All published articles of this journal are available on ScienceDirect.
Predictability of Root Movements Using Virtual Root Setup in a Patient With Periodontal Disease Treated With Clear Aligners
Abstract
Aims:
The aim of the study was to show a case with a midline diastema in a patient with high periodontal risks and gingival recessions treated with clear aligners. The objective was to predict and quantify root movements using a dedicated software that extrapolates data from the Cone Beam Computed Tomography (CBCT).
Case Presentation:
A 31-year-old female with a mandibular midline diastema asked for an aesthetic treatment. She had vertical bone loss on the lower central incisors, so a CBCT was necessary in order to plan the root movements. The purpose of the treatment was to avoid an uncontrolled tipping of the incisors and, therefore, a vestibular movement of the roots, which could cause serious periodontal problems.
Conclusion:
At the end of the treatment, the complete closure of the diastema and the radiographic healing of the vertical bone loss between mandibular central incisors were achieved. The superimpositions with the virtual setup demonstrated predictability of root movements of 76%.
1. INTRODUCTION
Nowadays, the majority of adult patients require orthodontic treatments, especially aesthetic treatments [1]. It is necessary to carefully evaluate the patient's periodontal conditions, particularly in adults, because in the case of bone resorption the position of the center of resistance along the root of the tooth changes and this influences the type of orthodontic force that must be applied to the tooth to obtain the expected movement. The displacement of the center of resistance towards the root apex causes a torque increase, which further aggravates the destruction of periodontal tissues [2]. In this regard, in periodontal compromised patients, it would be very important to predict the movements of the roots, which is not possible using the standard software for the clear aligners treatment setup, which allow to visualize only the movements of the dental crowns. Therefore, adult patients with periodontitis should be treated with light force to maintain the health and stability of the periodontal environment [3].
The mandibular diastema is not a normal growth characteristic. It occurs less frequently than a maxillary diastema, but it is often more dramatic. The primary etiologic factor in mandibular diastemas is tongue thrust in a low rest position, or it can be due to a self-inflicted pathology by tongue piercing [4]. A midline diastema may compromise smile attractiveness and dentofacial harmony [5], but not all diastemas can be treated the same in terms of modality or timing [6].
This paper suggests a method to close midline diastema in a patient with high periodontal risks and gingival recessions, and to predict and quantify root movements using clear aligners. The conventional aligners virtual treatment plan shows only crown movements and not root movements. Differently, this study aimed to assess the accuracy of tooth movement when using clear aligners. In this treatment, there was a need to absolutely control the movements of the teeth in order to avoid uncontrolled root movements that could lead to the loss of these teeth.
The effectiveness of fixed appliances to apply root torque is the key to a successful treatment, while one employing clear aligners to move roots to designated positions has not been confirmed. Zhang et al. [7] showed that clear aligners could not perform bodily movements because they mostly move the teeth by uncontrolled tipping. They reported that the material properties of clear aligners are probably responsible for their inability to apply torque.
1.1. Patient Information
A 31-year-old female patient with a mandibular midline diastema was referred by her general dentist (Fig. 1). She explained that the diastema was due to the pressure of a tongue piercing, which was later removed, and she expressed the will to receive an esthetic orthodontic treatment only in the lower arch, despite the suggestion to treat both arches to correct the bilateral cross bite.

1.2. Clinical Findings
The patient showed a large inter-incisive diastema between 3.1 and 4.1, a class I molar and canine relationship and canine, premolar and molar cross bite on the right, molar cross bite on the left. Vestibular gingival recessions were visible on 3.1 and 4.1.
1.3. Diagnostic Assessment
At the first appointment, all data were collected: intra and extra oral photos and the CBCT that also showed a vertical bone loss between the lower central incisors. It was decided to perform an initial CBCT to radiographically assess the patient's bone condition, considering the clinically evident recessions. Vertical defects were considered a sign of progressive or advanced disease and were associated with further periodontal bone loss and tooth loss [8].
1.4. Therapeutic Intervention
The therapeutic alternatives were to choose between clear aligner therapy and lingual orthodontic treatment. The patient preferred a removable choice.
