All published articles of this journal are available on ScienceDirect.
Splinting of the Anterior Maxillary Teeth Using Glass-Ceramic Materials: A Case Report
Abstract
Objective:
The aim of this study was to present the technique of splinting anterior maxillary teeth using heat-pressed glass-ceramic material in a clinical case with long-term follow-up.
Clinical Considerations:
Various materials, including fiber-reinforced tapes, glass fibers, composite resin, and partial coverage metal frameworks, have been used as splinting materials with encouraging clinical results.
Conclusion:
As shown in the presented case, glass-ceramic heat-pressing materials can be used successfully for the splinting of anterior teeth.
1. INTRODUCTION
In cases of advanced periodontal disease, the destruction of the attachment apparatus may reach a level that some teeth may exhibit pronounced mobility or even signs of progressive mobility due to reduced periodontal tissue support. In such cases, there is an obvious need for splinting of the teeth, and additional prosthetic treatment may be necessary [1]. It has been demonstrated that teeth with severely reduced periodontal support and progressive mobility can serve as reliable abutment teeth for extensive fixed splints/bridges after establishing periodontal health and can be maintained in the remaining dentition. In these cases, the Fixed Dental Prostheses should be fabricated properly to preclude undue stress concentrations on the supporting dental apparatus [2].
Rehabilitation of the mastication ability in patients with reduced periodontal tissue support is multiple challenges in dentistry. It has been shown that tooth mobility is reduced by splinting of the teeth showing mobility. One of the primary reasons for splinting and stabilizing teeth is to connect them as an adjunct to periodontal therapy. Several techniques have been reported for the provisional or final stabilization of teeth with mobility. In every selected treatment option, the basic prerequisites of marginal fit, psychologic contour, the possibility of maintaining oral hygiene, and occlusion without trauma must be met. Although the restorations must be planned to withstand the functional requirements of occlusion and mastication, when the restoration is in the anterior zone, there is an additional need to achieve an acceptable esthetic result, also ensuring proper phonetics [3].
Various materials have been used for the splinting of periodontal teeth. Fiber-reinforced composite, composite resin, and metal-reinforced composite are often used as splinting materials for periodontally compromised teeth [4].
Fixed restorations have been used for several years for splinting of teeth with most effective results and long-term follow-up [5]. On the other side, fixed restorations demand extensive tooth preparation and high technical cost. Resin-retained restorations made with minimal tooth preparation have been in clinical use even for a long time, while their failure rarely resulted in adverse consequences for the patient [6]. Fiber-reinforced splinting has also shown encouraging clinical results with long time follow-up [7]. Nowadays, the ever-increasing patient demand for esthetics, minimal preparation, and cost efficiency has resulted in the evolution of techniques and materials that allow predictable restoration of teeth that would otherwise be compromised, especially in an era that ceramic materials may offer innovative solutions.
Interest in dental ceramics is widely known, and their physical properties along with their bonding agents, have significantly improved lately. However, dental ceramics show particularities as for their specialized characteristics and that is the main reason why porcelains and glass-ceramics are the most frequently chosen among them [8]. In general, dental ceramics are divided into two main categories: oxide and glass [9]. Oxide ceramics consist of no more than 15% of silica with little or not at all vitreous phase and are so-called “high strength ceramics” [9]. However, their surface cannot be etched with hydrofluoric acid [10] in contrast with glass-ceramics (the most usually used are feldspathic, leucite-reinforced, fluormica glass, and the mainly chosen nowadays lithium disilicate) [9]. Although these ceramic systems present lower mechanical strength than the oxide ones, their fracture resistance is shown to increase after the cementation with resin cement [9]. Another reason for their wide application in contemporary Prosthodontics is their high esthetic performance, their hardness being similar to natural tooth substance, and their structure being resistant to masticatory forces, dissipating them on the entire prosthesis [11].
