementation of Posts
Nearly three-quarters of practitioners reported that they treat the prepared post hole before cementing the fiber post (Table 5). The two most common rinsing solutions were phosphoric acid and sodium hypochlorite. Sodium hypochlorite was used less frequently by graduates from the West Europe and USA, more frequently by those who had more than 15 years of clinical experience and it was the most common rinsing solution for those working at MH.
| Question | Response | % | Gender | Qualification | Country of graduation | Practice location | Experience |
|---|---|---|---|---|---|---|---|
| P-value | |||||||
| Preferred cement for metal posts | Zinc phosphate cement | 14.8 | NS | 0.04 | 0.03 | NS | NS |
| Polycarboxylate cement | 9 | ||||||
| Glass Ionomer cement | 49.1 | ||||||
| Resin-modified glass ionomer | 14.2 | ||||||
| Adhesive resin cement | 12.9 | ||||||
| Preferred cementation technique for fiber posts | Acid etch/rinse and dual cure resin | 37.7 | NS | <0.001 | 0.007 | <0.001 | NS |
| Acid etch/rinse and light cure resin | 11.7 | ||||||
| Self-etching/self-adhesive dual cure resin | 28.9 | ||||||
| Self-etching/self-adhesive light cure resin | 5.5 | ||||||
| Resin modified Glass Ionomer | 6.9 | ||||||
| Glass Ionomer | 9.2 | ||||||
| Pre-treatment of radicular dentine (prepared post hole) before cementation of fiber post | Alcohol immersion | 6.4 | NS | NS | 0.01 | 0.001 | 0.046 |
| Chlorohexidine immersion | 5.3 | ||||||
| Sodium hypochlorite | 12.3 | ||||||
| Phosphoric acid rinsing | 36.9 | ||||||
| EDTA | 5.5 | ||||||
| Phosphoric acid rinsing and EDTA | 10.0 | ||||||
| No pre-treatment | 23.6 | ||||||
| Surface treatment of fiber post before cementation | Air abrasion | 5.4 | NS | <0.001 | 0.025 | NS | NS |
| Silane application | 14.8 | ||||||
| Air abrasion/Silane application | 11.0 | ||||||
| Adhesive (dentine bonding agent) application | 23.9 | ||||||
| No pre-treatment | 44.9 |
More than half (55.1%) of respondents reported that they surface treat fiber posts before cementation. The most common surface treatment was applying an adhesive dentine bonding agent and the second most common treatment was silane application. However, silane application was the most common approach used by endodontists, while it was the least common approach used by graduates from Asian countries.
Most practitioners use glass ionomer cement for luting a metal post, followed by zinc phosphate (Table 5). However, the second choice of cement by GDPs was silver-modified glass ionomer and adhesive resin cement was chosen by graduates from other Arab countries. In the case of fiber posts, the most common technique used by respondents was acid etch/rinse and dual cure resin, followed by self-etching/self-adhesive dual cure resin. However, prosthodontists and endodontists, graduates from Asian countries, and those working at dental schools preferred more self-etching/self-adhesive dual cure resin as their first choice cementation technique.
3.6. Failure of RFT with Posts and Cores
When asked the respondents that how often they encounter RFT with cracked coronal tooth structure or fractured roots, 12.1% reported that they encounter cracked coronal tooth structure very often, 29.9% often, 51.4% occasionally, and 6.6% stated that they never encountered such complication. Fractured roots of RFT teeth were seen very often by 2.9%, often by 12.5%, occasionally by 70.8%, and 13.9% stated that they never encountered such an event.
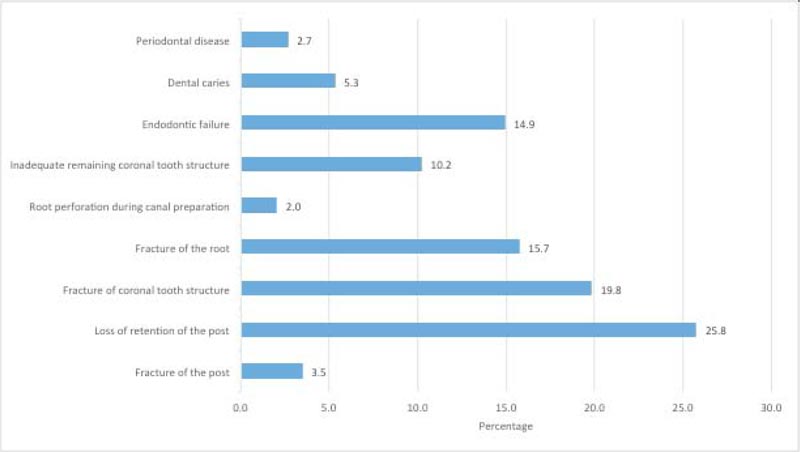
Loss of retention of the post and fracture of coronal tooth structure were the most common reasons for the failure of RFT that has a post and core (Fig. 4). This belief was not affected by factors comprising gender, qualification, country of graduation, place of practice, or years of experience.
4. DISCUSSION
This study aimed to investigate the current opinions and practices of Jordanian dentists when restoring RFT. The response rate (62%) was comparable to similar studies [36, 38] and well above the response rate of two recent surveys regarding the impact of Covid-19 on dental practices in Italy [39, 40]. Thus, the current survey could be considered representative of all Jordanian dental practitioners. Dentists restoring RFT with extensive loss of tooth structure are faced with a plethora of options regarding timing, materials preparation and conditioning techniques when placing definitive restoration after root canal treatment is successfully completed [41]. The majority of dentists who responded to this survey favored restoration of RFT as soon as possible or within less than one month. Providing definitive restoration in a short time span has been shown to yield favorable outcomes [42]. Immediate or within short time span definitive restoration of RFT was also chosen by dentists in Germany [32, 43] and Greece [44]. This might also explain why more endodontists tend to place more posts than both prosthodontists and GDPs.
