The Digital Diagnostic Approach to Stafne’s Bone Cavity (SBC): From a Review of the Literature to the Description of a Clinical Case.
Abstract
Introduction:
Stafne’s Bone Cavity [SBC] is a rare, well-defined, mandibular bone lesion, which was first discovered by Edward C. Stafne in 1942.
Objective:
The purpose of this article is to evaluate a digital diagnostic approach to Stafne’s Bone Cavity (SBC) through a review and description of some clinical cases.
Methods:
The review was conducted through an analysis of the literature of all articles published on Stafne’s Bone Cavity.
We report the case of a 55-year-old male patient who needed tooth implant rehabilitation, and therefore, a panoramic radiograph was taken as part of the routine evaluation and plan of care. After the diagnosis, the focus was on more precise imaging and the merits of choosing Computerized Tomography or Magnetic Resonance Imaging were compared.
Results:
According to our review of the literature, the prevalence of these cavities was found to be 0.14%, while 8% of them were found in male patients and 72% of them were found in male patients older than 44 years of age.
The patient’s panoramic radiograph revealed the presence of an SBC in his left posterior side of the mandible. In order to confirm and improve the diagnosis, the patient underwent a Computer Tomography exam, chosen for its benefits outweighing those of an MRI.
Conclusion:
Stafne’s bone cavity (SBC) is indeed an uncommon finding as it is asymptomatic and is identified only through panoramic imaging, CT scans or MRIs. However, it can pose some logistical problems in the application of dental implants. The typology of this case study confirmed the findings of the systematic review; the patient, being a middle aged male, presented a mandibular SBC, which was discovered only during a routine panoramic x-ray to plan the fitting of dental implants. The use of tomography confirmed the diagnosis of SBC and detailed the anatomical structure, thus guiding the restoration process.
1. INTRODUCTION
In 1942, Edward C. Stafne [1] found thirty-five bone cavities in 44 patients situated near the angle of the mandible; 80% of them were located in male patients and the average age of the patients was 47-53 years. The cavities had a diameter variable between 1 and 3 cm, a round or oval form, no preponderance of findings in one of the sides, no change or increase in size, and in only one case, they were present on both sides.
| Author[s] [Ref] | Year | Cases | Nationality | Cross-section | Number of SBCs | Rate of SBCs [%] |
|---|---|---|---|---|---|---|
| Lilly et al. [2] | 1965 | 1,283 | USA | Dentists | 2 | 0.16 |
| Karmiol and Walsh [3] | 1968 | 4,693 | USA | Veterans | 18 | 0.38 |
| Johonson [4] | 1970 | 2,486 | USA | Veterans | 10 | 0.40 |
| Oikarinen and Julku [5] | 1974 | 10,000 | Finland | Patients | 10 | 0.10 |
| Uemura et al. [6] | 1976 | 3,000 | Japan | Patients | 10 | 0.33 |
| Ehara et al. [7] | 1977 | 10,000 | Japan | Patients | 21 | 0.21 |
| Chen and Ohba [8] | 1978 | 23,000 | Japan | Patients | 24 | 0.10 |
| Correll et al. [9] | 1980 | 2,693 | USA | Veterans | 13 | 0.48 |
| Sisman et al. [10] | 2012 | 34,221 | Turkey | Patients | 29 | 0.08 |
| Assef et al. [11] | 2014 | 14,005 | Germany | Patients | 11 | 0.08 |
| All US studies | 11,155 | USA | All | 43 | 0.39 | |
| All Japanese studies | 36,000 | Japan | Patients | 55 | 0.15 | |
| All patients | 98,919 | All | Patients | 123 | 0.12 | |
| Total | 105,381 | All | All | 148 | 0.14 |
These rare, asymptomatic, radiolucent, well-demarcated, mainly unilateral and anterior lesions are commonly called Stafne’s Bone Cavities (SBC) from the surname of the first discoverer, but they are also known as latent, idiopathic or developmental mandibular bone cavities, cysts, defects or depressions.
