All published articles of this journal are available on ScienceDirect.
Management of Membrane Exposure Utilizing Concentrated Growth Factor (CFG) in Guided Bone Regeneration: A Clinical Report
Abstract
Introduction:
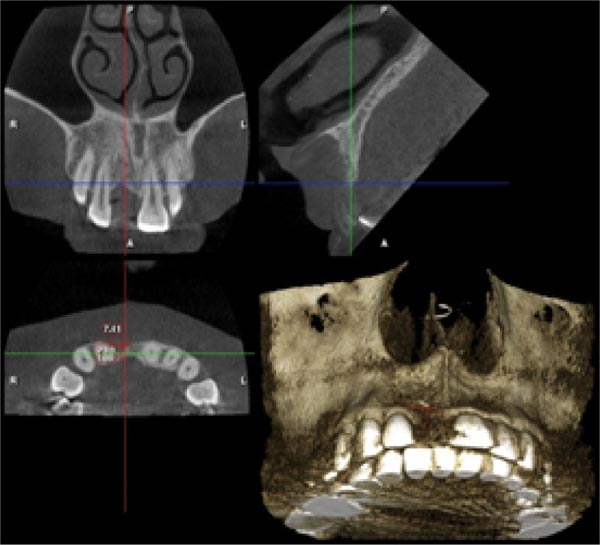
This is a clinical case of a healthy woman with a missing upper right central incisor (#8) who requested a permanent prosthetic replacement due to endodontic failure. Clinically, she was presented with thin edentulous ridges and fibrous gingival tissue and minimal or compromised alveolar bone segment on the buccal profile as detected on cone-beam computed tomography (CBCT).
Case Report:
The conventional treatment approach is to add pink porcelain; however, rarely does the prosthetic gingiva substitute blend well with the existing oral profile. Therefore,Guided Bone Regeneration (GBR) was done instead on #8 using the allograft [RegenOss, Neobiotech] and PTFE membrane. Upon examination, membrane exposure was detected, and the size was found to be increased in follow-up visits. The membrane was replaced with a Concentrated Growth Factor [CGF] and sutured at the site of the defect. After 12 months, a vertical and horizontal bone with adequate soft tissue emergence profile was achieved clinically, radiographically, and digitally. The delayed removal of the exposed membrane provided more time for initial bone regeneration in GBR. The replacement barrier of an exposed membrane using CGF is considered an innovative procedure with the cellular content providing vascularization and regeneration.
Conclusion:
This case concludes that CGF can be a viable alternative material to enhance GBR outcome in replacing exposed membranes.
1. INTRODUCTION
There are numerous challenges in rehabilitating anterior dentition, particularly in cases with deficiency of the buccal plate, thin gingival biotype, and loss of significant alveolar bone volume. In addition, there are also various augmentation procedures to rehabilitate the deficient alveolar ridge. However, bone deficiencies remain a challenge, with the most utilised procedure Guiding Bone Regeneration (GBR). A successful GBR therapy is achieved by ensuring adequate angiogenesis, space maintenance, primary closure, and wound stability performed at the surgical site [1]. The main component in GBR therapy includes placing a non-resorbable or resorbablebarrier membrane to exclude migration of undesired cells into the wound area [2].
The desired properties of the membrane have been postulated, which include biocompatibility, minimal host tissue reaction, optimum clinical handling, cell occlusiveness, space development agent, and aiding in the bone regeneration process [3]. However, the risk of membrane exposure after the initial surgery remains present. Membrane exposure after GBR has a negative effect on the desired outcome with less bone gain on the edentulous ridge [1]. The management of the exposed membrane is mainly reported in case reports and series, which include conservative management and connective tissue grafting, which can be time-consuming, leading to site morbidity and technique sensitivity [4-6].
Concentrated Growth Factor (CGF) is an autologous platelet concentrate initially developed by Sacco et al. with a higher density and reservoir for growth factor in the fibrin matrix due to alternate speed during centrifugation. The growth factors include Transforming Growth Factor b1 and (b2 TGF-B1 and TGF-b2), Vascular Endothelial Growth Factor (VEGF), Fibroblast Growth Factor (FGF), and others. Thus, the utilization of CGF has been an on-going development in dentistry with the ideal application focusing on various surgical and periodontal therapies. Nevertheless, CGF can produced an autologous membrane that is thicker, denser, and more durable than the conventional PRF, which makes it better in terms of clinical handling and management to the clinician [7, 8]. Therefore, the aim of this case report is to describe the utilization of CGF clinically for a membrane exposure incident in guided bone and tissue regeneration.
