All published articles of this journal are available on ScienceDirect.
Usefulness of Hard Palate Measurements in Predicting Airway Dimensions in Patients Referred for Cone Beam CT
Abstract
Purpose:
The aim of the study was to evaluate the usefulness of hard palate measurements in predicting airway dimensions in patients referred for cone-beam CT (CBCT).
Materials and Methods:
Six hundred forty-three patients (239 males and 404 females) were examined by CBCT. Using dedicated CBCT software (Kodak CS 3D imaging version 3.8.6, Carestream, Rochester, NY, USA); different hard palate (palatal interalveolar length, palatal arch depth, maxillo-palatal arch angle, and alveolar width) and airway measurements (airway volume, minimum cross-sectional area, minimum anteroposterior distance, minimum right to left distance and airway length) were obtained and correlated using Pearson’s correlation coefficients and regression analysis.
Results:
Although the correlation between hard palate and airway measurements was weak (Pearson coefficient (r) < 0.40), there were significant (P < 0.05) additive effects for hard palate measurements in predicting airway dimensions. Maxillo-palatal arch angle was the only hard palate measurement that had no effect in predicting airway dimensions.
Conclusion:
Hard palate measurements are considered useful in predicting airway dimensions in patients referred for CBCT.
1. INTRODUCTION
Several studies have explored the possible correlation between oro-pharyngeal measurements and craniofacial structures in different populations and in particular in subjects with sleep disorders [1-3]. For this purpose, various modalities were utilized, including cephalometric radiographic measurements and magnetic resonance imaging [4-6]. More recently, the use of three-dimensional (3D) craniofacial reconstruction imaging approaches has led to the widespread use of 3D imaging techniques for calculating and correlating volumes of facial bones and air cavities [7, 8] and for the assessment, diagnosis and treatment of sleep disorders, particularly Obstructive Sleep Apnea (OSA) [9, 10]. The early detection and treatment of OSA have been shown to be of paramount importance in reducing the risk of cardiovascular diseases and death as well as the frequency of strokes [11].
Although OSA has been addressed in the literature, a complete understanding of the pathophysiology and Upper Airway (UAW) anatomic specifications is yet to be reached. The coexistence of specific anatomic features and neuromuscular disorders appears to contribute to the narrowing and closure of the pharynx during sleep [12]. Many authors have shown that certain physical alterations (craniofacial, dental-bite, pharyngeal soft tissue, UAW size and shape) can be recognized in patients with OSA [13-15]. For instance, patients with OSA have narrowing in the oropharynx, usually at the level of the uvula–soft palate complex or the base of the tongue [16, 17]. Interestingly, several oral features were proposed to be useful in predicting those patients at risk of having UAW abnormalities. These features include; maxillary constriction and shallow palate, mandibular retrognathia, tooth crowding, retroclination of the anterior teeth and posterior cross-bite [18].
Therefore, dentists can play an important role in early diagnosis and referral of patients at risk of sleep disorders, as they come in close contact with the oral cavity in daily practice, and if well trained, they may be able to identify those who are at risk of OSA [19, 20]. More specifically, practitioners who use Cone Beam Computed Tomography (CBCT) technology are in a unique position to evaluate their patients for OSA [21-26]. In the paediatric population, pedodontists and orthodontists have the unique advantage of working with populations whose breathing disorders have not yet been diagnosed, and who are at a stage of development at which growth patterns are still easily modifiable for treatment of OSA [18].
Accordingly, this approach of engaging dentists in early detection and referral of patients at risk of breathing disorders could be enhanced if a relationship could be established between certain oral measurements on one hand, and the airway dimensions on the other hand. In this context, this study was designed to evaluate the usefulness of specific hard palate measurements in predicting airway dimensions in patients referred for CBCT.
2. MATERIALS AND METHODS
2.1. Patients
In our cross-sectional retrospective study, images for all patients aged over 40 years who underwent CBCT between January 2011 and January 2020 for dental implant treatment and other dental purposes at our dental radiology clinic were retrieved and evaluated. Only CBCT images showing the hard palate and oropharyngeal airway with correct patient positioning, normal jaw alignment, and free of pathologies and artefacts were included in the study. Cases with severe alveolar bone resorption or unilateral bone loss were excluded from the study. The patients included in the study were 643 patients. The present study is part of a protocol (20/2019) that was approved by our research review board.