In the literature, ten published studies have been found on the prevalence of the SBC in the population conducted between 1965 and 2014, and the average rate of SBCs was found to be 0,14%; all the studies carried out by American researchers suffered from the bias of an only-male (in the cases of military veterans) or a mostly-male (in the case of the dentists in 1965) population, so excluding those studies, the average rate decreased to 0.12%. Unfortunately, there are no American studies without gender bias, so investigating the eventual presence of the highest SBCs rate in both sexes in the USA is not possible; however, the rate reported by Lilly et al. [2] is very close to the average world rate, so it may be reasonable to think that the real American average rate of the prevalence of these cavities is no different from the other countries (Table 1).
Some of these studies allowed us to consider the gender variability, and we found that 88% of the cases of SBCs were diagnosed in male patients. In the study of Sisman et al. [10], it was possible to obtain additional confirmation of this aspect, as the prevalence of SBC in male patients was ten times higher than the prevalence in female patients (Table 2).
The same studies reported in Table 2 and the study by Correll et al. [9] allowed us to evaluate age variability as well, and we found that 72% of the cases of SBCs were diagnosed in patients with an age range between forty-five and ninety-five years. The study of Sisman et al. [10] confirmed this data as the prevalence of SBC in patients between the ages forty-one and ninety-five resulted in being twenty-seven times higher than the prevalence in patients between the age of four and forty (Table 3).
