All published articles of this journal are available on ScienceDirect.
Perception and Attitude of Dental Students and Interns Regarding the Diagnosis and Management of Oral Mucosal Lesions and Salivary Glands Hypofunction
Abstract
Background:
The perception and attitude of dental students/graduates regarding diagnosing/managing oral medicine cases are scarcely investigated.
Objective:
The aim of this investigation was to evaluate the level of confidence in diagnosing/managing cases of oral mucosal lesions and salivary glands hypofunction.
Methods:
A 29-items questionnaire descriptive survey was distributed among dental interns and sixth-year students in the city of Jeddah during March-April of 2020.
Results:
A total of 136 (81 interns and 55 sixth-year students) completed the questionnaire, of which 69.9% were from a government school, and 30.1% were from private schools. For oral mucosal lesions [i.e., aphthous/herpes simplex virus ulceration], the majority of government and private schools’ participants reported being confident in their ability to diagnose (88.4% and 87.8%, respectively) and provide treatment (63.2% and 56.1%, respectively). For oral candidiasis, the majority were confident in their ability to diagnose (government: 95.8%; private: 59.1%) and treat (government: 77.9%; private: 65.9%). The confidence in diagnosing lesions suspicious for dysplasia/premalignancy was high in 77.9% of government and 80.5% of private schools. Similar reporting was found regarding salivary hypofunctions (government: 93.7%; private: 90.2%). For the likeness to refer, the majority of participants were likely to refer to oral medicine, as the 1st choice, followed by oral surgery.
Conclusion:
Dental interns/sixth-year students seemed to have high levels of confidence in diagnosing/managing oral mucosal lesions and salivary hypofunctions. However, the partial participation and the subjectivity of reporting may have hindered capturing the full/precise picture.
1. INTRODUCTION
Oral medicine is defined as a specialty of dentistry focused on the diagnosis and management of oral mucosal lesions, salivary glands dysfunction, and orofacial pain, in addition to dental management of patients with medical complexities [1, 2]. It bridges medicine and dentistry to provide patient care for services not rendered by other specialties.
In 2000, the National Institute of Dental and Craniofacial Research released the Surgeon General’s report highlighting the increased reporting of oral and perioral conditions that, for a long time, remained neglected by dental and medical communities [3]. Oral ulceration, whether infectious, drug-induced or immune-related, are frequent and affect approximately 19% of adults aged 25 to 44 [3, 4]. Moreover, advances in cancer diagnostics and treatment modalities have resulted in an increased number of cancer survivors who require intensive oral care prior to, during, and after their cancer therapy [5].
The rise in demand for oral medicine services has necessitated its stronger presence in dental school curricula [6, 7]. Burzynski et al. surveyed the perception of graduating dental students on oral cancer education in seven dental schools [8]. The results emphasized the lack of knowledge and skills perceived by graduating students that may translate to subsequent deficiency in oral cancer detection and control in the future practice of these dentists [9-12]. Jafer et al. conducted a study concerning dentists’ and dental students’ perception about oral cancer early detection and prevention in Jazan, Saudi Arabia. The study highlighted the lack of dental education and training in this area and discussed how this might negatively impact the ability of dentists to detect/prevent oral cancer in their communities [13]. Few other single-institution studies have investigated dental students’ knowledge and competency in some aspects of oral medications, such as orofacial pain and oral cancer detection [14-16]. Improvement of educational strategies to develop the necessary knowledge and skills in this field was recommended [14-17].
To our knowledge, no large-scale multicenter survey has been previously conducted to evaluate confidence in detecting, diagnosing, and managing patients with common conditions falling within the scope of oral medicine. The aim of this investigation was to evaluate dental students and new dental graduates’ level of confidence in detecting, diagnosing, managing cases of oral mucosal lesions and salivary glands hypofunction.