Lithium disilicate is the most widely used glass-ceramic used as a reinforcing substance in ceramic materials. The IPS e-max lithium disilicate, (Ivoclar Co) in particular, is composed of quartz, lithium dioxide, phosphor oxide, alumina, potassium oxide, and other components [12]. Thanks to this composition, this glass-ceramic material presents a thermal-and-shock resistance due to the low thermal expansion that occurs during processing [12]. Restorations can be fabricated from this type of ceramic system either by lost-wax heat-pressing techniques or CAD/CAM milling procedures [12]. Nowadays, the introduced lithium disilicate (IPS e-max Press/IPS e.max CAD, Ivoclar Co) offers the strength and the esthetics necessary to meet the highest demands and enables truly multifunctional use [13, 14].
Heat-pressed lithium disilicate has been indicated for several clinical cases including inlays, onlays, thin or full-thickness veneers, partial crowns, anterior and posterior crowns, 3-unit anterior bridges, 3-unit premolar bridges, primary telescope crowns, and implant superstructures [12]. In cases where minimally invasive tooth preparation is desired, for instance, in thin veneers, IPS e-max lithium disilicate makes it possible to fabricate heat-pressed restorations as thin as 0.3 mm while still ensuring the strength of 400 MPa [12, 15]. Its mechanical properties may also provide the option of even no preparation when there is sufficient occlusal space available or in cases of severely worn dentition when preservation of tooth substance is of utmost importance [16].
When it comes to posterior regions fabricating a full contour crown using CAD systems out of lithium, disilicate can offer 360 MPa of strength through the entire restoration [12]. As a result, thanks to these recent advances in mechanical properties, restorations demonstrate a “monolithic” strength unlike any other metal-free restoration [16, 17].
All innovative solutions offered by this ceramic system are widening the restorative treatment options; due to the excellent optical properties, the high mechanical resistance, the variability in clinical indications, and the different manufacturing techniques, it is no doubt one of the most promising dental materials in the realm of Digital Dentistry [18].
This material can be bonded to residual enamel and dentin after etching of the inner ceramic surface with hydrofluoric acid (HF) and silanization, using the latest-generation dual-curing resin cement. Being able to create an adhesive link between the ceramic restoration and the dental substrate allows the clinician to perform more conservative tooth preparations. A feather-edge or knife-edge preparation makes it possible to minimize the needed preparation, thus maintaining more enamel layer intact, and for this reason are recommended for disilicate lithium restorations [19].
2. AIM
The aim of this study was to present the technique of splinting of anterior maxillary teeth using heat-pressed glass-ceramic material in a clinical case with long-term follow-up.
3. CASE REPORT
3.1. Initial Examination and Treatment Plan
A 38-year-old Caucasian woman was referred by her periodontist to a private practice limited to prosthodontics. The patient’s chief complaint was the esthetics of the anterior maxillary area and she also expressed discomfort in normal mastication and speaking. The patient was diagnosed with aggressive periodontitis 4 years ago. She has been treated since then by a periodontist that was re-evaluating the clinical condition at 3-months recalls
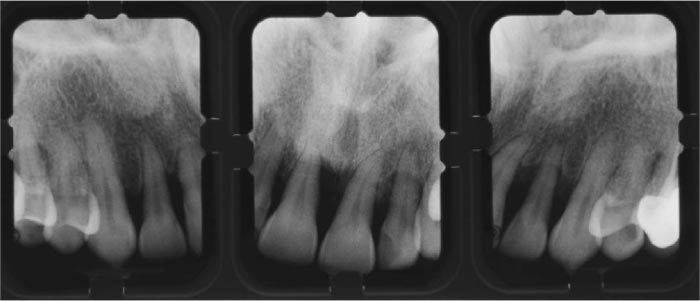
The anterior maxillary teeth showed severe bone loss, as depicted in the initial intraoral radiographs (Fig. 1). The central and lateral incisors had minimum bone support and this explains the severe mobility (II+) and shifting of the teeth. (Figs. 2 & 3). For the initial stabilization of the teeth, the previous dentist had provided the patient with a thin (1mm) omnivac heat-vacuum-formed sheet. The patient was instructed to use the appliance constantly and remove it only during meals. This caused significant functional difficulties and resulted in a feeling of pressure on the anterior teeth if the patient neglected to wear it for an hour. This finding was indicating the shifting of the teeth that could occur even in such a short period of time. One more aggravating factor was the smoking habit of the patient resulting in intensive staining (Fig. 4).



