All published articles of this journal are available on ScienceDirect.
COVID-19 is a New Challenge for Dental Practitioners: Advice on Patients’ Management from Prevention of Cross Infections to Telemedicine
Abstract
Background:
The COVID-19, originated in China in December 2019, has spread worldwide pandemically. Infection control measures are especially needed for healthcare professionals who meet potentially infected patients.
Objective:
The authors aimed to provide general knowledge about COVID-19 disease and indications for the management of emergency dental procedures based on recent literature and experience gained.
Methods:
A literature search was performed to identify scientific information on COVID-19 and prevention of cross infection appropriate for the practice of dentistry.
Results:
The authors provided relevant information about SARS-CoV-2 virus, COVID-19 disease, and prevention of cross infections in the dental office. Furthermore, the authors described their experience and highlighted the potential of telemedicine.
Conclusion:
This article, based on relevant researches, guidelines and Authors’ experience in a COVID-19 Hospital, introduces essential knowledge about COVID-19 and transmission routes and provides recommended management protocols for dental practitioners.
1. INTRODUCTION
On 11th March 2020, the World Health Organization (WHO) declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or Coronavirus Disease 2019 (COVID-19) as a pandemic. At the time this article was written 4103152 infections and 282727 deaths were reported all over the world. The United States is the most affected country with 1329799 infections and 79528 deaths (https://coronavirus.jhu .edu/map.html). In Europe, 1359380 infections and 124525 deaths were confirmed: Spain and Italy have the largest diffusion with 223578 infections and 26478 deaths, and 218268 infections and 30395 deaths, respectively. The ongoing COVID-19 pandemic was first confirmed to have spread on 31 January 2020, both in Spain and Italy [1].
The past experiences with other SARS-CoV outbreak suggest possible modes of transmission including respiratory droplets, contact, fomites, and the fecal-oral route [2-4]. Transmission within healthcare workers has been documented and the risk of cross infection may be higher between dental practitioners and patients due to the characteristics of dental setting [2]. This data was underlying in a document published on March 15, 2020 in New York Times, which showed that dentist, dental assistant, oral and maxillofacial surgeon and dental hygienist are the health care workers with the highest infection risk (exposure percentage between 95 - 100%) [5].
| DENTAL DEVICESPRODUCING AIRBORNE CONTAMINATION | |
|---|---|
| Ultrasonic and Sonic Scalers | Greatest source of aerosolcontamination High risk of dissemination |
| Air Polishing | Moderate to high source of aerosolcontamination |
| Turbine Handpiece | Moderate to high airborne contamination* |
| Low speed handpiece | Minimal to moderate airborne contamination* |
| Ultrasonic and Sonic Surgery devices | Moderate to high airborne contamination |
| Laser (CO2; diode; Er:YAG; Nd:YAG) | Minimal airborne contamination (plume from the infected tissue) |
Therefore, a major strain on infection prevention and control measures is needed in dental practice.
The aim of this study focused on the essential disease outbreak response measures to COVID-19 in dental settings. Due to the increasing number of cases worldwide, the authors provide some management protocols for dentists and dental professionals in the affected areas.
1.1. SARS-CoV-2
The SARS-CoV-2 belongs to the Coronaviridaes’ family that is characterized by a large, single, plus-stranded RNA as their genome (26-32 kb) [6, 7]. Only α- CoV and β-CoV genera can usually infect humans and vertebrates, causing respiratory and gastrointestinal problems and damage to the central nervous system [6]. Specifically, the β-CoV genus includes Middle East respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV [8, 9], both already known for the severe respiratory diseases determined in 2003 and 2012, respectively [10, 11].
For coronavirus, the entry in the host cells is a complex mechanism determined by the trans-membrane spike glycoprotein and the angiotensin-converting enzyme 2 (ACE2) as a receptor [12, 13]. After the entry, SARS-CoV-2 releases the viral genome to the cytoplasm, promoting virus replication mechanism [12].