2. MATERIALS AND METHODS
2.1. Ethical Considerations
Ethical review was conducted in accordance with the Declaration of Helsinki by the Ethical Committee at King Abdulaziz University, Faculty of Dentistry, Jeddah, Saudi Arabia. Approval was obtained from the Ethical Committee after confirmation of compliance (ethical approval number: 32-12-19). Participation in the study was voluntary. A cover letter explaining the study’s purpose, methods, and affirming participants’ anonymity and confidentiality was provided. A consent form was obtained from each participant prior to their enrollment in the study.
2.2. Study Design and Participants
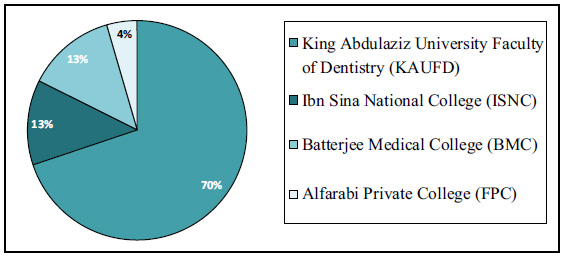
This Cross-sectional study was conducted to evaluate the level of confidence of dental graduates/students in diagnosing and managing/referring cases involving oral mucosal lesions and salivary glands hypofunction. The targeted population included interns and the sixth-year students of the government and private schools in the city of Jeddah, Saudi Arabia (i.e., King Abdulaziz University Faculty of Dentistry (KAUFD), Ibn Sina National College (ISNC), Batterjee Medical College (BMC), Alfarabi Private College (FPC). The study relied on a convenient sample size to maintain voluntary participation.
2.3. Inclusion and Exclusion Criteria
Inclusion criteria included interns and sixth-year dental students of the government and private schools in the city of Jeddah, Saudi Arabia, willingness to participate in the study voluntarily, and signing the consent form prior to filling out the questionnaire. Exclusion criteria involved those who participated in the face validity and content validity testing.
2.4. Questionnaire’s Face Validity and Content Validity Testing
A self-administered 29-item questionnaire was constructed using Google survey forms. Face validity and content validity were tested by two dental interns from KAUFD who were chosen to take the survey prior to its distribution. The questionnaire was edited based on the feedback received to ensure clarity and readability.
2.5. Questionnaire Distribution and Data Collection
The questionnaire was distributed to the targeted population via their institutions’ emails in the period between March and April 2020. To ensure blinding of the study investigators and elimination of selection bias, all e-mail addresses for eligible potential participants were pooled together into one mailing list and sent all at once. Data provided by the study participants were automatically populated into an excel sheet to avoid any confirmation bias.
A reminder e-mail was sent two weeks after the distribution of the first recruitment e-mail to encourage/remind those who did not complete the survey. Collected data was instantly populated from the Google Survey forms to an encrypted online Excel form that could be accessed only by the investigators in this study. Data was transferred automatically, as a whole, to the online Excel form with no further manipulation to eliminate the chance of confirmation, interpretation, or prediction biases.
2.6. Questionnaire Details
The 29-item questionnaire composed of written questions with simplified language was distributed to all eligible potential participants. To avoid guiding the participants and/or influencing their answers, no images for the oral mucosal lesions or the salivary glands hypofunctions were provided. Participants were asked to provide information about their demographic as well as their didactic and clinical exposure to oral mucosal lesions and salivary glands hypofunction topics/cases. Afterward, participants were requested to rank their level of confidence in detecting, diagnosing, and managing these cases using a five-point Likert scale (i.e., extremely confident, confident, somewhat confident, not so confident, not at all confident). Furthermore, participants were asked about the likeliness of them treating versus referring the aforementioned cases after graduation and if they know to whom to refer to.
2.7. Data Management and Analysis
Frequencies of responses were calculated, and comparisons of frequencies of the main outcomes were made using the chi-square test using SPSS software version 2.0. P-values of less than 0.05 were considered statistically significant. Blinding of the study groups was ensured during data analysis to eliminate the chance of bias.
