All published articles of this journal are available on ScienceDirect.
Local Dental Emergencies and Mitigation Strategies Adopted by Private Dental Practitioners of South India during COVID-19 Shelter in Place Warning - Multi-Centric Online Survey
Abstract
Objective:
To evaluate the common dental emergencies reported to dental practitioners and to compare the mitigation strategies implemented during the Shelter-In-Place (SIP) warning with dental practitioners’ age and sex.
Methods:
We conducted a cross-sectional online survey among the dental practitioners of south India during the period of COVID-19 SIP warning. An initial pool of items was prepared to capture the mitigation strategies in managing local dental emergencies. A structured questionnaire was then prepared in English based on the inputs of four expert dentist panel. Age and sex of the practitioners were also recorded.
Results:
The mean age of the dental practitioners was 37.11(range: 23 - 63) years.Of 159 dental practitioners that responded to survey, 90 were male. Most dental practitioners responded that they were contacted through a phone call (n=140) and WhatsApp messaging (n=108). The common dental emergencies reported were tooth pain (100%), swelling (91.7%), a decayed tooth (81.3%), and gum pain (78.6%). A higher number of male than female dental practitioners had “scheduled the treatment immediately” (OR=3.45; P=0.002) after adjusting for age.
Conclusion:
The most common dental emergencies during COVID-19 SIP were tooth pain, swelling, decayed teeth, and gum pain. Males and older dental practitioners scheduled appointments immediately.
1. INTRODUCTION
Oral or dental emergencies often relate to pain, bleeding, or trauma, which require immediate attention by the dental practitioner [1]. These may not be effectively managed by the general practitioner, as they are different and unique as compared to medical emergencies. Dental emergencies are common, and studies have reported that 1/5th of the general population has experienced orofacial pain in the last six months [2, 3]. Recent systematic review concluded that 3 out of 10 children or adolescents would have experienced pain [2]. The reasons for dental emergencies are tooth and gum pain due to caries, periodontitis, bleeding, erupting tooth, pericoronitis, trauma, etc [4], [5]. Bae et al. reported that dental trauma, dental infection, oral bleeding, and temporomandibular joint disorders were the common conditions reported in the emergency room [6]. The management of these conditions may vary from simple household remedies, local or systemic medications to complex dental procedures.
Literature reported a decline in the utilization of services during the COVID-19 pandemic for both dental emergencies (38% less) and non-emergencies (30% less), while there was an increase in oral infection of 20% [6]. Blackhall and Singh reported that 73% of the dental emergencies were infection related and 20% were trauma related [7]. Yu et al. reported that irreversible pulpitis was the most common dental emergency in a COVID-19 high-risk area that needs to be managed by endodontic therapy [8]. Langella et al. reported that the common dental emergency reported was severe dental pain (28%) [9]. Kranz et al. also reported that almost half (46.7%) of the respondents delayed dental visit due to the Pandemic and 12.4% delayed dental treatment even when it was bothering [10]. Hartnett et al. reported 42% decline in emergency dental visits when compared to the previous year [11]. Cagetti et al. reported a decline in all types of dental emergencies during lockdown when compared to pre-COVID period and increase in dental emergencies after reopening. They reported that endodontic emergencies were only 1/3rd during lockdown when compared to the pre-COVID period [12]. Similar findings were reported by Eggman et al. [13]
Literature exists on the preparedness or knowledge of dental practitioners concerning the management of dental emergencies [14-18]. However, the literature is scant regarding common dental emergencies and various mitigation management strategies used during the services’ unavailability (COVID-19 shelter-in-place warning).
There was a disruption in the availability of dental services across the country during the COVID-19 Shelter-In-Place (SIP) warning. Various agencies and associations have developed guidelines with continuous amendments to manage dental emergencies [19-22].
Understanding the morbidity of these conditions and management strategies would help to develop practical patient management guidelines and capacity building for disaster preparedness. Hence, we aimed to evaluate the common dental emergencies reported to dental practitioners and mitigation strategies implemented by dental practitioners during the SIP warning. We also assessed the association of the demographics of the dental practitioners with the mitigation strategies.
2. MATERIALS AND METHODS
We conducted a cross-sectional web-based survey among south India’s dental practitioners during the COVID-19 SIP warning (July to October 2020).The institutional ethics committee of Kasturba Hospital and Kasturba Medical College, Manipal (IEC 364/2020) approved the protocol.We sought informed consent from all the participating dentists.
