All published articles of this journal are available on ScienceDirect.
Evidence-based Recommendations on Periodontal Practice and the Management of Periodontal Patients During and After the COVID-19 Era: Challenging Infectious Diseases Spread by Airborne Transmission
Abstract
Background:
Periodontal care, which was completely suspended during the peak of the SARS-Cov-2 pandemic and was delayed and recurrently discontinued during the succeeding waves, must be safely provided in the COVID-19 era.
Objectives:
The study aimed to provide recommendations on periodontal practice, optimizing safety, ergonomics, and economic resources, and the management of periodontal patients, ensuring continuity, timing, and effectiveness of periodontal care in the COVID-19 era.
Methods:
Reported protocols for the dental practice in the context of the COVID-19 and current evidence on periodontitis treatment and prevention were reviewed.
Results:
Evidence-based recommendations on contamination control and ergonomic improvements for periodontal practice and the management of periodontal patients challenging COVID-19 and airborne infectious diseases have been provided.
Conclusion:
Due to the economic, ergonomic, and ethical concerns raised by limited periodontal care due to the SARS-Cov-2 pandemic, and awareness of other emerging airborne transmitted infections, the periodontal practice should integrate measures minimizing airborne cross-infections and optimizing time-space and economic resources. The management of periodontal patients in the COVID-19 era should comprise less complex treatments and more comprehensive and definitive approaches, reducing emergencies, session length and number, and, concurrently, extending the recall and maintenance intervals. Moreover, it should implement prevention strategies through teledentistry tools and apps, improving periodontal awareness and self-care, and also through the self-reporting of periodontitis and periodontal risk assessment tools, performing both “population-based” and “high-risk” surveillance of periodontitis. Finally, it should enhance inter-professional collaboration, through telehealth networks, especially targeting subjects at high-risk of both periodontitis and systemic disorders, each of the two variously linked to COVID-19 onset and worsening.
1. INTRODUCTION
An outbreak of a novel coronavirus disease, which was first reported in China in December 2019 [1] and designated as COVID-19 on 11th February 2020, has rapidly spread across the globe and been declared as a pandemic disease by the World Health Organization on 11th March 2020 [2].
The latest strain of coronavirus, later named as severe acute respiratory syndrome coronavirus 2 or SARS-CoV-2 [1], has genomic similarities of 79% with SARS-CoV and 50% with MERS-CoV, respectively, also belonging to Corona-viridae family, but differs from them principally in its receptor-binding domain sections spike protein structures [1], which show higher effectiveness in binding to human cellular entry receptor ACE2, facilitating virus cell entry and inter-human transmission [3].
SARS-CoV-2 is mainly transmitted via direct contact with respiratory droplets, through cough, sneeze and droplet inhalation, or via indirect contact of oral, nasal, and eye mucous membranes with contaminated fomites or saliva [4] from infected, also asymptomatic, subjects [1, 5]. Moreover, fecal-oral transmission [6] of SARS-CoV-2 has also been described as well as airborne transmission [7, 8], which may be of particular interest for dental settings, that invariably carry the risk of SARS-CoV-2 transmission, especially considering the inter-personal proximity, the exposure to blood and saliva, the handling of sharp instruments, and the variety of aerosol-generating dental procedures [1, 5, 9].
Therefore, dental patients are inevitably exposed to a high risk of SARS-CoV-2 infection, as the virus can be transmitted both via direct contact of the oral and nasal mucosa (as well as conjunctival mucosa safety goggles) with droplets and aerosols containing the virus, generated from an infected individual and propelled at short distances and via indirect contact with contaminated dental instruments and/or dental setting surfaces [10].
Analogously, oral healthcare professionals are exposed to a higher risk of getting infected because of the close contact with patients not wearing face masks, aerosol and droplets from the patients’ oral cavity, the risk of direct contact with blood, oral fluids, or other patient materials.
Given these considerations, non-urgent periodontal care has been completely suspended in US [11, 12] and in many other countries during the peak of COVID-19/SARS-CoV-2 pandemic and delayed and recurrently discontinued during the succeeding viral waves, therefore, increasing the number of dental patients in need of definitive treatments. This may be especially true for periodontal patients, who are affected by a chronic disease, which represents a major global disease burden, with deleterious effects on oral health and oral health-related quality of life and with several interconnections with general health, and who do not require urgent care but a systematic and long-term periodontal treatment planning and scheduling.