3. RESULTS
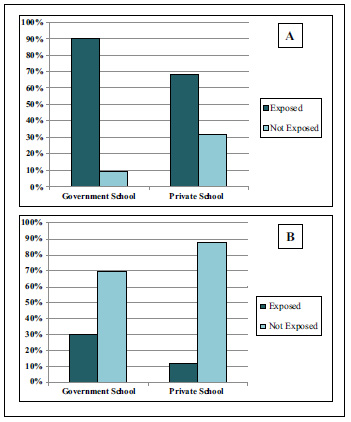
A total of 136 participants, 81 interns (59.6%) and 55 sixth-year dental students (40.4%), completed the questionnaire. Among those, 95 (69.9%) were from a government school (KAUFD) and 41 (30.1%) were from private schools distributed between ISNC (n=17; 12.5%), BMC (n=18; 13.2%), and FPC (n=6; 4.4%) (Fig. 1). Females constituted 51.5% of the participants, while 48.5% were males, with the majority being 24 (43.4%) and 25 years old (31.6%) (Table 1). Exposure to clinical cases of oral mucosal lesions was highly reported in participants from government and private schools, while exposure to cases with salivary glands hypofunction was reported to be low in both groups (p=0.003 and p=0.04, respectively) (Fig. 2a and b).
The majority of participants from both government and private schools reported that the third year was the time when didactic courses concerning oral mucosal lesions (52.6% and 65.9%, respectively) and salivary gland dysfunction (43.2% and 56.1%, respectively) were provided (Table 2). The level of confidence in the ability to diagnose cases of oral mucosal lesions, such as recurrent minor aphthous ulceration or oral herpetic infection, was high in the majority of government school participants (88.4%) as well as private schools’ participants (87.8%). While 63.2% of government school participants and 56.1% of private school participants reported the likeliness to provide the treatment themselves, the majority of both also preferred referring to specialists (73.7% and 78.0%, respectively). In terms of referral to specialists, oral medicine was the first choice selected by both government (84.2%) and private (90.2%) schools’ participants, followed by referral to oral surgery or preference to treat the patients themselves (Table 3).
| Variables |
Government Dental School N = 95 (69.9%) |
Private Dental Schools N = 41 (30.1%) |
Overall N=136 (100%) |
||
| Institution | KAU | 95 (100%) | -- | 95 (69.9%) | -- |
| ISNC | -- | 17 (41.5%) | 17 (12.5%) | ||
| BMC | -- | 18 (43.9%) | 18 (13.2%) | ||
| FBC | -- | 6 (14.6%) | 6 (4.4%) | ||
| Gender | Male | 52 (54.7%) | 14 (34.1%) | 66 (48.5%) | -- |
| Female | 43 (45.3%) | 27 (65.9%) | 70 (51.5%) | ||
| Age | 23 | 16 (16.8%) | 8 (19.5%) | 24 (17.6%) | -- |
| 24 | 46 (48.4%) | 13 (31.7%) | 59 (43.4%) | ||
| 25 | 27 (28.4%) | 16 (39.0%) | 43 (31.6%) | ||
| 26 | 3 (3.2%) | 2 (4.9%) | 5 (3.7%) | ||
| >27 | 3 (3.2%) | 2 (4.9%) | 5 (3.7%) | ||
| Current year in Dental School | Internship | 62 (65.3%) | 19 (46.3%) | 81 (59.6%) | 0.061 |
| Sixth year | 33 (34.7%) | 22 (53.7%) | 55 (40.4%) | ||
| Exposed to clinical cases with Oral mucosal lesions | No | 9 (9.5%) | 13 (31.7%) | 2 (16.2%) | 0.003 |
| Yes | 86 (90.5%) | 28 (68.3%) | 114 (83.3%) | ||
| Exposed to clinical cases with Salivary gland dysfunction | No | 66 (69.5%) | 36 (87.8%) | 102 (75.0%) | 0.04 |
| Yes | 29 (30.5%) | 5 (12.2%) | 34 (25.0%) | ||
| Variables | Levels |
Government Dental School N = 95 (69.9%) |
Private Dental Schools N = 41 (30.1%) |
| Year started classes in Oral mucosal lesions | 2nd Year | 0 (0.0%) | 3 (7.3%) |
| 3rd year | 50 (52.6%) | 27 (65.9%) | |
| 4th year | 35 (36.8%) | 9 (22.0%) | |
| 5th year | 10 (10.5%) | 2 (4.9%) | |