An initial pool of items to capture dental practitioners’ mitigation strategies in managing local dental emergencies during COVID-19 SIP was prepared, given regional context and real-life scenario. They consisted of four dentists (periodontist, endodontist, maxillofacial surgeon, and public health dentist). A structured questionnaire was prepared in English based on a panel of expert dentists’ inputsover two rounds. We designed the questionnaire using Google forms and circulated it through the WhatsApp practice-based network groups. Based on the response distribution of 90%, with a 5% margin of error, 138 subjects were required. Sample size was inflated to 175, considering a non-response of 20%. A pilot study on a group of 20 dentists was done to assess the feasibility. The expert panel suggested minor modifications based on the results of the pilot study.
Independent dental practitioners contacted by patients or those who provided services during COVID-19 SIP warning and those willing to participate were included. We have excluded dental practitioners associated with group practice, corporate dental clinics, only academic, research institutions as their views, and strategies reflect the guidelines laid by their employers.
A questionnaire consisted of information on age, gender, “have you been contacted by your patients/friends for the management of local dental emergencies during COVID SIP warning? (yes/no),” mode of patient contact (Call/SMS /WhatsApp /Website/Clinic/teleconsultation apps), “frequency of patient contact” (almost every day/once in 2-3 days/ once in a week/ rarely), “type of dental emergencies” (tooth pain/gum pain/ abscess/broken filling/trauma to teeth/bleeding/ swelling/ others), “type of treatment related dental emergencies” (pain or swelling after filling/endodontic treatment/periodontal surgery /implants/orthodontic appliances/teeth removal/delay in ongoing treatment), mitigation strategies used (scheduled appointment/video call/phone call/photo or video of the oral cavity), recommended procedures (prescribed medications/local remedies/scheduled treatment due to lack of response with medicines/immediate treatment/referral of the patient), how much percentage of patients could be managed “without the need for rescheduling”, “self-reported satisfaction of patient management during lock down (0-10),”“most common patient’s reaction for the non-availability of dental services,” and any requirement or assistance for capacity building in the field of “infection control and waste management”, “Development of apps to effectively communicate,” “Technological advancement in the dental treatments,” “Infrastructure requirements for dental clinics,” and “Economic reforms to reduce the cost of treatment.”
2.1. Statistical Analysis
Data were analyzed by using SPSS version 18(PASW Statistics for Windows, Version 18.0. Chicago, SPSS Inc.). A p-value of <0.05 was considered statistically significant. Chi-square test compared the categorical variables. Logistic regression analysis was done for significant variables in bivariate analysis. Hosmer – Lemeshow test evaluated the goodness of fit for the logistic regression model.
3. RESULTS
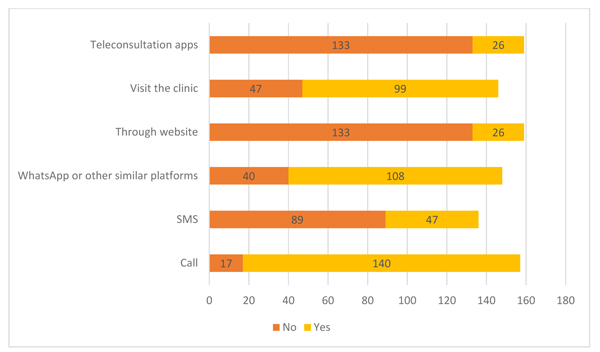
One hundred fifty-nine practitioners responded, out of which 90 were male.The participants’age ranged from 23 to 63 years,with a mean age of 37.11 years (SD=7.2; Median = 35). Patients contacted most dental practitioners through a phone call (n=140) and WhatsApp messaging (n=108). Very few dentists used teleconsultation Apps (n=26) (Fig. 1).
