All published articles of this journal are available on ScienceDirect.
Comparative Evaluation of Pain Perception in Symptomatic Apical Periodontitis among Smokers and Non-Smokers Patients during Endodontic Treatment. A Clinical Prospective
Abstract
Introduction:
The most common sequelae of events caused by the bacterial ingress into the tooth structures leading to pain is almost always treated by endodontic therapy, which establishes a correlation between pain and endodontics. There are many host modulatory factors that alter pain response. Smoking is one such factor that has a significant effect on human responses, immune responses, along with the risk of infection.
Methods:
A total of 10 non-smokers and 10 smokers having symptomatic apical periodontitis undergoing root canal treatment were selected. The treatment was divided into four appointments, and the patients were asked to record the interappointment pain level on a VAS scale. The data obtained were analyzed using SPSS version 20 software, and the tests employed were independent sample t-test, post-hoc Bonferroni test.
Results and Discussion:
The interappointment pain levels during the endodontic treatment were found to be higher among smokers than non-smokers. Both the groups initially showed the perception of pain, but even at the end of the treatment, smokers were found to have pain. p-value </= 0.5 was considered significant.
Conclusion:
It was concluded from the study that smokers have a higher level of pain perception when compared to non-smokers.
1. INTRODUCTION
The most common sequelae of events are caused by the bacterial ingress in pulp space which leads to pain; this correlation between pain and apical periodontitis results in endodontic therapy. In most cases, when treatment is not sought at the appropriate time, the microbial infection progresses towards the periodontal tissues, leading to progressive destruction of the supporting tissues with pocket formation, recession, or a combination of both [1].
Pain can be an unpleasant sensation, and it depends on psychological factors, such as emotional and motivational status, or it can be due to tissue damage. Any structural and functional alterations within the central and peripheral nervous systems, along with other defensive mechanisms, presence of inflammatory mediators, and other host modulatory factors, can evoke pain response in the individuals [2].
Cigarette smoking is a known factor for an increase in the risk of various systemic diseases; Juan Jose Segura Egea et al. in their study demonstrated that smokers with hypertension had a high prevalence of apical periodontitis than non-smokers, and they also concluded that the patient showed poor periodontal condition [3].
Inter-appointment pain is one of the most common complaints encountered by the patient. Proper knowledge regarding the various etiological factors leading to inter-appointment pain and its mechanism is very important for a clinician to properly avoid or intervene in this undesirable condition. A proper history, correct diagnosis, and efficient treatment planning are required for the practitioner to avoid this undesirable circumstance [4].
Comparisons between smokers and non-smokers have shown that smokers have higher pain perception and, in most cases, have an impact on occupational and social function. Vascular changes leading to a change in blood flow and the increased vasculature and higher Osmotic Pressure (OP) are features of tissue inflammation that lead to a change in homeostasis.
Smoking can lead to a change in the fluid dynamics of any normal tissue, which could further disturb the normal physiological processes, resulting in various inflammatory responses and changes in the pain pathways [5, 6].
Various forms of consumption of tobacco, including cigarette smoking which is a form of nicotine, can have an altered pain mechanism in the tissue [6]. Smoking causes altered phagocytic response and chemotaxis of neutrophils. It also produces protease inhibitors, prostaglandin E 2, and free radicals in two different tissues [7].
Hence, the aim of the study was to assess and compare the inter appointment pain perception among the smoker and non-smoker patients with symptomatic apical periodontitis during endodontic treatment using a standard and significant method.
2. METHODOLOGY
Twenty patients in the age group of 25-40 years were selected, out of which 10 patients were cigarette smokers(approximately between 5 to 10 in a day) having symptomatic apical periodontitis and 10 patients were non-cigarette smokers having symptomatic apical periodontitis, which were categorized as Group 1 and Group 2, respectively. All the selected patients were diagnosed thoroughly with proper clinical findings and other investigation procedures. Patients with a tooth with pus drainage, sinus opening, and swelling or with systemic health diseases were excluded from the study. Patients with symptomatic apical periodontitis (anterior or posterior tooth) irrespective of the location, placement of tooth in the dental arch, or the number of tooth roots were included in this study.
The same practitioner performed all the procedures using a single-use pre-sterilized rotary files system on each patient, and consent forms were given to every patient prior to the procedure.
The aim of the study was to assess the inter appointment pain perception and to evaluate the pain perceived specifically in each step of the root canal therapy, and the treatment was scheduled in four appointments to prevent any variable changes in the pathology and treatment flare-ups.
Appointment 1- access opening and pulp extirpation under LA (2%Lidocaine, Warren)
Appointment 2- working length determination and hand filing with 8, 10,15k file (Mani K file)
Appointment 3- biomechanical preparation using rotary files (Helix rotary system, Helix health care)
Appointment 4- obturation using 25(6) % gutta-percha cones (Dentsply)
A pain assessment chart was given to the patients, and the pain level was recorded in a calibrated horizontal Visual Analogue Scale (VAS). The VAS scale is easy to use, easy to understand, a handy tool for patients, reliable, valid, and a quantitative predictor for evaluating pain. In the current study, the standard protocol of VAS has been recorded with an initial calibrated at zero, signifying no pain, and ten, which signify the most intense pain. Antibiotic or analgesic coverage was not administered to the patients who participated in the study until obturation and temporary post- endodontic restoration.