2. CASE REPORT
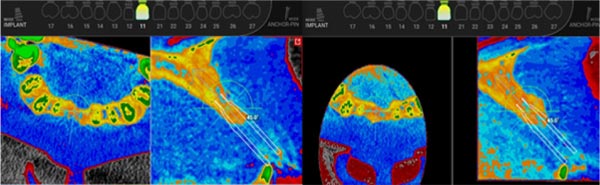
A healthy 45-year-old woman was referred to the Prosthodontic Specialist Clinic, Universiti Sains Islam Malaysia (USIM), for the treatment of a missing upper right central incisor [#8]. The patient did not have any relevant medical and dental history. She also visited the dentist every 6 months. The tooth was extracted due to a history of endodontic failure. Clinically, she was presented with thin edentulous ridges and fibrous gingival tissue and minimal alveolar bone on the buccal area, detected on cone-beam computed tomography (CBCT) (Fig. 1). Her other dentitions were present and sound. The CBCT showed 7.41 mm horizontal and 2.80 mm vertical bony defect (Fig. 1). Diagnostic wax-up showed the possibility of an elongated pontic on #8 due to insufficient volume of soft and hard tissue vertically and horizontally. Commonly, the conventional approach is to add pink porcelain; however, this technique involves additional cost, and the prosthetic gingiva substitute can rarely blend well with the existing oral profile. Therefore, different options were given to the patient, and she agreed to continue with a surgical alveolar bone regeneration followed by the prosthesis and/or dental implant. The patient provided written and oral consent for photography recording, treatment, and data publishing. The surgical procedures and prosthetic management were conducted by an experienced prosthodontist (MSA) under magnification (2.5x).



2.1. Clinical Management
The guided bone regeneration [GBR] procedure was carried out on #8. Local anesthesia of 2% of lignocaine hydrochloride with 1:80000 solutions was administered, and a full mucoperiosteal flap was raised using surgical scalpel blade 15. The flap was extended from mid-buccal of #7 to mid-buccal of #9 facially and palatally. Periosteal and vertical releasing incisions were made on the buccal flap to ensure flap mobility and passivity with the intention of a final primary closure at the surgical site. There was a small amount of alveolar bone, both horizontal and vertically (Fig. 1). Thus, the defect was filled with cortico-cancellous freeze-dried bone allograft [RegenOss™, Neobiotech] followed by the placement of the High-Density d-PTFE membrane (Cytoplast® Ti-250, Deore Materials, Osteohealth, USA) (Fig. 1). The flap was sutured using resorbable vicryl 5-0 followed by some post-operative instructions (Fig. 1). The patient was then prescribed with amoxicillin 500 mg, three capsules per day for the subsequent 5 days, and arcoxia 90 mg for pain management and only to be taken when needed.
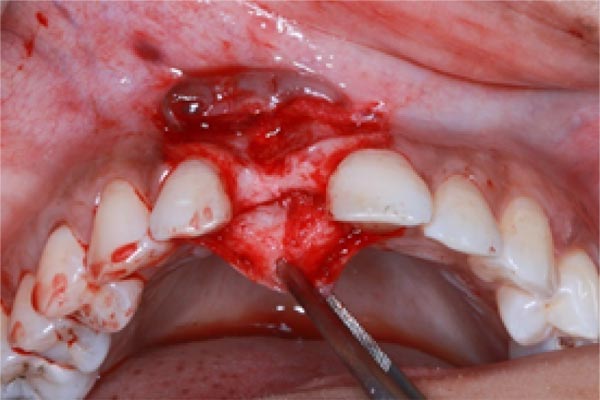
Upon examining it 14 days after the surgery, wound dehiscence with an exposed membrane was detected with a measurement of 4mm x 9mm with loose and dislodged stitches at the surgical site. There was evidence of an epithelial seal on the mesial and distal surgical site with exposure only on the middle area. There was no suppuration or detachment upon probing (Fig. 2). This might be due to careful and conservative management, such as reinforcing the oral hygiene instructions and adequate irrigation with Chlorhexidine Digluconate mouthwash 0.12% (Oradex®, Cavico [M] Sdn. Bhd.).