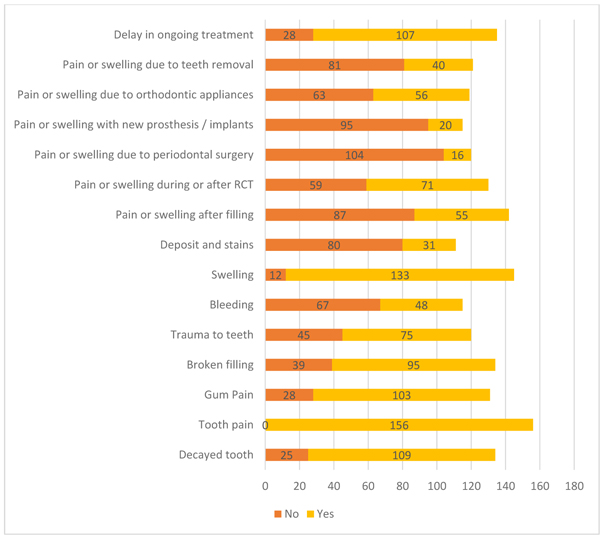
The frequent dental emergencies reported to the dental office during SIP were tooth pain (100%), swelling (91.7%), a decayed tooth (81.3%), and gum pain (78.6%). The most common treatment-related dental emergencies were “Pain or swelling during or after RCT (54.6%), Pain or swelling due to orthodontic appliances (47.1%), pain or swelling after filling (38.7%), and Pain or swelling due to teeth removal (33.1%). The majority of the patients reported that they were concerned about the delay in ongoing treatment (79.3%) (Fig. 2).
We compared the mitigation strategies with the dental practitioner’s age and sex. No significant differences between male and female dental practitioners for different mitigation strategies like “appointment to the clinic (P=0.067)”, “video call (P=0.494)”, “phone call (P=0.578)”, “requested a photo or video of the oral cavity (P=0.464),” “prescribed medications (P>0.99)”, “prescribed local remedies (P=0.159)”, and “scheduled the treatment due to lack of response/relief by either drugs or local remedies (P=0.31)” during SIP warning. However, a significantly higher number of male dental practitioners have scheduled the treatment immediately (P<0.001). A considerably higher number of female dental practitioners have referred the patients elsewhere (P=0.034) (Table 1).
Mitigation strategies were compared between young (≤35 years) and old dental practitioners (>35 years). It was seen that there were no significant differences between young and old dental practitioners for different mitigation strategies like “video call (P=0.372)”, “phone call (P=0.049)”, “requested a photo or video of the oral cavity (P=0.068),” “prescribed medications (P=0.319)”, “prescribed local remedies (P=0.15)”, “scheduled the treatment due to lack of a response/relief by either drugs or local remedies (P=0.359)” and “referral of patients (P=0.061)” during SIP warning. However, a significantly higher number of older dental practitioners have “scheduled appointments at clinics (P=0.031)” and “scheduled the treatment immediately” (P=0.008) (Table 1).
We used a binary logistic regression model to evaluate the role of age and gender on mitigation strategies. Factors that were significant in the bivariate analysis were included in the model. There was no significant association seen with “scheduling appointment to the clinic” with age (OR=0.506; P=0.113) and gender (OR=1.57; P=0.279) of the dental practitioners. A higher number of male than female dental practitioners had “scheduled the treatment immediately” (OR=3.45; P=0.002) after adjusting for age. There was no significant association was seen between the “referral of patients” with age (OR=1.54; P=0.241) and gender (OR=56; P=0.125) of the dental practitioners.
Overall, the mean percentage of patients that could be managed without scheduling the treatment was 41.5±22.06 (Median = 40). Most of the dental practitioners reported that the majority of their patients were “understanding”(66.7%). In contrast, 1/4th of the dental practitioners said their patients were disappointed (27.7%) or arguing (5.7) with managing dental emergencies during the SIP warning. For self-reported satisfaction in the management of dental emergencies, male (7.09±2.32; P<0.001) and older (6.73±2.26; P=0.044) dental practitioners were more satisfied than female (5.29±2.32) and younger (5.89±2.63) dental practitioners.