Therefore, the purpose of the present study was, through cross-search databases (PubMed/MEDLINE and Science Direct), to identify reported protocols for dental practice appropriate to counteract airborne transmitted infections, especially those developed in the context of COVID-19, and to review current scientific evidence on periodontal treatment and periodontitis prevention, in order to provide recommendations on periodontal practice, optimizing safety, ergonomics and economic resources, and on the management of periodontal patients, ensuring the overall continuity, timing and effectiveness of periodontal care, during and after the COVID-19 era, challenging airborne infectious diseases.
2. PERIODONTAL PRACTICE, COVID-19 AND AIRBORNE TRANSMITTED INFECTIONS: CONTAMINATION CONTROL MEASURES AND ERGONOMIC IMPROVEMENTS OPTIMIZING SAFETY AND ECONOMIC RESOURCES
In the COVID-19 era, dental and periodontal procedures should be performed under the recommendations given to minimize the risks of SARS-Cov-2 transmission in dental settings [1, 5, 8-10, 13-17], and appropriate for periodontal care, as reported in Table 1. Those measures allow a safe provision of oral health care over airborne cross-infections, but may require additional efforts, also described in Table 1, in the overall ergonomics of dental and periodontal practice to avoid an increase in dental as well as periodontal treatment time and costs. Indeed, rescheduling of periodontal patients should be specifically performed according to priority, as advised for patients requiring oral and maxillofacial surgery procedures [13], and consistent with the time-space organization required by contamination control measures, implying, with the ever-increasing number of periodontal treatments discontinued during the peak and the further waves of the pandemic, delays in rescheduling of patients in active periodontal therapy, as expected for general dentistry and other dental specialties [1]. Concomitantly, recalls for patients in periodontal maintenance care may be even more procrastinated, further reducing the accessibility to periodontal care and potentially determining a lack of periodontitis progression control [18], a negative impact on the oral health-related quality of life [19] and an unintentional patient abandonment. In addition, rising costs of periodontal management may affect both private and public dental care services, making periodontal therapy economically unaffordable for more people. Since periodontitis constitutes an important public health problem, if left untreated may lead to serious morbidity and financial burdens [20], especially considering the high prevalence of the disease [21]. Therefore, teledentistry may play a relevant role in minimizing cross-infections and improving ergonomics, increasing access to dental care while reducing person-to-person contact and the daily number of patients and healthcare workers in the office, therefore,decreasing personal protective equipment use and decontamination procedures costs.
3. MANAGEMENT OF PERIODONTAL PATIENT DURING AND AFTER THE COVID-19 ERA: SAFETY, CONTINUITY, TIMING AND EFFECTIVENESS OF PERIODONTAL CARE
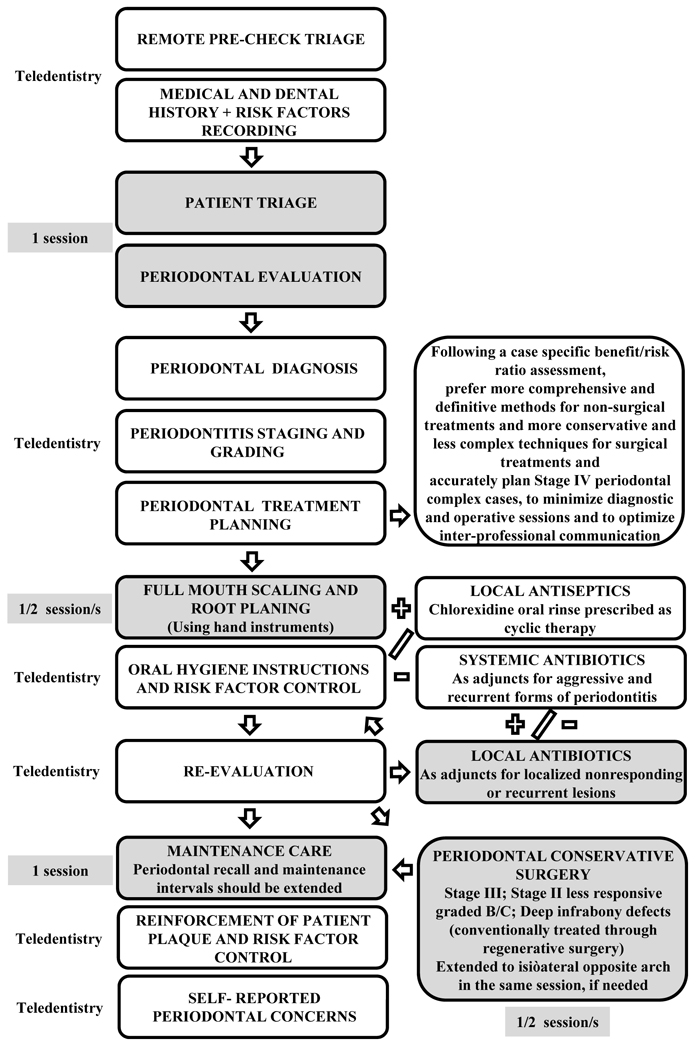