| Author[s] [Ref] | Year | 45+ old | Nationality | Number of SBCs |
Rate of SBCs% |
|---|---|---|---|---|---|
| Oikarinen and Julku [5] | 1974 | 8 | Finland | 10 | 80 |
| Uemura et al. [6] | 1976 | 8 | Japan | 10 | 80 |
| Chen and Ohba [8] | 1978 | 14 | Japan | 24 | 58 |
| Correll et al. [9] | 1980 | 11 | USA | 13 | 85 |
| Sisman et al. [10] | 2012 | 21 | Turkey | 29 | 72 |
| Assaf et al. [11] | 2014 | 8 | Germany | 11 | 73 |
| Total | 70 | 97 | 72 |
2. CASE REPORT
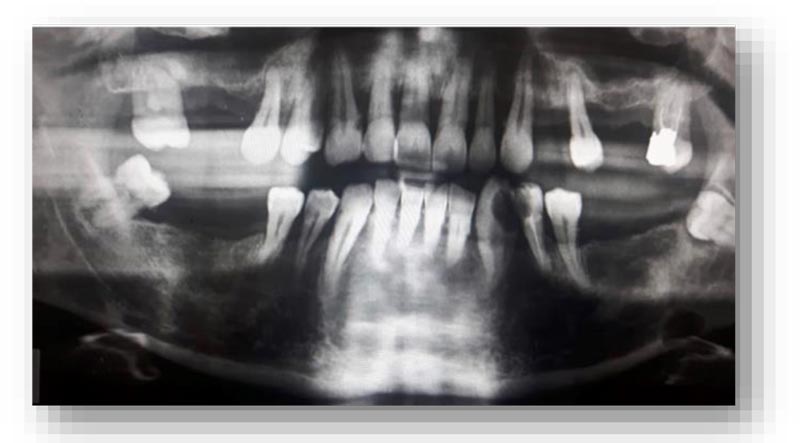
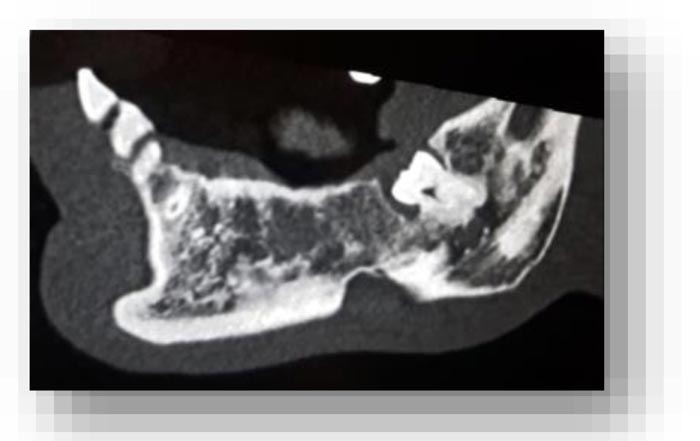
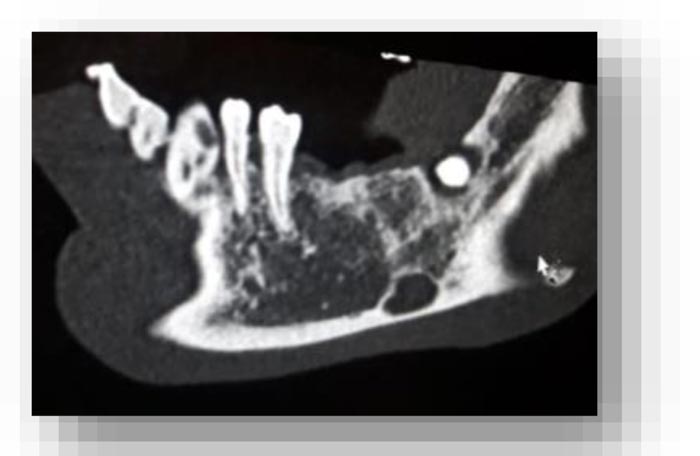
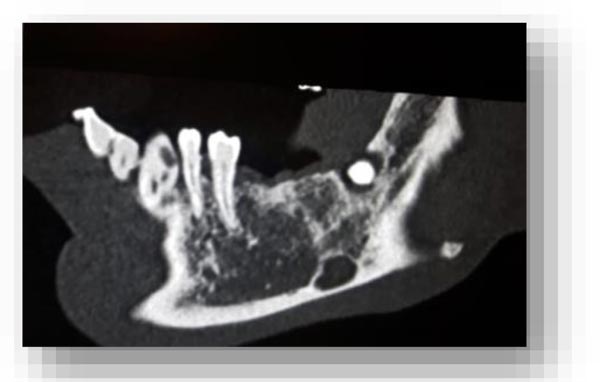
A 55 year-old male patient had routine panoramic radiography done in preparation for prosthetic rehabilitation (Fig. 1). The panoramic imaging revealed an oval cyst-like well-defined lesion (Fig. 2) in the left posterior mandible, anterior to the mandibular angle and the third molar, below a wide edentulous area. The patient was asymptomatic, and there was no report of paresthesia or anesthesia.
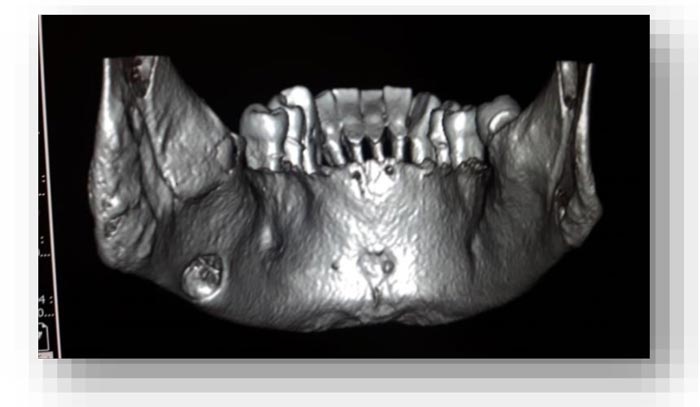
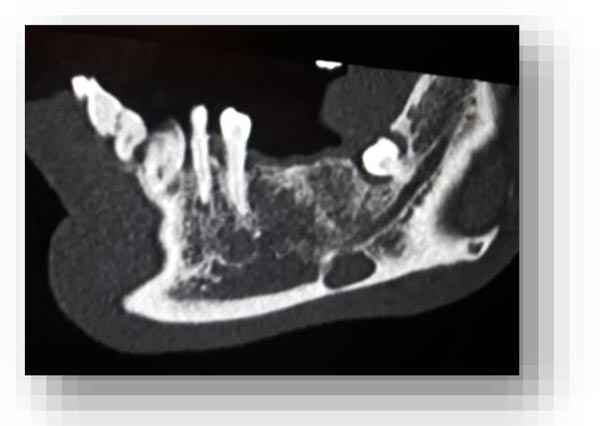
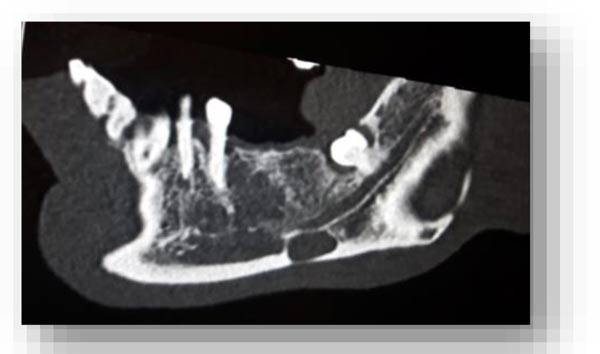
From the objective exam and the panoramic radiography, we observed the presence of multiple edentulous areas which needed to be rehabilitated. As part of an implant-prosthetic plan of care, Spiral Computerized Tomography was prescribed to him (Fig. 3), obtaining bi-dimensional reconstructions as panorex, parasagittal slices by multiplanar reformation and tridimensional reconstructions by volume rendering [12, 13].