| Year started classes in Salivary gland dysfunction | 2nd Year | 3 (3.2%) | 0 (0.0%) |
| 3rd year | 41 (43.2%) | 23 (56.1%) | |
| 4th year | 26 (27.4%) | 15 (36.6%) | |
| 5th year | 25 (26.3%) | 3 (7.3%) |
Regarding the ability to diagnose cases of oral candidiasis, the majority of the government school participant was confident (95.8%), as well as those of private schools (95.1%). In addition, 77.9% of government school and 65% of private school participants were likely to provide treatment. However, the majority of government and private school participants were also likely to refer (61.1% and 73.2%, respectively). The first choice for the specialist to refer to was oral medicine in both government (77.9%) and private school participants (80.5%) (Table 3).
For cases of oral lichen planus or lichenoid reaction, high confidence in the ability to diagnose was reported by the majority of government school participants (84.2%) as well as private school participants (92.7%). Regarding the likeliness to provide treatment, 34.7% of the government school participants were “not sure,” followed by 33.7% who reported the unlikeliness to treat. On the other hand, 46.3% of the private school participants were likely to provide treatment, followed by 43.9% who were “not sure”. In terms of referral, both government and private school participants were likely to refer (82.1% and 73.2%, respectively). The first choice for the specialist to refer to was oral medicine in both government (91.6%) and private school participants (90.2%) (Table 3).
For the ability to diagnose cases with a white lesion suspicious for dysplasia/premalignancy, the majority of government and private school participants reported being confident (77.9% and 80.5%, respectively). Moreover, both government and private schools’ participants were likely to refer (75.8% and 73.2%, respectively). Oral medicine was the first choice selected by both government (87.4%) and private (85.4%) schools’ participants, followed by oral surgery (Table 3).
For the ability to diagnose cases with xerostomia and/or suspected salivary gland hypofunction, the reporting of confidence in government and private schools’ participants was high (93.7% and 90.2%, respectively). More than half of the participants were likely to provide the treatment themselves (61.1% from government and 63.4% from private schools) while the majority preferred to, contradictorily, refer to specialists (78.9% of government and 73.2% from private schools). Oral medicine was the first choice to refer to for both government and private schools’ participants (75.8% and 73.2%, respectively) (Table 3).
Investigating the level of confidence in performing diagnostic tests showed that 44.2% of the government school’s participants were confident in obtaining oral cytology to detect dysplastic tissues while 55.8% were not. On the other hand, 61% of the private schools’ participants were confident while 39% were not. For obtaining a fungal smear to detect oral candidiasis, approximately half of the participants reported being confident (52.6% of government and 56.1% of private schools’ participants). In regard to salivary flow testing (i.e., sialometry to detect cases of salivary hypofunction), 68.4% of government and 63.4% of private schools’ participants were confident (Table 4).