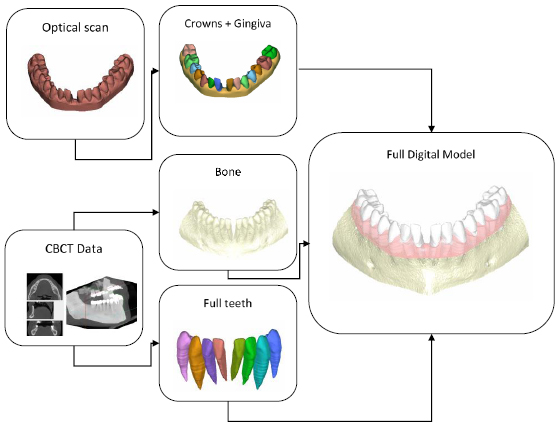
Clear aligner therapy was planned to move only the lower anterior teeth and it was predicted to close the central incisor diastema, align and rotate the lower incisors and canines and produce a lingual movement of these teeth. Moreover, the initial CBCT was matched with the scan of the orthodontic models and the result was used to include the dental roots in the orthodontic setup in order to predict the roots’ movements too (Fig. 2). This possibility permitted us to reach a more precise prediction of the movements of the teeth, including the position of the roots. The purpose of the treatment was to avoid an uncontrolled tipping of the incisors and, therefore, a vestibular shift of their roots that could cause serious periodontal problems.

To provide mechanical retention and support for the desired rotation, vestibular attachments were planned on canines and first premolars, and pressure points on the lingual side of canines.
Thirty-two aligners were delivered for the initial treatment phase. After one year of treatment, it was decided to call for a refinement of eight aligners with the addition of vertical rectangular attachments on the lower incisors to intrude them.
2. MATERIALS AND METHODS
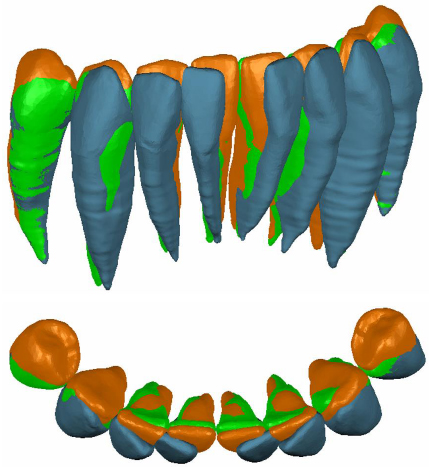
The digital model of the patient’s mouth anatomy was obtained by combining digital impressions with 3D data from a Cone Beam Computer Tomography (CBCT). The methodology used allowed for the merging of these multi-source data to obtain full tooth anatomies including crown and root shapes, the gingiva’s anatomy and maxillary/mandibular bone anatomies. Highly accurate crown and gingiva geometries were obtained from optically scanned data that allowed the best resolution and accuracy, while root geometries were obtained by processing CBCT data (Fig. 3) Digital model acquisition flow.
2.1. Optical Scan
In this study, an optical scanner was used to acquire the patient’s visible anatomies by means of plaster models obtained from impressions. An accurate digital mouth model of both crown shapes and gingival tissue was obtained. The model was then subdivided into disconnected regions, which represented the crowns and the gingiva. The subdivision was carried out by a semi-automated segmentation procedure, which exploited the curvature of the digital mouth model [9].
2.2. CBCT Scan
CBCT produces volumetric data that represents a stack of slices corresponding to cross-sections through a maxillofacial volumetric region, where each slice is an image of grey intensity values corresponding to the x-ray attenuation through the crossed anatomical tissues. CBCT data are stored in a sequence of Digital Imaging and Communications in Medicine (DICOM) images that contains geometric information of the bone structure as well as the complete tooth geometries.
The 3D model of the bone was obtained by segmentation tools provided by an open-source software for medical image analysis [3DSlicer: A multi-platform, free and open-source software package for visualization and medical image computing. http://www.slicer.org/]. The obtained model represented the isosurface of the volumetric data corresponding to a specific grey intensity threshold value. The model contained the mandibular bone and all the teeth of the inferior arch. The final bone model was obtained by a Boolean subtractive operation, once the individual models of the teeth were obtained.
