Degenerative Changes in the Temporomandibular Joint in Elderly Patients with Posterior Edentulous Maxilla and Mandibula According to Cone-Beam Computed Tomography Data.
Abstract
Aim:
This study aimed at assessing the degenerative changes in the Temporomandibular Joint (TMJ)in elderly patients with posterior edentulous maxilla and mandibula according to Cone-Beam Computed Tomography (CBCT) data.
Materials and Methods:
The study included 32 patients (64 temporomandibular joints) aged from 50 to 81 years (mean age 62 ± 7.9 years; 16 males and 16 females). TMJs were visualized on reconstructed parasagittal, paracoronal, and axial sections of the joint. The following changes in bone tissue were evaluated: condyle flattening, erosion, sclerosis, subchondral cysts, osteophytes. Joint space was evaluated as well.
Results and Discussion:
100% of patients had at least one sign of degenerative changes in TMJ at least on one side. In 19 patients, degenerative symptoms were found only on one side. The most common sign was subchondral cysts. It was noted that the number of degenerative symptoms in male patients was statistically more than in the female group. On the right side, the anterior, superior, and posterior joint spaces had the following values: 2.35 mm, 2.95 mm, and 4.84 mm, respectively. On the left side, the anterior, superior, and posterior joint spaces had the following values: 2.14 mm, 2.3 mm, and 4.1 mm, respectively.
Conclusion:
Both edentulousness and aging affect the bone structure of TMJ in both genders.
1. INTRODUCTION
Temporomandibular Joint (TMJ) is a complex joint containing both bone and soft tissue components [1]. TMJ is a bilateral synovial joint responsible for the range of mandibula motions, that allows speaking, chewing, and breathing [2]. Temporomandibular Joint Diseases (TMD) are a diverse group of conditions, often with a multifactorial etiology, that can affect one or all of the TMJ components, including bone and soft tissue elements (for example, the articular disc and capsule), supporting elements, and functional elements such as muscles and ligaments. TMD are the most common cause of extraoral pain with a variety of manifestations, including muscle pain, preauricular pain, headache, joint sounds such as clicking and crepitus, and limited or asynchronous mouth opening. Approximately 40-75% of the adult population is asymptomatic but they have at least one sign of joint dysfunction (noise, mandibular movement disorders, etc.) [3].
Moreover, age is considered the main factor associated with degenerative changes in the TMJ [4]. According to different studies, a functional overload, caused by the inability to replace lost teeth, in the TMJ occurs, which leads to TMD during the entire aging process [5, 6]. TMD associated with degenerative changes are characterized by degeneration of the articular cartilage and bone tissues and can lead to pain, discomfort, and joint hypomobility [7].
Cone-beam Computed Tomography (CBCT) and Magnetic Resonance Imaging (MRI) are some of the methods for three-dimensional (3D) TMJ evaluation [8, 9]. The morphology of the TMJ bone components, the integrity of the cortical bone, and changes in the subcortical bone can be observed with CBCT with higher sensitivity. CBCT is a relatively low dose and cost-effective imaging option, providing high-quality images for the diagnostic evaluation of TMJ bone abnormalities [6, 10, 11]. Degenerative changes in the TMJ bone components include erosion, flattening, sclerosis, subchondral cysts, and osteophytes. The joint space also decreases as a result of the loss of the joint cartilage tissue [3]. Knowledge of these bone changes is fundamental for the diagnosis of dysfunctions associated with TMD [12].
The aim of this study was to evaluate the degenerative changes of the TMJ in older patients with missing teeth in the posterior maxilla and mandibula with CBCT.
2. MATERIALS AND METHODS
This retrospective study included 32 patients (64 temporomandibular joints) aged 50 to 81 years (mean age 62 ± 7.9 years; 16 males and 16 females). Patients were edentulous in the posterior maxilla and mandibula from seven to 15 years. The included group had no partial removable dentures (or did not use them during the edentulous period). Eight patients underwent periodontal treatment. Written consent for CBCT examination was signed by all patients prior to the examination.
The following inclusion criteria were applied:
(1) No history of TMD;
(2) No systemic diseases that can affect the structure of the TMJ components;
(3) No congenital diseases or syndromes;
(4) Right and left temporomandibular joints are fully visualized on the CBCT scans;
(5) Absence of artifacts on CBCT scans.
(6) Patients presented and complained of no TMD symptoms.
CBCT-scans were obtained using an eXam® computer tomography (KaVo, Biberach, Germany) with standard settings (scan area 23 * 17 cm; voxel size 0.3 mm; 110 kV; 1.6–20 s). Measurements were carried out using OsiriX MD 10.0 software (Pixmeo SARL, Bernex, Switzerland).
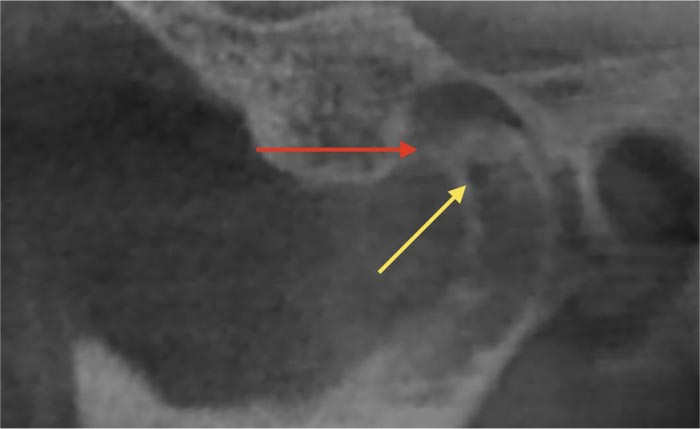
The right and left temporomandibular joints were visualized on sagittal (perpendicular to the longitudinal axis of the condyle), coronal (parallel to the longitudinal axis of the condyle), and axial sections of the joint. The following changes in bone tissue were assessed (Fig. 1 and 2): flattening of the condyle (flat bone contour), erosion (area of reduced density of the cortical bone), sclerosis (area of increased density of the cortical layer), subchondral cysts (osteolytic area of the bone without destruction of the cortical layer), osteophytes (marginal bone outgrowths - exostoses).