| Variables |
Government Dental School N (%) |
Private Dental Schools N (%) |
Government Dental School N (%) |
Private Dental Schools N (%) |
Government Dental School N (%) |
Private Dental Schools N (%) |
||||
| Ability to diagnose | Confident | Minor aphthous ulceration or oral herpetic infection | 84 (88.4%) | 36 (87.8%) | Oral candidiasis or denture stomatitis | 91 (95.8%) | 39 (95.1%) | Salivary gland hypofunction | 89 (93.7%) | 39 (95.1%) |
| Not confident | 11 (11.6%) | 5 (12.2%) | 4 (4.2%) | 2 (4.9%) | 6 (6.3%) | 2 (4.9%) | ||||
| Likeliness to treat | Likely | 60 (63.2%) | 23 (56.1%) | 74 (77.9%) | 27 (65.9%) | 58 (61.1%) | 27 (65.9%) | |||
| Unlikely | 10 (10.5%) | 0 (0.0%) | 7 (7.4%) | 1 (2.4%) | 14 (14.7%) | 1 (2.4%) | ||||
| Not sure | 25 (26.3%) | 18 (43.9%) | 14 (14.7%) | 13 (31.7%) | 23 (24.2%) | 13 (31.7%) | ||||
| Likeliness to refer | Likely | 70 (73.7%) | 32 (78.0%) | 58 (61.1%) | 30 (73.2%) | 75 (78.9%) | 30 (73.2%) | |||
| Unlikely | 8 (8.4%) | 2 (4.9%) | 19 (20%) | 2 (4.9%) | 4 (4.2%) | 2 (4.9%) | ||||
| Not sure | 17 (17.9%) | 7 (17.1%) | 18 (18.9%) | 9 (22%) | 16 (16.8%) | 9 (22%) | ||||
| 1st choice for referral | OM | 80 (84.2%) | 37 (90.2%) | 74 (77.9%) | 33 (80.5%) | 72 (75.8%) | 33 (80.5%) | |||
| OS | 3 (3.2%) | 3 (7.3%) | 1 (1.1%) | 4 (9.8%) | 6 (6.3%) | 4 (9.8%) | ||||
| PCP | 3 (3.2%) | 0 (0.0%) | 4 (4.2%) | 0 (0.0%) | 7 (7.4%) | 0 (0.0%) | ||||
| ENT | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.1%) | 0 (0.0%) | ||||
| Not sure | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.1%) | 0 (0.0%) | ||||
| Myself | 9 (9.5%) | 1 (2.4%) | 16 (16.8%) | 4 (9.8%) | 8 (8.4%) | 4 (9.8%) | ||||
| 2nd choice for referral | OM | 11 (11.6%) | 5 (12.2%) | 19 (20.0%) | 10 (24.4%) | 20 (21.1%) | 10 (24.4%) | |||
| OS | 53 (55.8%) | 32 (78.0%) | 37 (38.9%) | 23 (56.1%) | 46 (48.4%) | 23 (56.1%) | ||||
| PCP | 9 (9.5%) | 2 (4.9%) | 12 (12.6%) | 2 (4.9%) | 11 (11.6%) | 2 (4.9%) | ||||
| ENT | 2 (2.1%) | 0 (0.0%) | 1 (1.1%) | 1 (2.4%) | 2 (2.1%) | 1 (2.4%) | ||||
| Not sure | 5 (5.3%) | 2 (4.9%) | 6 (6.3%) | 1 (2.4%) | 8 (8.4%) | 1 (2.4%) | ||||
| Myself | 15 (15.8%) | 0 (0.0%) | 20 (21.1%) | 4 (9.8%) | 8 (8.4%) | 4 (9.8%) | ||||
| Ability to diagnose | Confident | Oral lichen planus or lichenoid reaction | 80 (84.2%) | 38 (92.7%) | White lesion suspicious for dysplasia/premalignancy | 74 (77.9%) | 33 (80.5%) | |||
| Not confident | 15 (15.8%) | 3 (7.3%) | 21 (22.1%) | 8 (19.5%) | ||||||
| Likeliness to treat | Likely | 30 (31.6%) | 19 (46.3%) | -- | -- | |||||
| Unlikely | 32 (33.7%) | 4 (9.8%) | -- | -- | ||||||
| Not sure | 33 (34.7%) | 18 (43.9%) | -- | -- | ||||||
| Likeliness to refer | Likely | 78 (82.1%) | 30 (73.2%) | 72 (75.8%) | 30 (73.2%) | |||||
| Unlikely | 8 (8.4%) | 0 (0.0%) | 6 (6.3%) | 1 (2.4%) | ||||||
| Not sure | 9 (9.5%) | 11 (26.8%) | 17 (17.9%) | 10 (24.4%) | ||||||
| 1st choice for referral | OM | 87 (91.6%) | 37 (90.2%) | 83 (87.4%) | 35 (85.4%) | |||||
| OS | 1 (1.1%) | 3 (7.3%) | 7 (7.4%) | 5 (12.2%) | ||||||
| PCP | 1 (1.1%) | 1 (2.4%) | 2 (2.1%) | 0 (0.0%) | ||||||
| ENT | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||||
| Not sure | 1 (1.1%) | 0 (0.0%) | 1 (1.1%) | 1 (2.4%) | ||||||
| Myself | 5 (5.3%) | 0 (0.0%) | 2 (2.1%) | 0 (0.0%) | ||||||