2.3. Individual Tooth Model Extraction
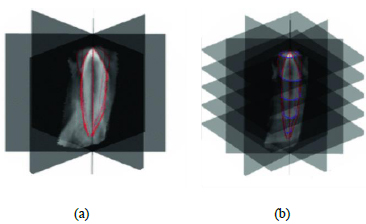
The individual tooth anatomies are not so simple to extract from tomographic data because of similar grey intensity values of the tooth root and surrounding bone tissue. Slice-by-slice segmentation procedures are commonly used for this purpose, but this can result in processing hundreds of slices in order to obtain segmented models, thus leading to time-consuming procedures. In this case, DICOM images were processed by adopting the methodology introduced in the paper by Barone et al. [10]. This method is based on processing a subset of images (reformation images) for each tooth on the basis of anatomy-driven considerations. The reformation images allowed us to easily obtain the tooth geometry by using a limited set of 2D curves representing the contour of the tooth in each image. Indeed, four reference planar sections were automatically obtained. These reference sections were used to outline the tooth by tracing four different 2D curves that represented the tooth contours (Fig. 4a). The four contours were used to automatically extract a series of closed curves on each slice perpendicular to the tooth axis (transverse slice) (Fig. 4b).
This methodology allowed us to rapidly extract the geometry of a full tooth by means of manually processing a few automatically extracted images from CBCT data. The processing time was significantly lowered compared to common manual standard methods.
2.4. Full Anatomical Model
The 3D models obtained by using optical and tomographic scans had to be merged into one model in order to allow treatment planning. First of all, different models are needed to be aligned in a common reference system. The optical 3D models were coarsely aligned with the corresponding models from the CBCT data set (e.g., manually selecting at least three common points or by manually moving the 3D models), and successively, the obtained alignment was refined by means of a registration algorithm (best fine alignment or Iterative Closest Point technique). The final model of the teeth was obtained by merging optically scanned crowns with root data from CBCT. This provided fully closed models composed of the most accurate representation for tooth crowns. Thus, the final anatomical digital model was composed of these teeth, the gingiva from the optical scan and the bone from the CBCT.
For each tooth, axes and principal points were identified. The z-axes according to Di Angelo et al. [11] were defined approximately perpendicular to the occlusal plane and associated with the lower moment of inertia of its geometrical model. The mesiodistal (y-axis) and the buccolingual (x-axis) directions were set orthogonal to the z-axis, while the apex and principal points (two for incisors and one for canines and premolars) were defined as depicted in Fig. (5).
3. FOLLOW-UP AND OUTCOMES
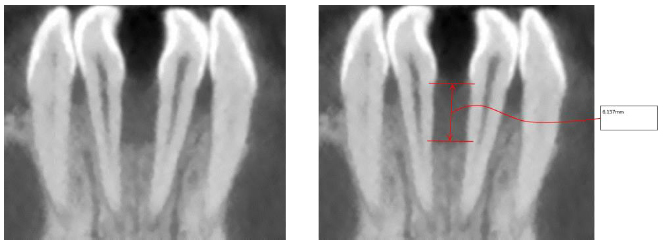
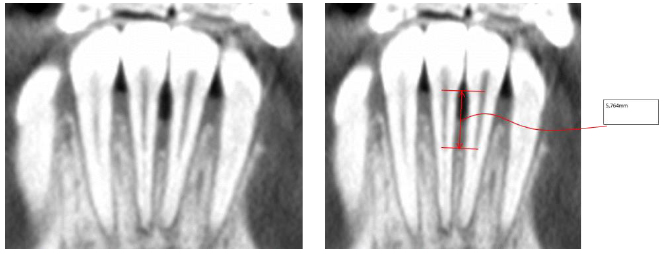
Post treatment records (Fig. 6) demonstrated anterior leveling and alignment, accompanied by the complete closure of the diastema and the radiographic healing of the vertical bone loss (Figs. 7 and 8) between mandibular central incisors with a regeneration of the inter radicular bone of about 0.4 mm. Then, the patient was instructed to wear a clear retainer in the lower arch at night. Fig. (9) shows the superimposition of the initial, final and planned positions; it was evident that most of the planned movements were achieved, but not all.