Along with the above-mentioned ergonomic and economic concerns, ethical issues may also be raised by limited dental and periodontal practice, such as the disattendance, in the context of COVID-19, and principles of Justice (fairness), Nonmaleficence (do no harm) and Beneficence (do good) [22], requiring a properly adapted management of periodontal patients, in order to ensure continuity, timing and effectiveness of periodontal care. In this perspective, oral health care professionals and periodontists, beyond integrating all recommendations on contamination control and ergonomic improvements (Table 1), should, as appropriate, adjust both periodontal treatment plans in active and maintenance phases of the therapy (Fig. 1), and improve interprofessional collaboration, also aided by teledentistry, as synthesized in Table 2.
Flowchart for active periodontal treatment and maintenance care proposed for the management of periodontal patients in the COVID-19 era is presented in Fig. (1).
3.1. Active Periodontal Treatment
A pre-operative mouth rinse with povidone-iodine, able to inactivate both SARS-Cov and MERS-CoV within 15 seconds in a 1:30 dilution [23], or with cyclodextrins combined with Citrox®, still under study [24], maybe recommended, to reduce SARS-Cov-2 aerosolization [23] and salivary load [24], respectively, since chlorhexidine seems to be not effective against SARS-CoV-2 [9, 24, 25], and the use of hydrogen peroxide, based on the vulnerability of Sars-Cov-2 to oxidation, is not supported by sufficient scientific evidence [25].
In line with the recommendation to avoid or reduce to a minimum the aerosol-generating procedures [5, 17], subgingival, as well as supragingival, mechanical plaque and calculus removal should be performed using hand rather than powered instruments, which are equally effective in reducing gingival bleeding [26, 27] and in improving self-performed oral hygiene maintenance [28], and require, in order to achieve and maintain a healthy periodontal status, to be combined with oral hygiene instruction, that may be provided through teledentistry instruments. In particular, subgingival nonsurgical periodontal treatment should be preferentially conducted, if possible, through the use of non-aerosol generating curettes, which determine lower sensitivity, leave a smoother root surface and are more effective, even if slower, in calculus removal when compared to sonic and ultrasonic scalers [28].
Since physical distancing is not feasible during dental and periodontal procedures, contact times should be shortened [21], sessions should be reduced in numbers, and periodontal recall and maintenance intervals should be otherwise extended. In this perspective, a decision-making algorithm in periodontitis management may lean toward more comprehensive and definitive techniques and methods, preferring full-mouth in place of quadrant approach and one- to multi-stage procedures. In addition, treatment planning may be inclined toward more conservative and less complex treatment strategies that enhance the effectiveness of the treatment and, concurrently, reduce the risk of postoperative complications and emergencies and the need for close-set controls. From this point of view, full-mouth disinfection, providing one/two-stage scaling and root planing of the entire dentition within 1-24 hours period, with optional chlorhexidine application, decreases the risk of re-infection of treated sites [28, 29] due to microorganisms from untreated, periodontal lesions, mucosal surfaces and saliva, and reduces the time needed for subgingival instrumentation [28], and, as a consequence, sessions number and length and may, therefore, meet the needs of the COVID-19 context better than the conventional multi-stage treatment approach [28-30]. Repeated reinforcements of patient biofilm control, required by more comprehensive and definitive approach, may benefit from teledentistry.