| 2nd choice for referral | OM | 15 (15.8%) | 4 (9.8%) | 15 (15.8%) | 9 (22.0%) | |||||
| OS | 48 (50.5%) | 33 (80.5%) | 62 (65.3%) | 26 (63.4%) | ||||||
| PCP | 12 (12.6%) | 3 (7.3%) | 8 (8.4%) | 1 (2.4%) | ||||||
| ENT | 2 (2.1%) | 1 (2.4%) | 1 (1.1%) | 1 (2.4%) | ||||||
| Not sure | 11 (11.6%) | 0 (0.0%) | 7 (7.4%) | 3 (7.3%) | ||||||
| Myself | 7 (7.4%) | 0 (0.0%) | 2 (2.1%) | 1 (2.4%) | ||||||
When comparing the level of confidence in performing diagnostic tests in interns versus sixth-year students, regardless of their institutions, only 50.6% of the interns and 47.3% of the sixth-year students reported confidence in performing oral cytology to detect dysplastic tissues. Similarly, 54.3% of interns and 52.7% of sixth-year students reported confidence in performing fungal smear tests to detect oral candidiasis. For salivary flow testing (i.e., sialometry to detect cases of salivary hypofunction), 69.1% of interns and 63.6% of sixth-year participants were confident (Table 5). Another interesting finding was the likeliness of treating oral mucosal lesions, such as oral lichen planus, where 47.3% of sixth-year students from all institutions were more likely to treat compared to 28.4% of interns.
| Level confidence in performing diagnostic tests |
Government Dental School N = 95 (69.9%) |
Private Dental Schools N = 41 (30.1%) |
P-value | |
| Oral cytology (including brush biopsy) to detect dysplastic tissues | Confident | 42 (44.2%) | 25 (61.0%) | 0.11 |
| Not confident | 53 (55.8%) | 16 (39.0%) | ||
| Fungal smear to detect oral candidiasis | Confident | 50 (52.6%) | 23 (56.1%) | 0.85 |
| Not confident | 45 (47.4%) | 18 (43.9%) | ||
| Salivary flow testing (sialometry) to detect cases of salivary hypofunction | Confident | 65 (68.4%) | 26 (63.4%) | 0.71 |
| Not confident | 30 (31.6%) | 15 (36.6%) | ||
| Level Confidence in Performing Diagnostic Tests |
Interns N = 81 (59.6%) |
6th Year Students N = 55 (40.4%) |
P-value | |
| Oral cytology (including brush biopsy) to detect dysplastic tissues | Confident | 41 (50.6%) | 26 (47.3%) | 0.84 |
| Not confident | 40 (49.4%) | 29 (52.7%) | ||
| Fungal smear to detect oral candidiasis | Confident | 44 (54.3%) | 29 (52.7%) | 0.99 |
| Not confident | 37 (45.7%) | 26 (47.3%) | ||
| Salivary flow testing (sialometry) to detect cases of salivary hypofunction | Confident | 56 (69.1%) | 35 (63.6%) | 0.63 |
| Not confident | 25 (30.9%) | 20 (36.4%) | ||
4. DISCUSSION
Developing comprehensive dental education and training curriculum that serves the community’s needs and extends its focus beyond the mechanical aspects of dental management is fundamental. Dental schools’ curricula must embrace the concept of bridging between medicine and dentistry to positively influence the behavior and management decisions taken by dentists when providing dental care for their patients. Oral medicine is the specialty that brings medicine to dentistry and ensures that dental care extends beyond “teeth and their supporting structures.” It is quite important to assess the dental schools’ curricula in oral medicine and ensure their capability of providing the adequate knowledge and training that boosts the confidence of dental graduates to diagnose, manage and/or refer oral medicine cases that may be encountered in general dental practice.