New adhesive techniques have allowed a more conservative approach, including adhesive direct fillings, partial crowns and endocrowns [7, 45]. In this study, only a minority of dentists contemplated placing a direct restoration only when dealing with RFT with extensive loss of coronal tooth structure. Most dentists reported using a post and core followed by conventional full-coverage metal-ceramic or all-ceramic crowns. More dentists contemplated using endocrowns or onlays when restoring molars compared to premolars or anterior teeth. The presence of more coronal tooth structure available for bonding in molars might explain this trend.
In contrast to Prosthodontists and Endodontists, more GPDs in this study held the belief that restoring RFTs with posts would increase the fracture resistance of those teeth. While this cannot be supported by current evidence, this belief was also shared by more GDPs than restorative specialists in other countries as well [29, 32, 35, 38, 46].
Arguably one of the most important factors when considering favorable prognosis of root treated teeth is the presence of a “Ferrule” [47, 48]. The presence of at least 1.5-2mm of vertical tooth structure circumferentially has a positive effect on the fracture resistance of RFT [49]. This was chosen by almost two-thirds of dentists in this study and was also chosen by a majority of dentists in Sweden [29] and Germany [32].
When restoring RFT anterior teeth, the majority of dentists reported using fiber posts. Fiber posts were still the first choice in premolars and molars to lesser degrees, followed by prefabricated metal posts, while cast metal posts were the least popular to use in all three categories of teeth; anteriors, premolars and molars. Favoring prefabricated fiber and metal posts over cast posts may be attributed to the need for another extra clinical visit when using the latter. This trend was noted in a recent UK survey as well [50]. The popularity of fiber posts use was also reported in another multinational survey [35]. Cast posts tend to perform better when the ferrule is lacking or severely jeopardized [51]. Comparable performance was noted after 5 years of service between cast gold post and core and fiber post and composite core when adequate ferrule was present [52].
More than half of the dentists who regularly use prefabricated metal posts prefer to use active (threaded) posts. In literature, it has been shown that active threading would increase the likelihood of developing cracks inside radicular dentine, thus increasing the chances of root fracture [53]. It has been suggested that active threaded posts should be considered when roots are excessively short or bonding to radicular dentine is not predictable using fiber post or luting a smooth (passive) cast post does not provide enough retention [54, 55].
There was a general tendency to use more extracoronal indirect restoration for posterior RFT when compared to anterior RFT by dentists surveyed in this study. All-ceramic crowns were the preferred choice for anterior and premolar teeth. While dentists surveyed have used more metal-ceramic crowns on molar teeth, they also tended to use endocrowns with no post more in molars when compared to premolars.
When using RFT as bridge abutment, dentists surveyed in this study still favored fiber posts over cast or prefabricated metal post. The choice of material for final FPD was more toward all-ceramic when the RFT retainer was an anterior tooth, and toward metal-ceramic or all-ceramic material when the RFT was a premolar. When a molar RFT was used as an FPD retainer, more dentists preferred to use metal-ceramic material. The tendency to use metal-ceramic bridges in posterior teeth might be attributed to lower costs and easier maintenance. This tendency might also be attributed to the higher loss of porcelain material in veneered zirconia bridges [56].
The adequacy of root filling as evaluated in post obturation radiograph was the main factor that most dentists chose before preparing the canal space for a post. This was in line with European quality guidelines for endodontic treatments [57]. Poor technical quality was also the driving factor to consider retreatment for Jordanian dentists surveyed for the management of asymptomatic RFT with apical periodontitis [58]. A minority of dentists only chose the absence of clinical symptoms as the most important factor to consider when they are preparing canal space to receive a post.
Glass ionomer was the preferred cement to use with metal posts, followed by Zinc phosphate cement. Conventional dual cure resin cement with etch and rinse bonding strategy was predominantly used when bonding fiber posts followed by self-adhesive dual cure resin cement. Self-adhesive bonding strategy is less sensitive technique when compared to etch and rinse which might provide a leeway for the inexperienced dentists [18, 59]. It was found to be used more frequently than etch and rinse conventional cements by respondents in different countries [35]. Although Jordan is one of the courtiers who signed the Minamata convention to phase down amalgam by 2020 [60], this survey showed that 10-15% of respondents are still using amalgam regularly as a core build-up material.
Almost half of the dentists surveyed did not use any pretreatment to fiber posts before cementation, and only a minority of dentists would use an alcohol swap to clean posts before cementation. Interestingly, higher percentages of surveyed dentists use either phosphoric acid etch or sodium hypochlorite to condition posthole space. Sodium Hypochlorite used as the final irrigant was shown to adversely affect the bonding of post to radicular dentine [61-63].
As the majority of dentists surveyed in this study predominantly used fiber posts, the reasons of failure reported by them were mainly associated with fiber posts like loss of retention and fracture of coronal tooth structure. This was similar to the common failures associated with fiber post as reported in the literature [18].
CONCLUSION
It can be concluded that the selection of materials and techniques to restore RFT varies considerably between dentists in Jordan and is not necessarily evidence-based. Further training and continuous education courses might help reduce inconsistencies that have been noted while restoring those teeth.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research project was approved by the ethics committee of the school of dentistry, the University of Jordan, Jordan(201/2019).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Dentists who gave their consent to participate could access and complete the questionnaire via the online link. All responses were anonymous.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