3. RESULTS
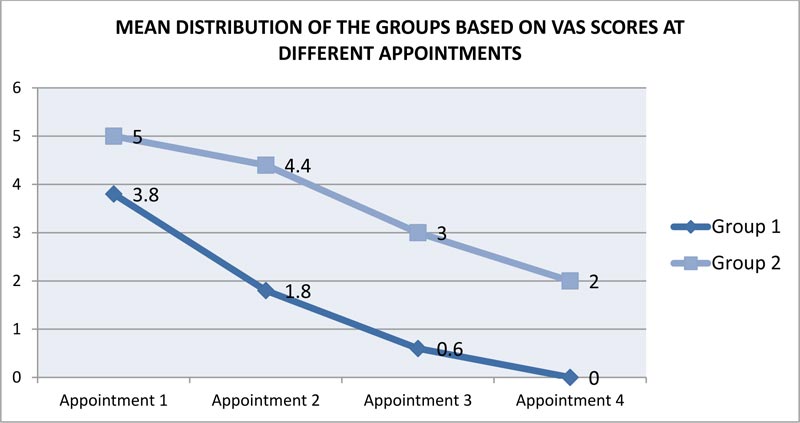
Descriptive statistics such as mean and standard deviation were used to present values (Fig. 1). Comparison of the groups at different appointments was analyzed using an independent sample t-test. Individual comparison of each appointment with the other appointments of the same group was analyzed using the post-hoc Bonferroni test. The data were analyzed using SPSS version 20 software. p-value </= 0.5 was considered significant.
| - | - | Minimum | Maximum | Mean | Std. Deviation | |||
|---|---|---|---|---|---|---|---|---|
| Group 1 | Appointment 1 | 2 | 6 | 3.80 | 1.135 | |||
| Appointment 2 | 0 | 4 | 1.80 | 1.476 | ||||
| Appointment 3 | 0 | 2 | .60 | .966 | ||||
| Appointment 4 | 0 | 0 | .00 | .000 | ||||
| Group 2 | Appointment 1 | 4 | 6 | 5.00 | 1.054 | |||
| Appointment 2 | 2 | 6 | 4.40 | 1.265 | ||||
| Appointment 3 | 0 | 4 | 3.00 | 1.414 | ||||
| Appointment 4 | 0 | 4 | 2.00 | 1.333 | ||||
| - | Mean difference | t value | p-value |
|---|---|---|---|
| Appointment 1 | -1.2 | -2.4 | 0.025* |
| Appointment 2 | -2.6 | -4.2 | 0.001* |
| Appointment 3 | -2.4 | -4.4 | 0.00* |
| Appointment 4 | -2.0 | -4.7 | 0.00* |
Table 1 shows the mean distribution of groups 1 (non-smokers) and 2 (smokers) based on VAS scores of pain perception at different appointments. The mean difference of pain values among the two groups were compared at all four appointments independently and
The mean difference of pain values among the two groups were compared at all four appointments independently and were found to be statistically significant at each appointment (Table 2 and 3).
4. DISCUSSION
Smokers seem to have a worse endodontic outcome than non-smokers, and also have a higher chance of developing periodontal infections, and were 1.7 times more likely to undergo an endodontic therapy, along with a delayed bone healing process than non-smokers [7].
| Groups | Appointment | Appointments | Mean Difference | p-value |
|---|---|---|---|---|
| Group 1 | Appointment 1 | Appointment 2 | 2.00 | .006* |
| Appointment 3 | 3.20 | .000* | ||
| Appointment 4 | 3.80 | .000* | ||
| Appointment 2 | Appointment 3 | 1.20 | .306 | |
| - | Appointment 4 | 1.80 | .023* | |
| Appointment 3 | Appointment 4 | .600 | .487 | |
| Group 2 | Appointment 1 | Appointment 2 | .600 | .487 |
| Appointment 3 | 2.00 | .006* | ||
| Appointment 4 | 3.00 | .000* | ||
| Appointment 2 | Appointment 3 | 1.40 | .008* | |
| - | Appointment 4 | 2.40 | .000* | |
| Appointment 3 | Appointment 3 | 1.00 | .090 | |
A study relating cigarette smoking and apical periodontitis describes smoking as a risk factor for endodontic therapy. The roles of macrophages, polymorphonuclear leukocytes, antibodies, T-cell lymphocytes, and immunoglobulins A, G, and M are suppressed in smokers (Holt, 1987). The amount of TNF-α (Tappia et al., 1995) and IL-6 (de Maat and Kluft, 2002), which are acute-phase inflammatory mediators, were found to be elevated in smokers. A study by Frohlich et al. found the levels of peripheral leucocytes and C-reactive Protein (CRP) higher in smokers than in non-smokers. These findings suggest that once microbes start forming colonies and cause pulpal and periodontal infections, the rate of destruction is seen more in smokers than non-smokers [7].