The initial treatment plan proposed to the patient was the extraction of maxillary incisors #12,11,21,22 and placement of two implants in the sockets of the laterals for a fixed 4 unit restoration supported on implants. The second proposed treatment plan was a fixed all-ceramic 6-unit restoration supported on the canines. Although the severity of the case and the age of the patient indicated a treatment plan with a long-term prognosis, the patient denied the extractions and asked for a treatment plan, including the maintenance of the existing teeth. Therefore a more conservative treatment plan was proposed that demanded the splinting of the anterior teeth. A factor complicating further the clinical procedure was the diastemas between the teeth and the high esthetic demands of the patient. Partial coverage splinting with metal reinforcement would definitely compromise the esthetic appearance and would lead to an unacceptable result.
Taking into consideration the patient’s demands and the abovementioned limitations, lithium disilicate was selected as the restorative material for splinting. Glass-ceramic materials have not been reported so far for this indication but the precision of fit and the translucency of the material advocated for its use. The splint would be fabricated by heat-pressing, offering a good fit, and the adhesive bonding on the palatal surfaces of the teeth after cementation would ensure the needed strength. The final result could be very stable, addressing the mobility of the teeth by splinting, while an esthetic solution for closing the diastemas could also be achieved. The use of veneers on the labial surface of the central incisors could further enhance the esthetic result.
The patient was informed that this could be a short term conservative treatment plan until she would consent to a definite restoration.
3.2. Clinical and Laboratory Steps
The palatal surfaces of all anterior maxillary teeth (#13-23) were minimally prepared in order to remove any undercuts that might jeopardize the fit of the final restoration. 1mm space was also needed as the minimum thickness of the glass-ceramic material. Therefore, in areas where the occlusal space between the maxillary and mandibular anterior teeth was less than 1 mm, additional preparation was performed on the maxillary palatal surfaces.
The final impression was taken with an additional type of polyvinyl-siloxane material, and the working casts were fabricated. The undercuts were blocked with orthodontic wax to avoid extreme stress on the teeth with mobility upon removal of the impression.

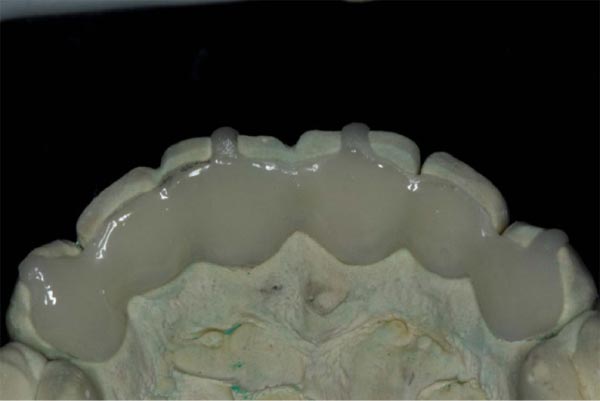
On the working cast, the wax pattern of the restoration was modeled and the restoration was fabricated in one piece by the heat-press technique using IPS Empress material (Ivoclar Co, Liechtenstein), available at that time (Figs. 5 & 6). The restoration was checked intraorally for the marginal fit. To achieve a stable position of the palatal splint during try-in and cementation, ceramic “hooks” were formed on the wax pattern and reproduced in the glass-ceramic. These “hooks” facilitated handling and ensured a stable position during cementation. They were removed after polymerization of the cement. The palatal splint was stained according to the selected tooth shade and finally polished (Fig. 7). The restoration was etched in the internal surfaces using hydrofluoric acid in gel form (Ceramic etching gel, Ivoclar Co) (Fig. 8) and was cemented (Figs. 8 & 9) using dual-curing resin cement (Vario-Link, Vivadent Co, Liechtenstein). The occlusal contacts were checked in maximal intercuspation, protrusion and laterotrusion (Figs. 10 & 11).