The result of the present study showed that sixth-year dental students and dental interns from both government and private dental schools in the city of Jeddah, Saudi Arabia, have generally reported high levels of confidence in diagnosing and managing oral mucosal lesions and salivary glands hypofunctions. This finding was applicable to their ability to diagnose cases of oral mucosal lesions such as recurrent minor aphthous ulceration, oral herpetic ulcers, oral lichen planus, oral candidiasis, suspicious dysplastic/potentially malignant lesions, and salivary glands hypofunction. This comes in contrast to what was reported in the study by Burzynski et al., who reported a lack of knowledge and skills perceived by graduating students regarding oral cancer detection [8]. Cerero Lapiedra et al. also suggested the need to increase the focus on cancer education in the dental curriculum to enhance students’ skills in identifying potentially malignant disorders [14]. Joseph et al. assessed oral cancer knowledge among undergraduate dental students and demonstrated the need for organized teaching programs [15]. The authors stressed that dental curricula should focus on helping the students identify the risk factors and the early signs of oral cancer by performing a thorough routine oral examination and knowing when to refer the patient for appropriate management [15].
This current study showed that more than half of the participants from government and private schools had reported high confidence in the likeliness of treating the aforementioned cases by themselves, except for lichen planus and oral lichenoid reaction. However, a significant number of study participants still reported the likeliness of referring patients to a specialist. The answers seem contradictory and should be interpreted with precaution. This contradiction indicates either the lack of understanding of the specific purpose of the survey or the avoidance of reporting their true level of confidence due to bias toward their own institutions or other personal, cultural, or social barriers. The high confidence in treating patients, reported by participants in this study, comes in contrast to the reporting by Doshi et al., where lower levels of confidence of junior doctors in managing oral conditions were illustrated [18]. Moreover, a study by Keat et al. showed that medical students might benefit from additional teaching on oral cancer [19]. In our community, the need to incorporate oral health training into the teaching programs for junior dentists to improve their confidence in the diagnosis and management of oral conditions is of great importance. However, the lack of transparent feedback and constructive critique from dental students and young graduates may hinder the educators’ ability to promote both didactic and clinical training curricula.
In terms of referring cases to specialists, the majority of both groups reported that oral medicine would be the first choice for referral, while referral to primary care physicians and otolaryngology were the least option to be chosen. A previous investigation by Friesen et al. demonstrated that the referral patterns of dental and medical practitioners are similar, with mucosal lesions being the most common referral reason [16]. Scully et al. showed that awareness of correct specialty to refer to could help optimize patient management, particularly for those with malignant or potentially malignant disorders or complicated/serious non-malignant conditions such as HIV or pemphigus vulgaris [17].