2.2. Cone Beam Computed Tomography Examination
A KODAK 9500 Cone Beam 3D System (Carestream, Rochester, NY) CBCT apparatus with flat-panel detector was used. CBCT scanning parameters were: 0.2-mm as a voxel size, 90 kV as a tube voltage, 10 mA as a tube current and 10.8s as an exposure time. The patient was asked to stop swallowing and to keep teeth in maximum intercuspation. The occlusal plane was parallel with the floor and the field of view was 15x9 cm.
2.3. Images
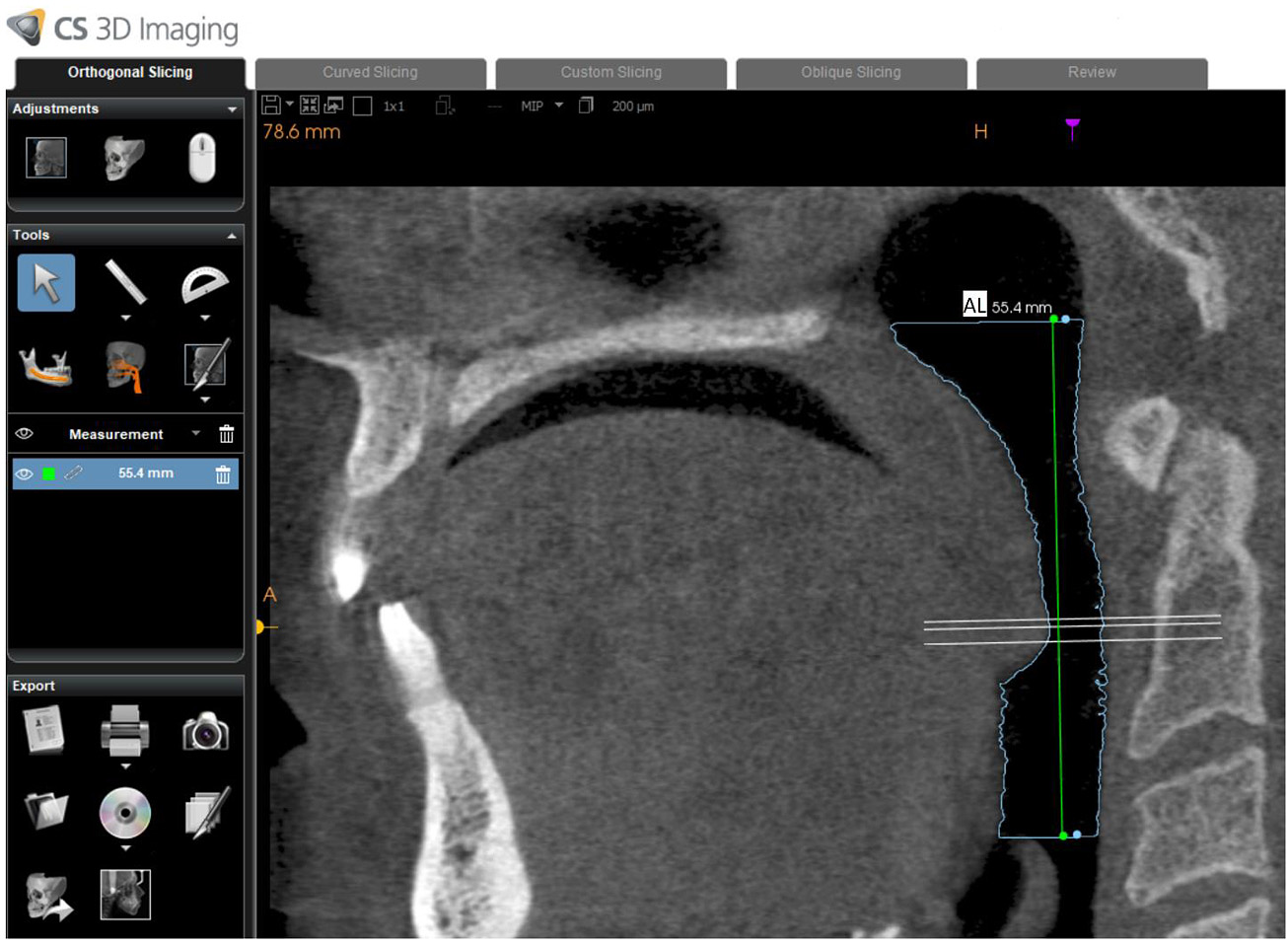
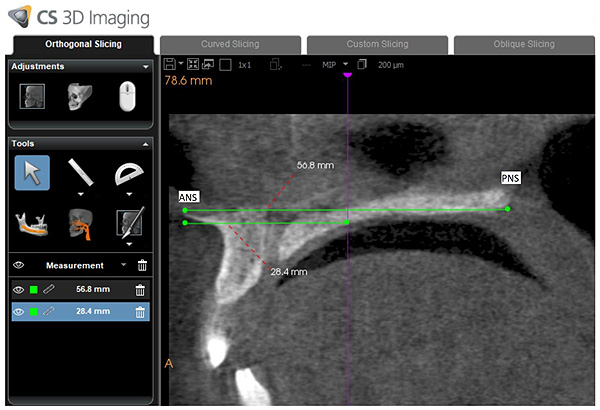
Using dedicated CBCT software (Kodak CS 3D imaging version 3.8.6, Carestream, Rochester, NY, USA), one calibrated oral radiologist (MA) with 12 years of experience with CBCT was responsible for drawing the path of the oropharyngeal airway from the posterior nasal spine to the superior border of the epiglottis on a midsagittal section (Fig. 1). The software subsequently and automatically generated the following values: airway volume (AV: cm3), minimum cross-sectional area (MCA: mm2), minimum anteroposterior distance (MAD: mm), and minimum right to left distance (MRD: mm). In addition to this, airway length (AL: mm) was manually measured by drawing a vertical line connecting the superior and inferior border of the oropharyngeal airway (Fig. 2).