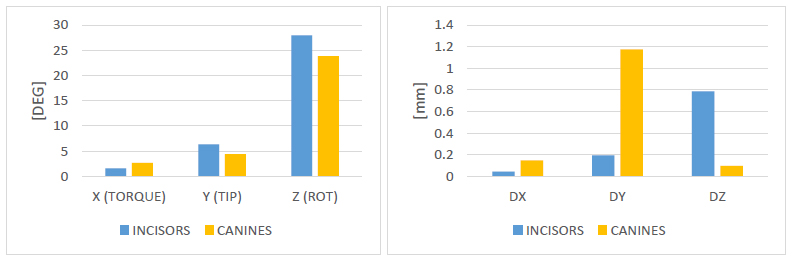
All the coronal and radicular planned movements of the incisors occurred in a more or less comparable way to the virtual setup (Fig. 10). The most effective were the mesial and lingual body movement of the incisors (98 and 97%) and the least effective was the bodily intrusion movement of the incisors (54%), and there were no unexpected movements in these teeth. The rotation of the incisors around its vertical axis showed a high degree of predictability (75%) and torque movements occurred in the incisors (76%). The tip movement occurred in 67% of patients compared to the virtual setup.
All the planned movements along with actual ones of the teeth, are reported in Tables 1-9.


| Tooth | ROT X [DEG] (TORQUE) | ROT Y [DEG] (TIP) | ROT Z [DEG] (ROT) | DX [mm] | DY [mm] | DZ [mm] |
|---|---|---|---|---|---|---|
| 44 | 0 | 0 | 0 | 0 | 0 | 0 |
| 43 | -0,31168 | -3,18523 | -31,1401 | 0,498573 | -0,49462 | 0,053101 |
| 42 | -0,27844 | -4,293 | -34,0652 | 0,119817 | -1,84107 | 0,121246 |
| 41 | 2,37 | -6,76 | -22,35 | -0,5308 | -1,23884 | 0,337608 |
| 31 | 0,21 | 5,85 | 24,46 | 0,877549 | -1,3721 | 0,348152 |
| 32 | -3,70251 | 2,397538 | 30,68933 | 0,316111 | -1,95082 | 0,894628 |
| 33 | -0,10785 | 8,159532 | 25,62461 | -1,24013 | -1,17045 | 0,247964 |
| 34 | 0 | 0 | 0 | 0 | 0 | 0 |
Table 2.
| Tooth | ROT X [DEG] (TORQUE) | ROT Y [DEG] (TIP) | ROT Z [DEG] (ROT) | DX [mm] | DY [mm] | DZ [mm] |
|---|---|---|---|---|---|---|
| 44 | -1,08158 | -4,53169 | -3,12598 | 0,720075 | -0,40534 | -0,48562 |
| 43 | -2,47806 | -2,6645 | -22,6286 | 0,567951 | -1,18671 | -0,21779 |
| 42 | -0,68594 | -1,79283 | -24,0376 | -0,08201 | -1,64447 | -0,40133 |
| 41 | 0,635898 | -4,14016 | -21,3214 | -0,92533 | -1,35285 | -0,26981 |
| 31 | -2,85 | 4,89 | 17,53 | 0,87562 | -1,40331 | -0,09989 |
| 32 | -3,96137 | 2,138656 | 20,71825 | -0,00572 | -1,80836 | 0,144147 |
| 33 | -4,00809 | 4,243633 | 10,32739 | -1,02221 | -1,65219 | -0,18043 |
| 34 | -1,04544 | 3,264033 | 4,151384 | -0,70181 | -0,70436 | -0,58294 |
No movement was expected in the first premolars. Instead, coronal and radicular movements were revealed by analyzing the data.