Plaque control should be enhanced through cyclic therapies with chlorhexidine mouthwashes, which gives better results than subgingival instrumentation alone or combined with professional supragingival debridement [28]. In addition, systemic antibiotics, which are not effective in periodontal management as a monotherapy, due to the high resistance of the biofilm to antimicrobials, and are not often administered to periodontal patients because of the risk for resistance and adverse reactions, may be considered, as previously proposed for juvenile periodontitis, and should be administered as adjuncts to non-surgical treatments for aggressive and recurrent forms of periodontitis, which are associated with specific microbiological profiles, upon, if possible, periodontal site microbiological evaluation [28]. Moreover, reinforcements of patient plaque control should be performed through teledentistry tools, as described hereinafter.
In addition, since a careful and conventionally timely-planned periodontal monitoring may be hardly practicable, in the context of the COVID-19 pandemic, deep intrabony defects, conventionally treated through regenerative surgery [38], may also be preferentially treated with conservative rather than regenerative surgery, as the latter requires rigidly scheduled and repeated controls. Indeed, although guided tissue regeneration, as well as treatment with enamel matrix derivatives and a combination of the two procedures, similarly produce significant attachment gain and pocket reduction [27], healing of regenerated periodontal sites is considered as a delicate process, potentially affected by a multitude of systemic and local factors [28], especially flap design [28], smoking [39] and plaque control [40], that may scarcely be controlled through teledentistry. In particular, a lack of adequate plaque control after periodontal regenerative procedures may negatively affect both postsurgical outcomes and the long-term stability of the results [28], advocating the need for oral hygiene motivation. Analogously, mucogingival therapy may currently not be indicated and/or limited, if not suspended, in the context of the COVID-19 pandemic.
Stage IV complex periodontal cases, requiring an interdisciplinary approach to control periodontitis and to rehabilitate lost masticatory function [31], should be carefully diagnosed [41], initially discussed by the different providers through implemented telework solutions optimizing inter-professional communication [42]. Treatment flows of such complex cases should be accurately planned [43], avoiding redundant procedures and minimizing diagnostic and operative sessions. Teledentistry sessions, indeed, may be crucial in active periodontal treatments, for patients’ scheduling according to priority, remote pre-check triage, medical and dental history with periodontal risk factors recording, for periodontitis diagnosis with staging, grading and treatment planning in a multi-disciplinary digital setting, and for communicating to the patients therapeutic options, measures for risk factors control and oral hygiene instructions.
Table 1.
| Aspects | Recommendations | Goal(s) |
| Infection control | • Not seeing in dental settings patients with active COVID-19 infection, according to the ADA and CDC guidance [1] • Considering all patients as asymptomatic SARS-CoV-2-positive patients [16], since SARS-Cov-2 transmission rate is similar between symptomatic and asymptomatic cases [15], thus performing patients pre-check triages, to measure body temperature and record current health status and history of contact with the virus [5], and using adequately personal protective equipment [1,5,9] • Postponing at least 1 month, as previously proposed for SARS [14], the treatment for convalescing patients • Avoiding if possible, or conducting cautiously [4,5], aerosol-generating procedures, such as those employing a 3-way syringe and low or high -speed drilling or ultrasonic devices with water spray [5,17], and procedures potentially stimulating saliva and coughing, such as intraoral x-ray examinations • Employing fitted N95 respirators and fullface shields [5,17] in addition to conventional PPE, using rubber dams [5], anti-retraction handpieces [9] and high-volume saliva ejectors [8,10], for necessary aerosol generating procedures • Meticulously performing cleaning and disinfection procedures for instruments, dental apparatuses, surfaces, environment and non disposable PPE [5] • Properly reorganizing medical waste management [9] |
Minimizing the risks of SARS-Cov-2 transmission in dental settings to allow the provision of safe periodontal care |
| Ergonomics | ▪ Avoiding the presence of accompanying persons and reducing to a minimum number of patients in the waiting room and the waiting time, to guarantee the social distancing [13] ▪ Properly reorganizing operating and non-operating rooms, equipment storage, to guarantee adequate ventilation and decontamination procedures and ergonomical organization [5] ▪ Properly reorganizing staff assignment to accommodate only the patient and the necessary staff members [5] ▪ Correctly timing cleaning and disinfection procedures ▪ Rescheduling patients appointments according to priority [13] ▪ Reducing contact time, through periodontal active and maintenance sessions shortened in duration and reduced in number and maintenance intervals otherwise extended ▪ Performing procedures that carry lower risks and possibly higher benefit to periodontal patients ▪ Preferring more comprehensive and definitive techniques and methods, and more conservative and less complex treatment strategies, to enhance the effectiveness of the treatment and concurrently reduce the risk of postoperative complications and the need for close-set controls ▪ Planning aerosol generating procedures at the end of the day, if possible ▪ Preferably treating suspected cases with COVID-19 in isolated room, negatively pressured, as the last patient of the day. |
Reconceptualization of time and space organization and of economic and human resources in periodontal practice |
Table 2.