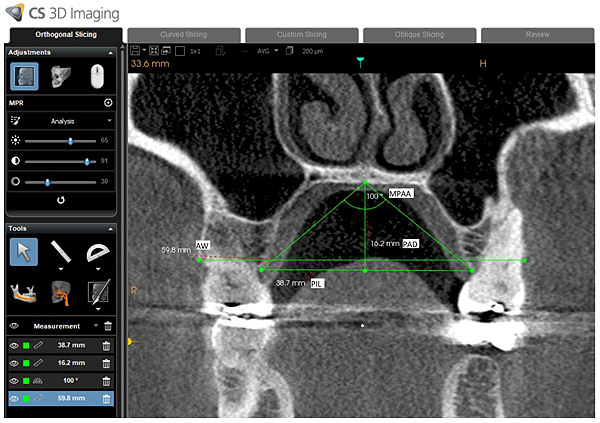
For hard palate measurements (Fig. 3), the following measurements were obtained following the examples of Akbay and Lim et al. [27, 28]:
(1) Palatal Interalveolar Length (PIL): Top-view length of the line from one side' alveolar crest to the same point of the other side’s alveolar arch.
(2) Palatal Arch Depth (PAD): The length of the line from the intersection of hard palates to the inter-alveolar line.
(3) Maxillopalatal Arch Angle (MPAA): The angle which is formed by the lines from the interpalatal’s mergence point to both crests of alveolar arches.
(4) Palatal arch depth/palatal inter-alveolar length (PAD/PIL): The ratio of hard palate depth to the inter-alveolar length.
(5) Alveolar Width (AW): The distance between right and left buccal alveolar bone
All of the hard palate measurements were obtained on a coronal section at mid-point of the hard palate length. The mid-point is the point located in the middle of the distance between anterior nasal supine and posterior nasal supine in the mid-sagittal plane (Fig. 4).
After 8 weeks, the same observer revaluated all of the airway and hard palate measurements. All images were evaluated on a high-definition liquid crystal display. The window settings were fixed for all cases.