After the final cementation of the palatal splint, the central incisors were prepared following the minimal invasion technique. Two ceramic veneers were fabricated using glass-ceramic (IPS Empress, Ivoclar Co) in the staining technique and were cemented following the same laboratory and clinical procedure (Figs. 12-14). Four veneers were proposed to the patient, but she decided only for the central incisors for economic reasons. A night guard was given to the patient for night use to avoid uncontrolled forces caused by eventual bruxism.


The final outcome satisfied the patient both from the functional and esthetic point of view. She was also pleased that she could maintain her existing natural teeth without feeling the functional difficulties that she had prior to treatment. The patient continued the 3-months recall program, and the clinical situation was stable after 7 years. During this period, no detachment was noticed. (Figs. 15 & 16). There was a need for root canal treatment of teeth #21, 22 that were performed through the disilicate lithium restoration and the access holes were covered by composite fillings.





4. DISCUSSION
The clinical management of mobile teeth can be a perplexing problem, especially if the underlying causes of mobility have not been properly diagnosed. In some cases, the clinician is asked to maintain mobile teeth as certain patients reject multidisciplinary treatment that might otherwise include extractions. The splinting of teeth with mobility has been an established treatment option for decades and can help patients maintain their natural teeth for several years [2, 7]. The basic functions of the splinting are to comfort the patient from the consequences of the tooth mobility, ensure function, distribute the occlusal forces on the periodontally compromised teeth and finally contribute to their clinical survival [4, 20]. After successful periodontal treatment followed by a proper recall program, the splinting of teeth is an essential step for their maintenance in clinical function [21].
All ceramic materials have been used successfully for various indications in Fixed Prosthodontics for nearly 30 years. They have also shown excellent results in the fabrications of partial coverage Fixed Dental Prostheses, especially in anterior teeth [22, 23]. Based on the abovementioned advantages of all-ceramic materials, it was decided to fabricate the palatal splint of anterior maxillary teeth from heat-press glass-ceramic in order to combine the esthetic performance, the minimal preparation, and the strength from the adhesive cementation. Zirconium oxide has been used extensively for the fabrication of partial coverage Fixed Dental Prostheses. It offers increased strength but cannot be etched and its opacity may result in an esthetic compromise in anterior teeth with increased translucency.
CONCLUSION
In the presented case, in order to fulfill the patients’ expectations, a conservative treatment plan was needed to avoid extractions and implant, at least as an intermediate stage. Full coverage splinted crowns could have been an option, but extensive tooth preparation would be unavoidable. On the other side, partial coverage metal-reinforced restorations, fixed on the palatal or lingual surfaces (Maryland type), have offered significant help in the maintenance of anterior teeth [3, 6]. An important inhibiting factor in the use of the metal framework in the presented case were the diastemas of the teeth and the increased translucency. Had a metal framework been used, it would probably lead to an unacceptable esthetic result.
Nowadays, the fabrication of a partial coverage palatal splinting from heat-press materials can be facilitated from intraoral scanning so that the stress applied on the mobile teeth during the impression procedure can be avoided. Additionally, the current CAD/CAM technique through a complete digital workflow would minimize problems of accuracy that might be caused by heat-pressing.
As the point of attention for the reported treatment option, the need for extreme accuracy -both in the clinical and laboratory stages- must be underlined. Even small discrepancies in the marginal fit may jeopardize the longevity of the restoration and of supporting teeth. On the other side, if a decementation might occur, it can be repaired intraorally without the need for extensive treatment. For the fabrication of the all-ceramic splint, a minimum thickness of 1mm is needed, and this is a limitation for patients with a deep overbite of lingual inclination of the anterior maxillary teeth.
Further in-vitro studies and controlled clinical trials are needed to confirm the efficacy of the presented treatment option and propose it for extended clinical use.
CLINICAL SIGNIFICANCE
The splinting of periodontally compromised anterior maxillary teeth is essential for their maintenance in clinical function. The use of glass-ceramic materials for the fabrication of fixed splints can offer adequate strength through adhesive bonding, the accuracy of fit, and a good esthetic result for the patient.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial, or otherwise.
ACKNOWLEDGEMENTS
Declared none.