Smokers have an impaired oxygen delivery and thereby an increased level of carboxyhemoglobin [7]. A lot of cellular processes are affected by the heme oxygenase and the carbon monoxide system, including oxidative stress, apoptosis, and inflammation. Heme oxygenase is a causative factor in the development of neuropathic pain. Decreased oxygen levels may increase the rate of degenerative processes, making the body more prone to injury [5].
There is a decreased expression of IL-1β, TNF-α, and hBD-2 among smokers [8] because of the reduced expression of inflammatory mediators. Individuals show an impaired defensive mechanism to resist the infection and are at a higher risk of manifesting symptoms after endodontic therapy of infected root canals. The reduced bleeding in smokers has been mainly due to gingival vasoconstriction, which is influenced by the actions of nicotine-stimulated adrenaline and noradrenaline on α1- adrenergic receptors [1]. Smoking has a vasoconstrictive effect, resulting in a decreased blood flow in the tissue. Nicotine causes the release of catecholamines (adrenaline, noradrenaline, and isoprenaline), leading to a continuous unrelieved sensation of pain [6].
Demirurek et al. have emphasized the significance of pulpal osmotic pressure variations among smokers and non-smokers. As the smoking is increased, the pulpal pressure is decreased, and the result shows reduced blood flow to the pulp, leading to different tissue responses [5-7]. Literature has shown an increase in the level of one of the neuropeptides, Calcitonin Gene-related Peptide (CGRP), among smokers, which had an influence on the pulpal blood flow and pulpal inflammation. These findings indicate that smoking has a negative influence on the circulatory system and the autonomic nervous system, which can cause an imbalance in the dental pulp and affect the normal functioning of the pulpal tissue [6].
Osmotic pressure is associated with vascular permeability and the rate of blood flow. A decrease in the pulpal osmotic pressure can have an influence on the severity of dental pain. Under ischemic conditions, the amount of blood flow through the tissue is also decreased, affecting the vitality of the pulp and resulting in early signs of inflammation [6].
Minimum studies were conducted correlating the pain response among smokers and non-smokers, and evidence suggests that chronic administration of nicotine induces a change in the endogenous pain mechanisms and has a greater intensity of pain perception. Nicotine administration can lead to an increase in stress production because of a beta-endorphin deficiency [9].
During the endodontic therapy, the oxidation-reduction potential of a root canal is altered, and as a result, an acute exacerbation can occur [4], leading to a delayed wound healing, and can also lead to an increase in pain perception after trauma, surgery, or other injuries [5].
Literature has shown that smoking has an influence on the central nervous function, which can exist even after the cessation of smoking. The smokers reported higher pain scores along with the persistence of chronic pain and had a lower amount of serum hydrocodone levels when compared with non-smokers [4]. Smoking can even be a predisposing factor for various conditions like lumbar disc diseases, impaired bone healing, and osteoporosis [5].
Ducan et al. in their review article, expressed the influence of cigarette smoking during endodontic treatment, and they described that nicotine can interfere with wound healing and can enhance microcirculation; this mechanism can result in platelet aggregation and endothelial cell dysfunction, resulting in vasoconstriction and reduced tissue perfusion [10].
In the present study, the mean distribution of pain perception between the two groups Table 1 has shown that pain perception was higher among smokers, and the pain was felt by most of the participants throughout the treatment procedure. Among non-smokers, pain perception was highest at the first appointment, and as the treatment progressed, a reduction in the pain perception was seen. In group 1(non-smokers), only at appointment 1 (access opening), the participants showed a minimum value of 2 and a maximum value of 6. In appointments 2 and 3, the minimum value was shown to be 0 while the maximum value graded was 4 and 2, respectively. Appointment 4 showed no pain perception among the participants. In group 2 (smokers), at appointments 1 and 2, the minimum value was graded at 4 and 2, respectively, but the maximum value was shown as 6. Appointments 3 and 4 had found to have the same values. When the two groups were compared independently at all four appointments Table 2, the results were found to be statistically significant at each appointment.
The present study has shown that both the groups (Group 1 and Group 2) exhibited preoperative pain, but at the end of the treatment, pain perception signifies a higher percentage among cigarette smokers compared to non-cigarette smokers.
CONCLUSION
Endodontic therapy is the treatment of choice when the microbial ingress affects the pulp and periodontal apparatus. There is a difference in the response towards pain, which is exhibited by non-smokers and smokers. The results of this study showed that smokers exhibited more pain and poor healing when compared to non-smokers. Throughout the study, a chronic persistence of pain response was seen among smokers. The results showed that smoking causes a change in pain modulation, thereby increasing the level of pain perception.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was obtained from Navodaya Dental College ,India (ref:Ndc/01/2019).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Consent form issued to the individual patient for participation.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank Ajman University for facilitating our research work and their continuous help and support.