2.4. Statistical Analysis
Data were described using means and were analysed using SAS 9.2 (SAS Institute, Cary, NC). Pearson’s correlation coefficient was used to determine the intra-rater correlation between first- and second-time measurements of the hard palate (PIL, PAD, PAD/PIL, MPAA, and AW) and airway (AV, MCA, MAD, MRD and AL) and the correlation between the hard palate and airway measurements. Independent samples t-test was used to compare the means of the variables between males and females. The interaction between different hard palate and airway measurements was tested using stepwise multivariate linear regression analysis. P < 0.05 was considered statistically significant.
3. RESULTS
This study included a total of 643 dental patients who were referred for CBCT (239 males and 404 females). Males had higher mean values for hard palate and airway measurements except for MPPA (Table 1). The differences in measurements were statistically significant except for MCA and MRD (t-test, P < 0.05).
The intra-rater correlations for hard palate and airway measurements were very strong (Pearson coefficient (r) ranged from .90-.98). Therefore, the two readings for each measurement were averaged to be used for further analysis. The correlation between average hard palate and average airway measurements was weak (Table 2).
| Parameter | Female | Male | P-value* | ||
|---|---|---|---|---|---|
| Mean (Range) | Standard Deviation | Mean (Range) | Standard Deviation | ||
| Age (years) | 55 (40-83) | 9.7 | 57.1 (40-96) | 10.2 | .009 |
| AW (mm) | 53.7 (36.9-65.3) | 4.6 | 55.4 (42.6-70.3) | 4.8 | <.0001 |
| PIL (mm) | 37.1 (28.6-45.7) | 3.3 | 38 (29-48.6) | 3.8 | 0.0024 |
| PAD (mm) | 13.2 (7.5-19) | 2.3 | 14.3 (8.1-22.3) | 2.5 | <.0001 |
| MPAA (degree) | 109.6 (80-135) | 10.5 | 106.3 (75-136) | 11 | 0.0002 |
| PAD/PIL (ratio) | 0.4 (0.2-0.6) | 0.1 | 0.4 (0.2-0.7) | 0.1 | 0.0002 |
| AV (cm3) | 10.4 (2.7-31.2) | 4.4 | 13.7 (4.4-39.6) | 5.3 | <.0001 |
| MCA (mm2) | 126.7 (17.6-444.5) | 80.8 | 132.9 (20.6-487.9) | 78.1 | 0.3401 |
| MAD (mm) | 8.5 (3.2-20.8) | 3.1 | 9.2 (4-18.4) | 3 | 0.0042 |
| MRD (mm) | 20.9 (7.8-37.4) | 6 | 21.4 (6.6-39) | 6 | 0.2726 |
| AL (mm) | 47.8 (33.2-64.3) | 5.8 | 57.8 (39-80.1) | 6.4 | <.0001 |
| Variable | AV | MCA | MAD | MRD | AL | |
|---|---|---|---|---|---|---|
| AW | Pearson r | 0.06 | -0.02 | 0.06 | -0.1 | 0.12 |
| P-value | 0.13 | 0.58 | 0.11 | 0.2 | 0 | |
| PIL | Pearson r | 0.1 | 0.04 | 0.12 | 0 | 0.08 |
| P-value | 0.01 | 0.29 | 0 | 0.6 | 0.05 | |
| PAD | Pearson r | 0.22 | 0.07 | 0.12 | 0.1 | 0.26 |
| P-value | <0.0001 | 0.07 | 0 | 0 | <0.0001 | |
| MPAA | Pearson r | -0.16 | -0.05 | -0.06 | -0.1 | -0.2 |
| P-value | <0.0001 | 0.21 | 0.14 | 0.1 | <0.0001 | |
| PAD/PIL | Pearson r | 0.16 | 0.06 | 0.06 | 0.1 | 0.2 |
| P-value | <0.0001 | 0.16 | 0.14 | 0 | <0.0001 |
| Parameter | Parameter Estimate | Standard Error | P-value |
Overall Model P-value |
|---|---|---|---|---|
| AV | ||||
| Intercept | 8.92 | 1.8 | <.0001 | <0.0001 |
| PAD | 0.33 | 0.08 | <.0001 | |
| Age | 0.049 | 0.02 | 0.008 | |
| Gender | -2.83 | 0.39 | <.0001 | |
| MCA | ||||
| Intercept | 131.64 | 25.66 | <.0001 | 0.0369 |
| PAD | 2.19 | 1.28 | 0.09 | |
| Age | -0.58 | 0.32 | 0.07 | |
| MAD | ||||
| Intercept | -7.20 | 6.12 | 0.24 | <0.0001 |
| PIL | 0.41 | 0.16 | 0.01 | |
| PAD | -0.73 | 0.42 | 0.08 | |
| PAD/PIL | 31.30 | 15.58 | 0.045 | |
| Gender | -0.48 | 0.26 | 0.06 | |
| MRD | ||||
| Intercept | 23.58 | 2.74 | <0.0001 | 0.0051 |
| AW | -0.12 | 0.05 | 0.02 | |
| PAD | 0.30 | 0.10 | 0.003 | |
| AL | ||||
| Intercept | 50.55 | 2.16 | <0.0001 | <0.0001 |
| PAD/PIL | 15.78 | 3.14 | <0.0001 | |
| Age | 0.18 | 0.02 | <0.0001 | |
| Gender | -9.23 | 0.47 | <0.0001 |