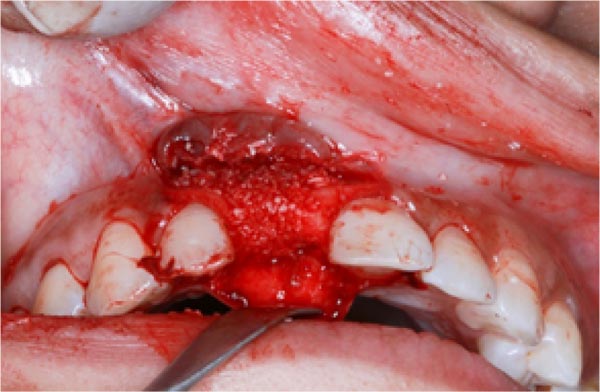
A examination after another 14 days revealed that the wound size increased by 5mm x 10mm. Therefore, to avoid further complications, the membrane was removed and replaced with a Concentrated Growth Factor (CGF) as a barrier. The processing protocol of CGF was followed as per Sacco’s Protocol [7, 8]. The patient’s venous blood of about 10ml was obtained and placed into a Vacuettes® tube without the addition of any anticoagulants. The blood was then centrifuged at an alternating speed using a designated Silfradent centrifuge (Medifuge, Silfradent, Santa Sofia, FC, Italy). The centrifugation protocol occurred as follows; initial acceleration for 30 seconds, 2700rpm for 2 minutes, 2400 rpm for 4 minutes, 2700 rpm for 4 minutes, 3000 rpm for 3 minutes, final deceleration for 36 seconds, and then it stopped [7, 8]. The CGF preparation medium was taken out of the test tubes, and the fibrin buffy coat and the growth factor phases were collected by cutting them off from the rest of the blood with a pair of scissors as per Fig. (2). The CGF sample mediums were pressed into molds to shape them into CGF membranes while removing the liquid element from the preparation. There was a superficial thin mucosal layer of epithelium underneath the membrane. The surgical site was initially deplaqued and irrigated with Chlorhexidine Digluconate mouthwash. The underlying bone graft was visibly clinically healthy without any signs of infection. After the removal of the original membrane, the flap was then slightly raised, and placement was performed, followed by suturing of the CGF at the surgical site using resorbable vicryl 5-0. The site, which was restored with adhesive bridges, showed a satisfactory aesthetic profile immediately after the surgery (Fig. 2). After that, the patient informed the operator [MSA] that she would visit a local dentist for a suture removal appointment due to logistics issues.
2.2. Clinical Outcome
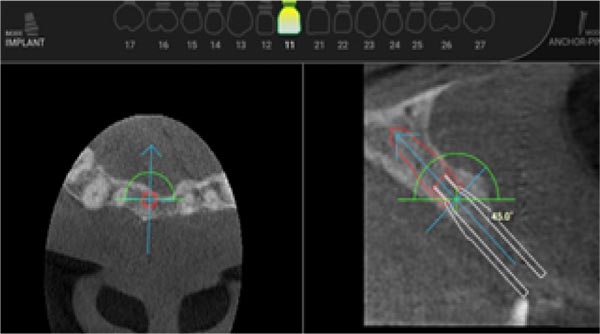
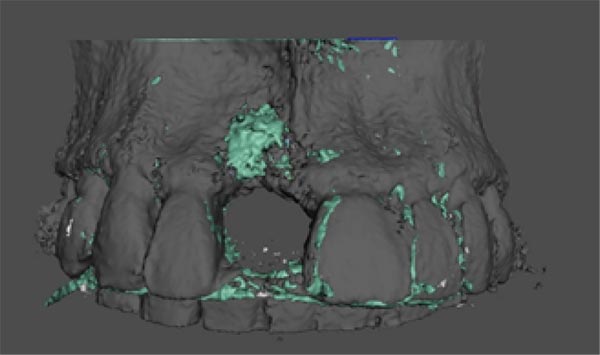
A review on the surgical site after 12 months showed satisfactory maturation of the soft tissue and it was adapting well with the adhesive bridges, which resulted in satisfactory aesthetic and frontal profile. The radiographic analysis showed apparent bone-fill with adequate horizontal bone gain, and it was further analysed using a specialized software for digital implant planning [R2Gate®, Megagen Implant, South Korea]. A digital superimposition with the future implant was planned, and surgical guided implant surgery was also planned for accurate and precise placement of the implant with the potential of simultaneous GBR at the site. A 3-dimensional modelling results revealed the horizontal bone gains buccally and is represented here by the green interface on the generated 3D model (Fig. 3).