One important finding in this study was the reporting of low exposure to salivary gland dysfunction cases by both government and private schools’ participants. This unexpected finding suggests the need for modifying the current curricula to provide further concentration on the clinical management of patients with hyposalivation. Another important finding was the likeliness of treating oral mucosal lesions, such as oral lichen planus, where sixth-year students from all institutions were more likely to treat compared to interns. This might be due to the presence of oral medicine faculties on the floor with the sixth-year dental students, which provides an extra level of assurance and increases their confidence. One last interesting finding in this analysis was the high confidence that all interns and sixth-year students from all the institutions reported regarding performing diagnostic tests, except the oral cytology (brush biopsy), where private school participants reported higher confidence. No previous studies have reported investigating the students/recent dental graduates’ confidence in this specific matter. This finding should be interpreted with caution as subjectivity and personal biases may skew the results of the questionnaire.
4.1. Study Limitations and Future Directions
The imitations of this study included the partial participation of interns and sixth-year dental students from all institutions, which hindered capturing the full picture. Moreover, the significantly smaller numbers of participants from private schools have obligated the investigators to pool all private schools’ data in one arm, rather than having independent comparison arms for every institution.
In addition, the inevitable subjective reporting in such a survey was vulnerable to a high risk of bias. The tendency of students to provide positive reporting regarding their institutions might be due to the competitivity between schools and the natural eagerness of the students to satisfy their faculties and institutions. Furthermore, the mindset of the dental students and recent graduates that has been programmed to provide the best and/or correct answers, rather than truly expressing their opinions, might have also influenced the responses to this questionnaire.
CONCLUSION
The purpose of the current study was to determine the level of confidence of sixth-year students and dental interns in both government and private dental schools in the city of Jeddah, Saudi Arabia. The study concluded that sixth-year dental students and dental interns had reported high levels of confidence in diagnosing/managing oral mucosal lesions and salivary glands hypofunction cases. Interestingly, although the reporting of “likeliness to treat” was high, the likeliness of referring to a specialist was also high, which was somehow contradictory. Thus, results should be interpreted with skepticism due to subjectivity and the high probability of bias.
RECOMMENDATION
Such a survey would be fruitful for further future investigations in other cities and universities in Saudi Arabia to ensure the effectiveness of their oral medicine curricula. An introductory study session might be needed in future investigations to ensure participants have a full understanding of the purpose of the survey and decrease the chance of receiving biased answers that may mask valuable results needed to improve dental schools’ curricula. Furthermore, providing a pre-test to assess the participants’ knowledge in oral mucosal lesions and salivary glands hypofunction may be considered in the future. This will highlight if the level of confidence in detecting, diagnosing, and managing the aforementioned conditions corresponds to the level of knowledge.
AUTHORS’ CONTRIBUTIONS
All persons designated as authors qualify for authorship and have checked the article for plagiarism. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
AMF was responsible for conceptualization, methodology, validation, supervision, and writing (reviewing and editing). MAH took part in the investigation and was responsible for writing the original draft of the manuscript. MAA also took part in the investigation as well as wrote the original draft of the manuscript. GAT took part in the investigation and conducted the formal analysis/validation, as well as reviewed and edited the manuscript.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Approval was obtained from the Ethical Committee at King Abdulaziz University, Faculty of Dentistry, Jeddah, Saudi Arabia, after confirmation of compliance on the third of March 2020 (ethical approval number: 32-12-19).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The questionnaire was accompanied by a consent form cover letter explaining the study’s purpose and methods and reassuring respondents of the survey’s confidentiality. Participation in the study was voluntary, and consent was obtained from each participant prior to accessing the questionnaire.
STANDARDS OF REPORTING
STROBE Guideline and methodology were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the KAU Google Drive at https://docs.google.com/docu ment/d/15ET0FL_2KdUuG8I7Hsl__KogA2J6hlDE/edit?usp=sharing&ouid=105500621813379395369&rtpof=true&sd=true.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Ross Kerr, Dr. Jaisri R. Thoppay, Dr. Ying Wu, Dr. David Dean, Dr. Rania Younis, and Dr. Bhavik Desai for their contribution in the development of the questionnaire used in this investigation and intended to survey attitude and perception of dental students nationally and internationally.