| Aspects | Recommendations | Goal(s) |
| Periodontal treatment Active therapy | • Pre-operative mouth rinse (with povidone-iodine or cyclodextrins combined with Citrox® or Hydrogen peroxide [24,25]) • Performing supragingival and subgingival mechanical plaque and calculus removal using hand rather than powered instruments to avoid or reduce aerosol generating procedures • Performing full-mouth in place of quadrant approach and one- in place of multi-stage procedures, favouring more comprehensive and definitive techniques and methods • Enhancing biofilm control, through a chlorhexidine oral rinse, prescribed as cyclic therapy • Considering adjunctive therapy with systemic antibiotics for aggressive and recurrent forms of periodontitis, as previously proposed for juvenile periodontitis, and upon periodontal site microbiological evaluation, if possible • Performing more conservative and less complex periodontal surgical treatments, such as conservative surgery in place of open flap debridement and modified Widman flap, in periodontal subjects belonging to stage III, based on case complexity factors • Preferring flap designs that preserves as much as possible the tissue microvasculature • Local application of antibiotics for localized nonresponding and recurrent lesions • Performing conservative surgical treatment of the ipsilateral opposite dental arches, if needed, in the same session, enhancing the time-effectiveness of the treatment. |
Adjustment of decision making, treatment planning and practice to ensure continuity, timing and effectiveness of periodontal care |
| Periodontal treatment Active therapy | • Considering conservative periodontal surgery also for those stage II patients, who are less responsive to standard treatment or graded as B or C, based on the rate of periodontitis progression, and require a more intensive management • Considering conservative periodontal surgery also for deep intrabony defects, conventionally treated through regenerative surgery, requiring rigidly scheduled and repeated controls, favouring more conservative and less complex treatment strategies • Limiting or suspending mucogingival therapy, favouring less complex treatment strategies • Accurately planning diagnostic and treatment flows of Stage IV periodontal complex cases, requiring an interdisciplinary approach, in order to minimize both diagnostic and operative sessions and to optimize inter-professional communication through telehealth tools. • Performing oral hygiene instruction and periodic motivation reinforcement, through teledentistry instruments |
Adjustment of decision making, treatment planning and practice to ensure continuity, timing and effectiveness of periodontal care |
| Periodontal treatment Maintenance | • Reducing the number of periodontal maintenance visits, as much as possible, without reducing patients' adherence to maintenance care. • Shortening the periodontal maintenance session, along with promotion of smoking cessation, devolving oral hygiene instruction, reinforcement and motivation to teledentistry • Potentially planning optimal periodontal recall intervals, through newly developed individual risk assessment tool |
Adjustment of decision making, treatment planning and practice to ensure continuity, timing and effectiveness of periodontal care |
| Periodontitis prevention | • Increasing patients’ periodontal awareness and literacy, through teledentistry tools and a dedicated app • Improving periodontal self care through teledentistry tools and a dedicated app • Enhancing a “population-based” preventive approach, through the development and the promotion of validated self-reporting of periodontal disease • Enhancing a “high-risk” preventive approach, through the development and the promotion of individual risk assessment tools [45] |
Adjustment of the prevention strategies for periodontitis onset and progression, to counteract the potential reduced accessibility to periodontal care and the related negative impact on oral health related quality of life |
| Inter-professional collaboration | • Telehealth networks • Online education [54,55] |
Improving the identification of subjects at higher risk for periodontitis as well as of periodontal patients exposed to higher risk for systemic disorders |
3.2. Periodontal Maintenance Care
The optimal recall and maintenance interval, monitoring periodontal health status and controlling risk factors, with the aim to prevent progression and recurrence of periodontal diseases and to reduce the occurrence of tooth loss, which has long been debated [44], should even more accurately be planned in the COVID-19 era, to reduce the number of periodontal maintenance sessions as much as possible, without reducing periodontal health status monitoring, risk factors control and patients' adherence to maintenance care. Compliance with a recall program and oral hygiene reinforcement, motivation and instruction, along with the promotion of smoking cessation, may benefit from teledentistry, especially considering that the necessity of performing subgingival debridement in each session remains controversial [28]. Moreover, combined with periodontitis grading [31, 37], which identifies the case-specific rate of progression, also validated individualized risk factor assessment tools [45], which predict periodontitis progression, may be of support in optimal periodontal recall planning. Teledentistry tools may aid in patients’ self-reported periodontal concerns, on the one hand, and in the case of re-evaluation, on the other, focusing a personalized recall scheduling.