| Tooth | ROT X [DEG] (TORQUE) | ROT Y [DEG] (TIP) | ROT Z [DEG] (ROT) | DX [mm] | DY [mm] | DZ [mm] |
|---|---|---|---|---|---|---|
| 44 | 1,081575 | 4,531687 | 3,125979 | 0,720075 | 0,40534 | 0,48562 |
| 43 | 2,16638 | 0,520734 | 8,51151 | 0,069378 | 0,69209 | 0,27089 |
| 42 | 0,4075 | 2,500174 | 10,02768 | 0,20183 | 0,196597 | 0,522576 |
| 41 | 1,734102 | 2,619839 | 1,028629 | 0,394524 | 0,114008 | 0,607414 |
| 31 | 3,06 | 0,96 | 6,93 | 0,001929 | 0,031207 | 0,448046 |
| 32 | 0,258855 | 0,258882 | 9,97108 | 0,32183 | 0,142461 | 0,750481 |
| 33 | 3,900242 | 3,915899 | 15,29722 | 0,217925 | 0,481741 | 0,428393 |
| 34 | 1,045443 | 3,264033 | 4,151384 | 0,701807 | 0,704357 | 0,582941 |
The movements planned on the canines were achieved only in the coronal part but not in the root part Table (10).
| Tooth | DX | DY | DZ |
|---|---|---|---|
| 44 | 0 | 0 | 0 |
| 43 | 1,2904 | 0,1133 | 0,0051 |
| 42 | 1,7564 | 1,0866 | 0,0754 |
| 41 | 0,8405 | 0,4999 | 0,3566 |
| 31 | 0,6806 | 1,337 | 0,3853 |
| 32 | 1,5083 | 2,2563 | 0,6507 |
| 33 | 3,2252 | 0,2054 | 0,0515 |
| 34 | 0 | 0 | 0 |
| Tooth | DX | DY | DZ |
|---|---|---|---|
| 44 | 1,6334 | 0,5864 | 0,5013 |
| 43 | 1,6801 | 1,1461 | 0,318 |
| 42 | 0,8828 | 1,5412 | 0,4216 |
| 41 | 0,2204 | 1,456 | 0,2418 |
| 31 | 0,5149 | 1,8197 | 0,1396 |
| 32 | 1,281 | 2,2681 | 0,0111 |
| 33 | 2,3172 | 2,1153 | 0,4314 |
| 34 | 1,3211 | 0,7995 | 0,646 |
| Tooth | DX | DY | DZ |
|---|---|---|---|
| 44 | 1,6334 | 0,5864 | 0,5013 |
| 43 | 0,3897 | 1,0328 | 0,3129 |
| 42 | 0,8736 | 0,4546 | 0,3462 |
| 41 | 0,6201 | 0,9561 | 0,1148 |
| 31 | 0,1657 | 0,4827 | 0,2457 |
| 32 | 0,2273 | 0,0118 | 0,6396 |
| 33 | 0,908 | 1,9099 | 0,3799 |
| 34 | 1,3211 | 0,7995 | 0,646 |
| Tooth | DX1 | DY1 | DZ1 | DX2 | DY2 | DZ2 |
|---|---|---|---|---|---|---|
| 44 | 0 | 0 | 0 | - | - | - |
| 43 | 0,0325 | 0,7281 | 0,0686 | - | - | - |
| 42 | 0,0413 | 0,5066 | 0,0476 | 0,7242 | 3,0573 | 0,2909 |
| 41 | 1,0281 | 1,3891 | 0,2981 | 0,7195 | 2,8509 | 0,7527 |
| 31 | 1,1751 | 1,1603 | 0,2809 | 0,8374 | 2,8435 | 0,6946 |
| 32 | 0,1592 | 0,3585 | 0,7061 | 0,4184 | 2,7335 | 0,9085 |
| 33 | 0,2522 | 1,4706 | 0,276 | - | - | - |
| 34 | 0 | 0 | 0 | - | - | - |
| Tooth | DX1 | DY1 | DZ1 | DX2 | DY2 | DZ2 |
|---|---|---|---|---|---|---|
| 44 | 0,1154 | 0,2034 | 0,525 | - | - | - |
| 43 | 0,1951 | 0,7943 | 0,2403 | - | - | - |
| 42 | 0,0136 | 0,586 | 0,4867 | 0,3381 | 2,4308 | 0,3441 |
| 41 | 1,201 | 1,0374 | 0,3341 | 0,9376 | 2,456 | 0,0517 |
| 31 | 1,3786 | 0,7723 | 0,2315 | 1,2128 | 1,9903 | 0,1188 |
| 32 | 0,0467 | 0,3722 | 0,0439 | 0,1971 | 2,0018 | 0,1379 |
| 33 | 0,2893 | 0,8478 | 0,2832 | - | - | - |
| 34 | 0,1413 | 0,4737 | 0,6416 | - | - | - |
| Tooth | DX1 | DY1 | DZ1 | DX2 | DY2 | DZ2 |
|---|---|---|---|---|---|---|
| 44 | 0,1154 | 0,2034 | 0,525 | - | - | - |
| 43 | 0,1626 | 0,0662 | 0,1717 | - | - | - |
| 42 | 0,0277 | 0,0794 | 0,4391 | 0,3861 | 0,6265 | 0,0532 |
| 41 | 0,1729 | 0,3517 | 0,036 | 0,2181 | 0,3949 | 0,701 |
| 31 | 0,2035 | 0,388 | 0,0494 | 0,3754 | 0,8532 | 0,5758 |
| 32 | 0,1125 | 0,0137 | 0,6622 | 0,2213 | 0,7317 | 0,7706 |