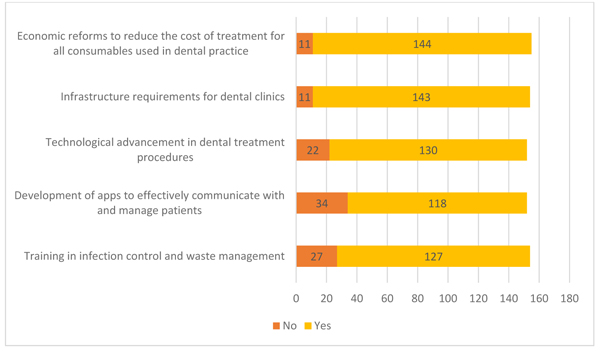
The most common perceived deficiencies reported by the dental practitioners were the need for “Economic reforms to reduce the cost of treatment for all consumables used in dental practice” (92.9%) and “infrastructure requirements for dental clinics” (92.9%) (Fig. 3).
| Mitigation Strategies | Male N(%) |
Female N(%) |
P-value | ≤35 Years N(%) |
>35 Years N(%) |
Total N(%) |
P-value |
|---|---|---|---|---|---|---|---|
| Scheduled appointment to the clinic † | - | - | - | - | - | - | - |
| No | 16(18.4) | 20(31.2) | 0.067 | 24(31.2) | 12(16.2) | 36(23.8) | 0.031 |
| Yes | 71(81.6) | 44(68.8) | 53(68.8) | 62(83.8) | 115(76.2) | ||
| Scheduled a video call † | - | - | - | - | - | - | - |
| No | 38(50.7) | 29(56.9) | 0.494 | 31(49.2) | 36(57.1) | 67(53.2) | 0.372 |
| Yes | 37(49.3) | 22(43.1) | 32(50.8) | 27(42.9) | 59(46.8) | ||
| Scheduled a phone call † | - | - | - | - | - | - | - |
| No | 14(17.3) | 8(13.8) | 0.578 | 7(9.9) | 15(22.1) | 22(15.8) | 0.049 |
| Yes | 67(82.7) | 50(86.2) | 64(90.1) | 53(77.9) | 117(84.2) | ||
| Requested a photo or video of the oral cavity † | - | - | - | - | - | - | - |
| No | 10(11.8) | 5(8.1) | 0.464 | 4(5.6) | 11(14.7) | 15(10.2) | 0.068 |
| Yes | 75(88.2) | 57(91.9) | 68(94.4) | 64(85.3) | 132(89.8) | ||
| Prescribed drugs (analgesics, antibiotics) † | - | - | - | - | - | - | - |
| No | 1(1.1) | 0(0) | >0.99 | 1(1.2) | 0(0) | 1(0.6) | 0.319 |
| Yes | 89(98.9) | 69(100) | 79(98.8) | 79(100) | 158(99.4) | ||
| Prescribed local remedies (local anaesthetic gel, salt water gargles or mouth rinses or desensitizing toothpaste) † | - | - | - | - | - | - | - |
| No | 11(12.8) | 4(6) | 0.159 | 5(6.4) | 10(13.3) | 15(9.8) | 0.15 |
| Yes | 75(87.2) | 63(94) | 73(93.6) | 65(86.7) | 138(90.2) | ||
| Scheduled the treatment due to lack of response/relief by either drugs or local remedies ‡ | - | - | - | - | - | - | - |
| No | 21(26.2) | 12(19) | 0.31 | 15(20) | 18(26.5) | 33(23.1) | 0.359 |
| Yes | 59(73.8) | 51(81) | 60(80) | 50(73.5) | 110(76.9) | ||
| Scheduled the treatment immediately ‡ | - | - | - | - | - | - | - |
| No | 35(43.2) | 44(75.9) | <0.001 | 47(68.1) | 32(45.7) | 79(56.8) | 0.008 |
| Yes | 46(56.8) | 14(24.1) | 22(31.9) | 38(54.3) | 60(43.2) | ||
| Referred the patient ‡ | - | - | - | - | - | - | - |
| No | 49(60.5) | 25(42.4) | 0.034 | 32(45.1) | 42(60.9) | 74(52.9) | 0.061 |
| Yes | 32(39.5) | 34(57.6) | 39(54.9) | 27(39.1) | 66(47.1) |
4. DISCUSSION
We conducted a cross-sectional web-based survey to evaluate the common dental emergencies reported to dental practitioners and mitigation strategies implemented by dental practitioners during the COVID-19 SIP warning. We also compared the relationship of age and sex of the dental practitioners with these mitigation strategies. Studies have been conducted on dentist preparedness or knowledge to manage dental or medical emergencies [14-17, 23] in the dental office, but not on the mitigation strategies in managing dental emergencies during the SIP warning or any disasters. Direct comparisons were not possible as similar studies were not reported to date. The concept of emergency dental services is practically non-existent in developing countries like India and limited to only a few centers that provide care for trauma. Other than trauma, dental emergencies would be managed with medications in most centers with appropriate referral to dental clinics. Most of the dental care in India is provided through private dental practitioners and is an out of the pocket expenditure to the patients. Insurance coverage is limited with high premiums with a range of only a few conditions that require hospitalization (trauma, severe oral infections, cysts, and tumors).