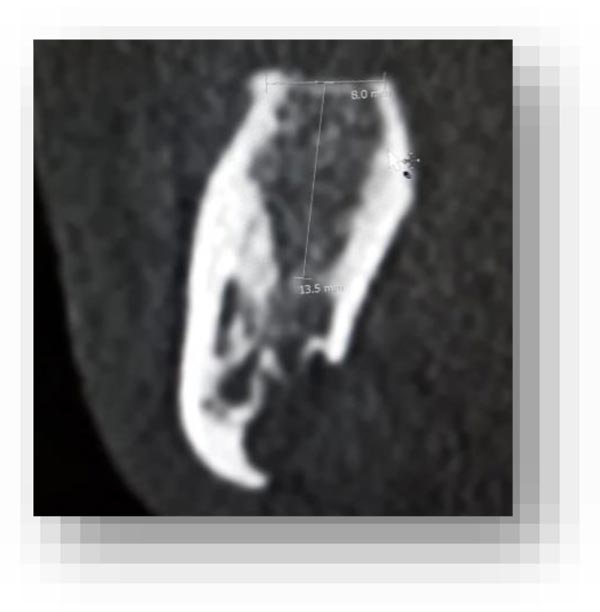
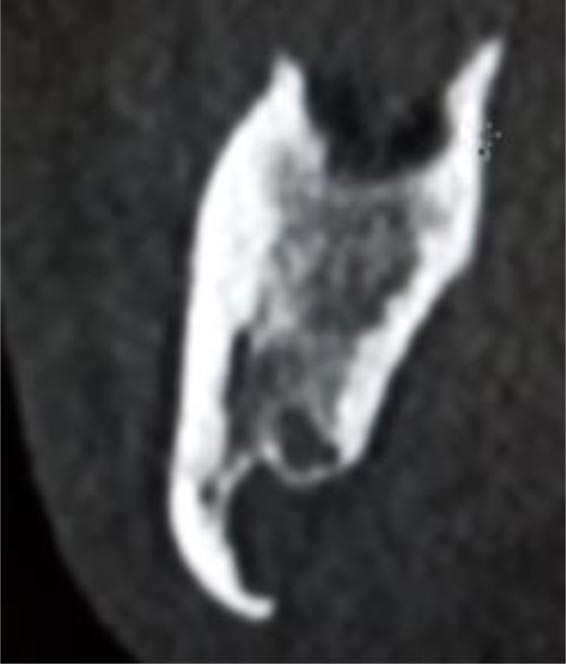
In this radiographic exam, we found an oval notch with radiolucent, clear and regular borders, located in the inferior portion of the horizontal branch of the mandible, on the lingual side, near the angle of the mandible, and below the mandibular canal. The X-ray allowed precise measurement showing a height ranging between 13.5 mm and 17 mm and breadth between 6 and 8 mm (Figs. 4-5).
The bi-dimensional reconstructions in parasagittal slices also permitted better identification of the closeness of the bone cavity to the canal of the alveolar inferior omolateral nerve, whereas the computerized volume rendering offered a more accurate view of the surrounding anatomical features (Figs. 6-12).


3. DISCUSSION
The case that we have described here corresponds to the most common manifestation of SBC and confirms the finding of the studies reviewed; the bone cavity is present in a male sex patient, a mature adult (age 55), in a position located posteriorly in the mandible.
| Advantages | Disadvantages | |
|---|---|---|
| CT | High level of resolution | Exposure to radiation |
| Ease of use | Soft tissues not well visualized | |
| Low cost | ||
| Comfortable for the patient | ||
| May be used in dental offices | ||
| MRI | Good visualization of soft tissues | Distortion artifact caused by metal |
| No exposure to radiation | Higher cost | |
| Less comfortable for the patient | ||
| Less ease of use |
The very low prevalence of this lesion, 0.14%, according to our review, is the main reason why the majority of the studies in the literature are case reports, with very few retrospective analyses and no systematic reviews.