| 33 | 0,0371 | 0,6228 | 0,0072 | - | - | - |
| 34 | 0,1413 | 0,4737 | 0,6416 | - | - | - |
| Teeth's group | X (TORQUE) | Y (TIP) | Z (ROT) | DX | DY | DZ |
|---|---|---|---|---|---|---|
| INCISORS | 76% | 67% | 75% | 98% | 97% | 54% |
| CANINES | 30% | 61% | 58% | 91% | 30% | 68% |
4. DISCUSSION
This treatment aimed to control crown and root movements as much as possible in the lower incisors in a patient with periodontal diseases in order to avoid a worsening of the situation.
Clear aligners are not able to give the teeth 100% of the movements planned in the digital setup [12, 13]. Simon et al. [14] proved that upper incisor torque could be performed using aligners with the mean accuracy of 42%. This study shows that in this patient the aligners were able to give a torque movement to the lower incisors with an average predictability of 76%, higher than the values reported in the literature. This could also be explained by the assumption that the torque movement of lower incisors with aligners is more predictable than other teeth because of their reduced root surface area [15].
The greatest discrepancies between the virtual setup and the patient’s situation at the end of the treatment were found in canine and incisor rotations. This is consistent with the results of previous systematic reviews indicating that rotation movements of the lower canines are the most difficult to achieve with aligners [12, 16].
The anchorage of the posterior teeth due to the posterior bite-block effect from the aligners’ constant occlusal coverage [17] could enhance the active intrusion of the incisors, and not allow the extrusive vectors of force on the anchorage teeth with the attachments.
5. CONCLUSION
This case showed that the reaction forces that pull to the anchorage teeth could move them: the premolars had an unexpected movement. Furthermore, it is necessary to consider that the effectiveness of clear aligners depends on the patient’s compliance. Thus, case selection is an important issue and teamwork and an open line of communication between the general dentist, the orthodontist and technicians are essential in determining the patient’s needs and achieving treatment goals [18].
6. LIMITATTIONS
The limitation of this study is that it is only a case report that can be considered as a pilot study to show the characteristics of the virtual root setup software. A controlled clinical trial would be necessary to validate the software. A study with a large sample of patients could add validity to the clinical experience presented in this paper and enable a more accurate assessment of the efficacy of this method of quantifying the amount of root movement that can be achieved with clear aligners.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written and informed consent was obtained from the patient.
STANDARDS OF REPORTING
CARE guidelines were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from corresponding author [S.M.] upon reasonable and justified request.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
None.
ACKNOWLEDGEMENTS
Declared none.