3. DISCUSSION
A systematic review and meta-analysis by Lim et al. 2018, discovered that regardless of the type of membrane used, membrane exposure [35%] and soft tissue dehiscence [35%] were the most common post-surgical complications in GBR. The membrane exposure can also occur as early as a week after GBR. The presence of the membrane exposure accompanying the GBR has a negative effect on the desired outcome with a lesser bone gain as compared to the site without membrane exposure on the edentulous ridge [1]. The evidence on exposed membrane management is limited to case reports and series which included initial conservative management such as the utilisation of chlorhexidine mouthwash and topical application, oral hygiene motivation, and weekly follow up in the dentist office, majority of which resulted in a constant increased in the dimension of the exposure. In addition to that, a connective tissue graft on the GBR site is also recommended. Nonetheless, it can be a sensitive technique, with the potential of a donor site morbidity, or it may require another additional surgery [3-5].
In this case report, the decision to use d-PTFE membrane allowed more protection to the grafting site since the structure was more resistant towards bacteria infiltration even if it was left exposed owing to its submicron (<0.3 μm) microporosity unique surface [9]. The delayed approach (28 days) to remove the membrane allowed more time for initial bone regeneration, which enhanced the quality of the bone at the site. Moreover, the delayed removal of the exposed membrane (1-month post-surgery) also provided stability during the healing process in dental implant placement with simultaneous GBR [10-15].
The primary cause of the exposure of the membrane, in this case, was probably due to the loading of the surgical site with a prosthesis [partial denture]. However, thorough examination and adjustments were made to ensure no impingement on its surface during the surgery visit. The original plan was to provide the patient with a prosthesis, i.e., resin-bonded bridge, after the initial surgery; however, wound dehiscence occurred, and the exposed membrane increased in size (5mm X 10mm) during the follow-up visits.. This condition created a visible membrane and affected the aesthetic. As a result, it was decided that the exposed membrane was to be removed and replaced with a barrier of Concentrated Growth Factor [CGF]. The decision to remove the exposed membrane, in this case, was in accordance with the guideline on the management of the membrane exposure of more than 3mm without purulent exudate [16].
The autologous platelet preparation such as CGF was effective as a biological agent to enhance osseointegration, surgical periodontal regenerative scaffold, management of intrabony defects, and sinus augmentation [10-13]. In this case report, the decision to use CGF as a biological membrane was the patient’s choice, as she had respectfully declined other options such as connective tissue graft and conventional recall appointment with oral hygiene motivation. As for the author’s interest, this is the first time in the literature that the implementation of CGF was used as a resorbable barrier to replace an exposed membrane on a wound dehiscence case. The usage of CGF is indeed beneficial in providing a more robust and higher tensile strength of biological membrane combined with the presence of a growth factor such as Transforming Growth Factor [TGF], Vascular Endothelial Growth Factor [VEGF], and progenitor cells and stem cells such as CD34+ [7, 8]. Empirically, this will promote angiogenesis, neovascularity, and cell proliferation at the surgical site [17, 18]. In the results, there was the presence of matured keratinized mucosa with the evidence of an increased soft tissue volume, indicating that soft tissue regeneration had occurred at the previous surgical site. This had been shown by Temmerman et al. that the autologous platelet preparation had the potential to be used as membrane in increasing the width of the keratinized mucosa surrounding the implants [19]. The utilization of the CGF can be beneficial to enhance the outcome of an exposed membrane incident with almost non-existent biological cost as it can be easily manufactured by utilizing a safe technique with acceptable results.
The present clinical report contains a few shortcomings. Fig. (3) on the virtual implant planning shows a potential for future bone augmentation and a mucogingival surgery may be needed for future implant placement. This case report is merely proof of a principle report, and the results should be interpreted cautiously. Further elaborative research works must be conducted to draw definitive conclusions. This case showed an acceptable outcome for the utilization of CGF in a membrane exposure incident. Nevertheless, the findings should be supported by retrospective and prospective case series followed by well-designed clinical trials to comprehend the utilization of CGF in periodontal regeneration, particularly in membrane exposure incidents.
CONCLUSION
In conclusion, this reported case showed an acceptable outcome for the utilization of CGF in membrane exposure incidents, demonstrating a potential use for bone augmentation and mucogingival surgery for implant placement.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
STANDARDS FOR REPORTING
CARE guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