Given the paucity of cases reported, it would be interesting in the future to explore other aspects of the SBC that could make its finding more common, such as investigating whether or not there is a specific original event that could have caused or contributed to the formation of the bone cavity, such as metabolic disorders, traumas, dental extractions, or a past dental abscess. Finding a common factor could guide the use of proper diagnostic tools and prosthetic procedures. Although rare, it would be useful to understand the long-term impact of SBCs, especially vis-a-vis the normal life of implanted prosthetics.
It is impossible to diagnose an SBC with just an objective examination because it is usually asymptomatic, so thanks to radiographic exams that dentists can identify this lesion and often this finding is serendipitous, happening when the imaging is performed for other purposes, as it happened in this case.
After visualizing the bone cavity by panoramic x-rays, we requested a Computerized Tomography (CT) scan, because it is a very versatile and powerful instrument for dental diagnosis and it has additional advantages for the volumetric reproduction of cranium and soft tissues, the absence of the overlap of anatomic parts that limits the visibility of the structures and the presence of a constant and easily reproducible reference system [14, 15].
In literature, some authors were observed to prefer the use of Magnetic Resonance Imaging (MRI). Probst et al. [16], preferred the use of an MRI instead of a CT because it does not emit radiation and it reproduces the soft tissues better than the CT, whereas Boffano et al. [17] recommended the use of a CT scan because MRI is very expensive and distortion artifacts may result from the presence of metal. Moreover, Sisman et al. [10] observed that a CT scan can be easily done in dental offices and it is reported to have a higher level of image resolution than the MRI, whereas Segev et al. [18] defined MRI as a primary diagnostic technique where SBC is suspected, underlining that the use of intravenous contrast material is not necessary for these lesions (Table 4).
In addition, in cases of an atypical SBC and a very difficult differential diagnosis, Li et al. [17] suggested the combination of CT and sialography, if needed, although this technique may be difficult to perform and uncomfortable for the patient.
Because the SBC is an asymptomatic and non-developmental lesion, the most suggested approach in the literature is conservative and the majority of the studies advised a follow-up radiographic examination; especially, Probst et al. [16] judged the radiographic follow-up as a reasonable recommendation, considering the possible progression reported by Prechtl et al. [20].
According to Venkatesh [21], CT should be used in the follow-up, whereas Boffano et al. [16] concluded that both CT and MRI are suitable for the follow-up, while Schneider et al. [22] explicitly affirmed that panoramic radiograph seems to be insufficient for this purpose.
Because the CT entails a higher exposure of radiation compared to a panoramic X-ray, a legitimate question could be the frequency of the follow-ups with radiographs. Dereci and Duran [23] proposed an X-ray to be conducted in 6 months follow-up and they monitored the symptomatology of the patient for 2 years, whereas Queiroz et al. [24] followed the patient for 4 years but used panoramics. Other studies have also advised a 6-month follow-up period, but many authors suggest that the follow-up should be regular and adequate.
CONCLUSION
Stafne’s bone cavity (SBC) is indeed an uncommon finding, as it is asymptomatic and is identified only through panoramic imaging, CT scans or MRIs. However, it could pose some logistical problems in the application of dental implants. The typology of this case study confirmed the findings of the literature review, the patient being a middle age man presenting a mandibular SBC, discovered only during a routine panoramic x-ray to plan for the fitting of dental implants. The use of tomography confirmed the diagnosis of SBC and its anatomical structure, thus guiding the restoration process. Considering all the advantages of a CT scan compared to an MRI, such as the lower cost, a higher level of resolution, a higher level of comfort for the patient, the absence of distortion artifacts caused by intraoral metal and the facility of use, we recommend a CT scan in oral reconstruction, so as not to miss possible cases of SBC.
The article has been translated into American English by Licia Coceani Paskay, MS, CCC-SLP.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial, or otherwise.
ACKNOWLEDGEMENTS
Declared none.