4. PERIODONTITIS PREVENTION DURING AND AFTER THE COVID-19 ERA: POTENTIAL ADDITIONAL MEASURES AIDED BY TELEDENTISTRY
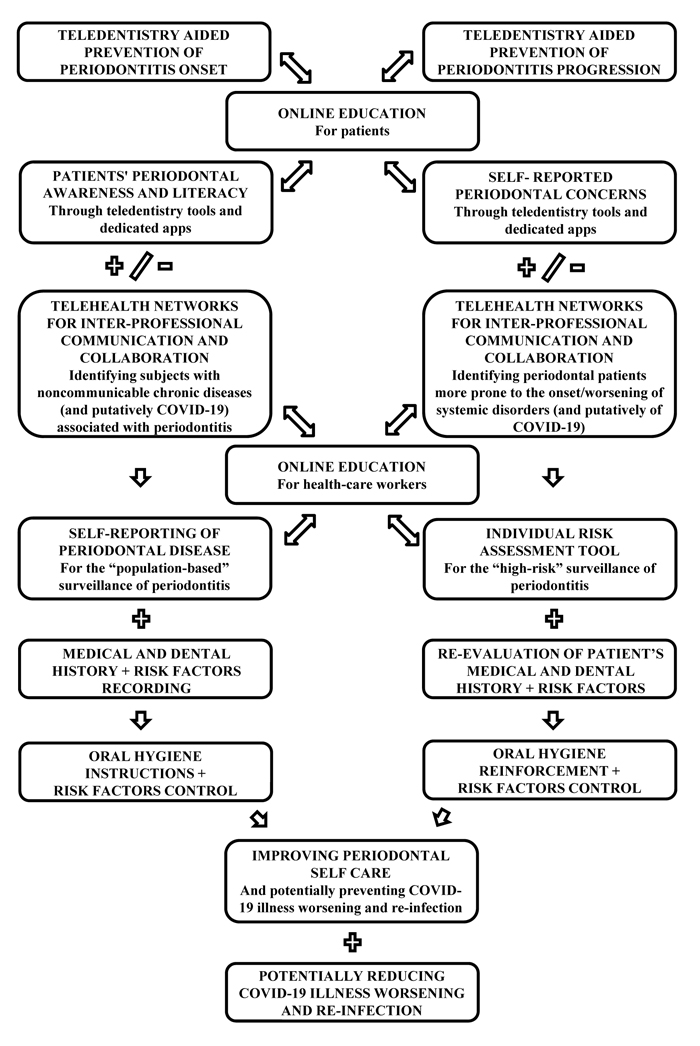
Periodontitis constitutes an important public health problem, most often under-acknowledged and implicated with general health, oral health-related quality of life and socio-economic burden [21], thus, enhancing the prevention of periodontitis onset and progression in the context of the COVID-19 pandemic (Table 2), may be particularly important, while also considering the possibly reduced accessibility to periodontal care.
Therefore, increasing patients’ periodontal awareness and literacy through teledentistry tools and dedicated apps should be added to already existent prevention measures. Teledentistry sessions aiming to improve periodontal self-care, plaque and behavioral risk factors control, especially smoking cessation, may be crucial in periodontal preventive management, especially in the context of the COVID-19 pandemic, and may prevent short-term recall, in compliance with SARS-Cov-2 infection control, and reduce, if not eliminate, the socio-economic gap [21], characterizing both periodontitis severity and access to periodontal care; therefore, this may be considered the keystone of effectiveness and cost-minimization in periodontal prevention.
Moreover, in the attempt to address the prevention of both onset and progression of periodontitis on a large scale with high-quality precision and personalized periodontal care for high-risk subjects [45], periodontitis surveillance, currently based on a combination of “population-based” and “high-risk” approaches, may benefit from newly developed and validated self-reporting of periodontal disease and from the individual risk assessment tool, respectively, also aided by teledentistry.