In order to evaluate the predictability of airway dimensions using hard palate measurements and demographics, we performed stepwise multivariate linear regression analysis (Table 3). There were significant additive effects for the PAD in predicting airway dimensions except for AL. While, a significant additive effect was shown for the: PIL in predicting MAD, AW in predicting MRD and the ratio of PAD/PIL in predicting MAD and AL. MPAA was the only hard palate measurement that had no effect in predicting airway dimensions.
4. DISCUSSION
OSA affecting different populations has been shown to be associated with age [29] and different anatomical abnormalities like hard palate depth and width [18-21, 26, 30]. Therefore, studying the anatomical characteristics of the hard palate by dentists in their clinic or by oral radiologists using CBCT images, will help in the identification of patients at risk of developing OSA.
In those previous studies [19, 20, 26, 30], the increase in PAD or the presence of deep palate was a common observation in OSA patients and increased the risk of developing OSA. Moreover, the increase in PAD was associated with posterior septal deviation [27]; this was also a significant finding in patients with OSA [30]. On the other hand, the presence of a narrow palate which can lead to low tongue position and narrowing of retroglossal airway space [26], is also a common and significant finding in patients with OSA [18-21, 26]. To overcome these abnormalities in hard palate dimensions, lowering and widening the palate by rapid maxillary expansion was shown to be successful in expanding the airway of adults with OSA [31].
Regarding CBCT airway measurements, most of them were formulated and investigated in relation to OSA by Tikku, Buchanan, Ogawa and Momany et al. [22-25]. In OSA patients, smaller measurements were obtained except for AL and MAD [23, 25]. To the best of our knowledge, there is no published research showing the usefulness of hard palate measurements in predicting airway dimensions. In contrast to airway measurements, palatal measurements can be easily obtained by using free CBCT software and even from a scan showing only the maxilla.
According to Ruangsri et al. [20], palatal depth and width can be classified into following: shallow palatal depth (<15 mm), normal depth (15–20 mm), deep palatal depth (>20 mm), narrow palatal width (<30 mm), normal width (30-42 mm), and large palatal width (>42 mm). However, we were unable to divide our patients following the same classification, since we used different methodologies for different populations.
The results of the current study imply that the dentist can early predict dimensions of the airway of the dental patients by calculating simple measurements of the hard palate in the clinic. This can be done directly inside the patient mouth or on CBCT images. Having only a CBCT image for the maxilla will be enough for getting the measurements. Patients with narrow dimensions of the airway can be referred to a sleep medicine specialist, this will help in identifying and treating patients with sleep apnea at an early stage.
Although this pilot study was conducted with a specific protocol on a specific ethnic group, its validity can be tested in future studies by correlating the CBCT measurements with the gold standard used to diagnose sleep disorders (polysomnogram study).
CONCLUSION
In conclusion, hard palate measurements are considered useful in predicting airway dimensions in patients referred for CBCT.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The present study is part of a protocol (20/2019) which was approved by Research Review Board of Jordan University, Jordan.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all patients before CBCT examination.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from the corresponding author [M. K.] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