Dentists can assist in disaster response activities like people of the medical community. In the event of dental emergencies during disasters, the medical personnel’s management is limited to the prescription of medications that may not be sufficient. Dental conditions are effectively managed in dental clinics than in hospital-based emergency rooms [24]. Guo et al. reported that fewer patients had sought dental emergency services with an upward shift in dental infections among the patients during the pandemic [25].The common dental emergencies reported in our study were tooth pain, swelling, decayed teeth, and gum pain, which was similar to that reported in previous studies [4-6, 25-28].An upward trend in emergency dental visits to the emergency departments was reported from developed countries [29]. Most of these conditions require emergency management and may or may not resolve with medical management. The dental practitioners must have a plan to make their services available to the patients. During the disasters, the conventional or traditional contact mode may not be possible, and patients may contact dental practitioners through alternate modalities. Dental practitioners should arrange for effective communication with the patients. With the advances in information technology, many alternate methods like phone calls, messaging, websites, and telemedicine apps are now available to contact dental practitioners. In our study, dental practitioners reported that most patients reached through a phone call, WhatsApp,or similar services or visited the clinic. Very few dentists were providing services through teleconsultation apps.
The most common treatment-related dental emergencies were pain or swelling during or after RCT, orthodontic appliances, after filling,or due to teeth removal. All these conditions would require management by the dental practitioner and werenot evaluated in previous studies.
Our study’s dental practitioners were mitigating the patient problems through phone calls, prescription of medication, or photo or video from the patient.Most dental practitioners reported the prescription of medications similar to that reported by Bae et al. [6]. There were no differences in the distribution of these mitigation strategies with dental practitioners’ age and sex. A substantial amount of dental practitioners provided the services by scheduling the appointments to the clinic in line with earlier reports [30].
Most dental practitioners had also scheduled the patients to the clinic when there was no response or relief with medications. Males and older dental practitioners have scheduled appointments immediately than their counterparts. In addition, females and younger dentists were more likely to refer patients. This tendency could be due to the higher risk-taking behaviour of males, due to which they could be more inclined to treating dental emergencies during SIP warning. The older dentists who were more experienced could manage dental emergencies in the clinic. However, we could not rule out the role of many other factors (financial, family, and personal).
Overall, the mean percentage of patients managed without scheduling the treatment was 41.5±22.06, highlighting those dental emergencies would require complex treatments and may not resolve with medications. Dental practitioners should be ready with various strategies to provide optimal care in routine dental practice and future pandemics. Males and older dental practitioners were more satisfied than female and younger dental practitioners were. It could be due to the mitigation strategies adopted by them, which could have led to many dental emergencies leading to greater satisfaction in resolving pain and suffering among the patients during the SIP warning. However, this aspect needs further evaluation as studies on the factors (age and sex) related to dental practitioners' satisfaction were scant.
Overall, because of the COVID-19 pandemic, most dental practitioners have reported a need for economic reforms to reduce dental treatment costs, improvement in the infrastructure requirements for dental clinics, and the need for technological advancement.
Government agencies and regulatory bodies need to develop area-specific guidelines for training and capacity building so that there is no disruption of emergency dental care services. There is a need to develop policies with dental practitioners’ help to render safe and effective emergency dental care services.
CONCLUSION
Only four out of 10 dental emergencies were managed with only medications. The common dental emergencies were tooth pain, swelling, decayed teeth, and gum pain. Female and younger dentists were more likely to refer patients.
ABBREVIATION
| SIP | = Shelter In Place |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Institutional Ethics Committee of Kasturba Hospital and Kasturba Medical College, Manipal (IEC 364/2020) approved the protocol.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
We sought informed consent from all the participating dentists.
AVAILIBILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available from corresponding author [K.C] upon reasonable request
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest financial and otherwise.
ACKNOWLEDGEMENTS
We thank all the practitioners for their valuable time in responding to the questionnaire.