Flowchart for periodontal disease surveillance, proposed for the prevention of periodontitis onset in periodontally healthy subjects, and progression in periodontal patients, in the COVID-19 era, which is principally aided by teledentistry, is illustrated in Fig. (2).
5. INTER-PROFESSIONAL COLLABORATION DURING AND AFTER THE COVID-19 ERA: HIGH-RISK SUBJECTS
Due to the interconnections between periodontal and general health status [46, 47], subjects considered at a high risk for periodontitis development, as well as periodontal patients more prone to the onset or worsening of systemic disorders, should be regarded with caution in multi-disciplinary settings, that may be aided by telehealth networks, improving the inter-professional communication and collaboration (Table 2).
Particular attention should also be given to a multi-disciplinary approach to older patients since the prevalence of both periodontitis as well as non-communicable chronic diseases associated with periodontitis is higher among adults ≥ 65 years old [48]. Noteworthy, such non-communicable chronic diseases, including cardiovascular disease, diabetes mellitus and cognitive impairment, are known to be risk factors for developing COVID-19 complications [50]. Rising evidence also suggests that periodontitis itself may constitute a risk factor for severe COVID-19 illness, probably due to the putative effect of the co-infection of periodontal pathogens and the SARS-Cov-2 virus [51] and the role of the dysregulated inflammatory response, which is involved in periodontitis pathogenesis [52], as well as in the association between periodontitis and several systemic disorders [48, 51], and has also been observed in severe COVID-19 cases [52].
If these hypotheses, suggesting that periodontitis may negatively affect COVID-19 severity [48, 51], will be verified, oral hygiene and antisepsis and periodontal treatment [53] might be introduced in the management of the subjects diagnosed with mild to moderate COVID-19 illness to prevent illness worsening, and of the healed subjects to prevent re-infection starting from the possible viral reservoir located within the periodontal pockets [48, 50, 51].
Moreover, such recent scientific acquisitions, if validated, should be massively divulged throughout dental research and especially clinical settings also through an enhanced online education [54, 55] (Table 2).
CONCLUSION
Considering the described ergonomic, economic and ethical concerns raised by limited and recurrently discontinued dental and periodontal practice [5, 9, 13, 21, 23], and hoping that the COVID-19 pandemic will be over soon, but being aware of the increasing number of emerging infectious diseases, added to already known ones showing up in new guises, that may, especially if spread by airborne transmission, affect different aspects of the dental practice, including oral manifestations, cross-infection control, and, above all, decision making [56], the common statement declaring that “nothing will be like before after this pandemic” could be considered especially true for oral healthcare providers and periodontists.
Accordingly, the periodontal practice should integrate the measures minimizing cross-infections and the ergonomic improvements optimizing time-space and economic resources, as described in (Table 1), and the teledentistry applications, increasing access to dental care while reducing person-to-person contact and the daily number of patients and healthcare workers in the office, therefore, decreasing PPE use and decontamination procedures costs [57].
The management of periodontal patients may be permanently adjusted (Table 1, Fig. 1) [58], comprising less complex treatments and more comprehensive and definitive approaches, to reduce emergencies, sessions length and number, and, concurrently, extend the recall and maintenance intervals, including teledentistry sessions, essential for patients’ scheduling, remote pre-check triage [57], medical and dental history with periodontal risk factors recording, and communication of therapeutic options, of measures for risk factors control and of oral hygiene instructions, as well as for professionals’ digital settings [57], allowing periodontitis diagnosis, staging, grading and treatment planning, especially in multi-disciplinary cases.
Prevention strategies and flowchart (Fig. 2) may be primarily implemented through teledentistry tools and apps to improve periodontal awareness and self-care, through periodontal risk assessment tools and self-reporting of periodontitis for the “high-risk” and “population-based” surveillance of periodontitis, and through telehealth networks, enhancing interprofessional collaboration, to especially target subjects at high-risk of both periodontitis and systemic disorders, which are variously linked to COVID-19 onset and worsening.
The present evidence-based recommendations on periodontal practice and the management of periodontal patients during and after the COVID-19 era should be constantly reevaluated, according to the continuous flux of novel findings and the state of the art and science.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available in PubMed/MEDLINE (PubMed (nih.gov)) and Science Direct (ScienceDirect.com |) databases.
FUNDING
This article did not receive any funding.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