The articular space was also assessed on the sagittal reformat according to the following algorithm (Fig. 3):

(1) A line is drawn from the top of the articular tubercle to the petrotympanic fissure;
(2) A perpendicular is drawn from the center of the articular head to the above line, then the bisectors of the obtained right angles are built.
(3) Measurements of the anterior, superior, and posterior spaces were carried out along three corresponding lines in the area of the joint space.
NOVA analysis of variance was performed along with student's test with a significance level of p <0.05 in StatPlus software (AnalystSoft Inc. WALNUT, CA, USA) to evaluate the results obtained and comparative characteristics were carried out.
3. RESULTS
In this study of 64 temporomandibular joints in elderly patients with missing teeth in the posterior maxilla and mandibula using CBCT, 100% of patients had at least one sign of degenerative changes in the TMJ on at least one side. In 19 patients (59.3% of the total number of patients; 13 women and 6 men), the degenerative sign manifested only on one side. The remaining 13 patients had degenerative changes in both TMJs. In general, the most common symptom (p = 0.6) was subchondral cysts (Table 1) with no statistical significance, which is also true for the group of men (p <.05), while sclerosis was more common in women (p = 0.8). It was also noted that the number of degenerative signs in men was statistically higher than in women (p <.05).
| Sign | Total % - of the Total Number of Joints (N-Joints) |
Men % - of the Total Number of Joints in Men (N-Joints) |
Women % - of the Total Number of Joints in Women (N-Joints) |
|---|---|---|---|
| Erosion | 15.6% (10) | 18.7% (6) | (4) |
| Flat contour | 3.1% (2) | 3.1% (1) | 3.1% (1) |
| Subchondral cysts | 34.3% (22) | 50% (16) | 18.7% (6) |
| Osteophytes | 14.1% (9) | 18.7% (6) | 9.3% (3) |
| Sclerosis | 20.3%(13) | 18.7% (6) | 21.8% (7) |
| Space | Right (mm) | center (mm) | Difference (mm) | Number of Patients with a Difference Above Average | p-value |
|---|---|---|---|---|---|
| Anterior (AS) | 2.35±0.65 | 2.14±0.73 | 1.17±0.7 | 19(59.3%) | 0.3 |
| Superior (SS) | 2.95±1.33 | 2.3±1.07 | 1.6±0.99 | 13 (40.6%) | 0.1 |
| Posterior (PS) | 4.84±1.88 | 4.1±1.7 | 2.4±1.6 | 15 (46.8%) | 0.3 |
At the second stage of this study, the space between the condylar head and the glenoid fossa of the TMJ was assessed (Table 2). The difference between the spaces on the right and left was not statistically significant. However, noteworthy is the fact that both on the left and the right, the posterior articular space was statistically larger (p. <05) than the anterior articular space, followed by the superior articular space, however, the difference between the anterior and superior spaces was not significant at both sides. This feature indicates a bilateral displacement of the condylar head anteriorly in the closed position of the temporomandibular joint.
4. DISCUSSION
It is known that degenerative joint diseases can also involve TMJ, and this feature is more common in elderly patients [13]. Also, a number of studies have argued that the absence of teeth leads to remodeling of the glenoid fossa, degeneration, and structural changes in the TMJ [14-16]. In our study, both factors were taken into account simultaneously: age and missing teeth.
Dumbuya et al. [13] in their study noted degenerative changes in the TMJ in 65.7% of patients on at least one side. This prevalence is comparable to the findings of dos AnjosPontual et al. [12] with 71% and Massilla et al. [17] with 80%. In these studies, only the age factor was taken into account. In our study, 100% of patients had degenerative changes in at least one TMJ.
In this study, the number of women with at least 1 affected TMJ was higher than men. These data are comparable with studies carried out earlier [6, 10, 18]. This feature is explained by the fact that women have hormonal effects of estrogen and prolactin, which can increase the degradation of cartilage and bone [19]. However, in our study, men have a greater total number of degenerative signs of TMJ.
Nowadays, the prevailing opinion is that the position of the condyle can be a valuable diagnostic tool in TMD [20]. The joint spaces of the temporomandibular joint are a critical point, which was considered as an indicator of the possibility of condyle movement [21]. Ikeda et al. [22] studied the position of the condyle in patients with no signs of TMD. Their dimensions of the anterior, superior, and posterior articular spaces were 1.3 mm, 2.5 mm, and 1.6 mm, respectively. Imanimoghaddam et al. [23] presented the following data for the anterior, superior, and posterior articular spaces: 2.3 mm, 3.3 mm, and 2.1 mm, respectively. In this study, the posterior articular space had higher values.
This feature is associated with the factors, such as density, width, and index, indicating the complexity of the TMJ trabecular bone, which decreases in patients with missing teeth [24]. Adaptive changes can occur in the region of the articular tubercle, and its flattening can be the result of this adaptation, leading to an anterior displacement of the head of the condylar process [25].
CONCLUSION
This study showed that the absence of teeth in the posterior regions of both maxilla and mandibula and aging affect the bone structures of the TMJ in both genders. CBCT scans can provide useful information about the position and morphology of TMJ components, which can be useful in diagnosing the joint in all patient groups. That is why it should be included in the diagnosis plan of the patients with posterior maxillary and mandibular edentulism.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written consent for CBCT examination was signed by all patients prior to the examination.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