Several research groups suggested that SARS-CoV-2 began to spread in China from the Rhinolophus affinis bat, in fact several similarities were found between coronavirus (BatCoV RaTG13) and this bat species (96.2%) [14].
Considering the epidemic or pandemic effect of SARS-CoV-2, the main role is played by the “basic reproduction number”, R0, defined as the expected number of secondary cases produced by a single infection in a completely susceptible population [15]. To date, the COVID-19 R0 is estimated between 2 and 3.5, infecting already more people than SARS-CoV in 2003 and MERS-CoV in 2012 [16-19]. Indeed, although COVID-19 has yet a lower case fatality rate (around 2% and 3%) than the 35% of MERS-CoV, it was estimated that SARS-CoV-2 will cause many more deaths than its predecessors due to a higher number of infected persons [18].
1.2. Transmission Routes
The SARS-CoV-2 can be transmitted from person to person mainly by droplets or saliva [20, 21]. Indeed, all procedures that may airborne the COVID-19 through aerosol should be indicated as potential transmission routes.
The main source of transmission is certainly the symptomatic COVID-19, but asymptomatic patients and patients in their incubation period are also carriers [22-24]. The incubation period of COVID-19 has been reported to be 1 to 14 days (5 to 6 days on average) [25]. This time lapse has been used as the quarantine period of potentially exposed persons. However, to date, it is prudent to consider the possibility of incubation period up to 14 days [24, 25].
It is obvious that dental procedures have a conjuncture of unfavorable situations: dental treatments involve close communication with the patients, exposure to body fluids, use of tools generating aerosol and airborne spread of saliva.
1.3. Infection Control in the Dental Office
Generally, the dental office adopts a lot of protective measures in daily work because of the habit of dental professionals to be exposed to many pathogenic microorganisms (i.e. HIV, HCV, etc.). Some of these measures are not effective in preventing the spread of COVID-19, especially for patients who are in the incubation period or unaware that they are infected [26].
In this scenario and without proper protections, this pathogenic microorganism can be easily transmitted through inhalation or contact of conjunctival, nasal, or oral mucosa with droplets and aerosols [27].
The other peculiarity of the dental practice is the short distance of work-routine between the infected patient and the practitioner. Dental patients who cough, sneeze, or simply breath can easily propel the pathogens into the surrounding area. In addition, many dental devices use high-speed gas to drive the turbine to rotate at high speed and work with running water. This condition usually generates a large amount of aerosol and droplets containing saliva or blood.
Many tools by the action of the rotary instrument, ultrasonic vibrations or the combined action of water sprays and compressed air produce the most visible aerosols (Table 1).
Finally, after a dental procedure the operator usually removes a protective barrier, such as a face mask, to talk to the patient. As the aerosol may remain in the air for up to 30 minutes, the potential contact with contaminated material remains and could occur. Human coronaviruses can persist on surfaces like metal, glass, or plastic and remain infectious for 2 hours up to 9 days [28, 29]. A higher temperature such as 30°C or 40°C and ethanol at concentrations between 62% and 71% seems to reduce coronavirus infectivity. Hydrogen peroxide is effective with a concentration of 0.5% and an incubation time of 1 minute while 0.02% chlorhexidine digluconate is ineffective [29].
The Italian experience of the last few weeks could be useful for colleagues who are preparing to face the COVID-19 emergency.
In March 2020, the Italian Ministry of Health ordered the suspension of all non-urgent outpatient activities (including dentistry) in hospitals and clinics of the public health system, until further notification according to the situation of the pandemic [30]. All Italian professional dental associations equally recommended the suspension of non-urgent activities in private dental offices [31]. The Italian dental scientific societies have drawn up guidelines in order to reduce the risk of SARS-Cov-2 transmission [32]. To date, there is a consensus in providing only emergency dental services (Fig. 1), but the situation is constantly evolving, therefore, the guidelines could be updated frequently.
2. MANAGEMENT OF PATIENTS
The goal is to identify the potentially infected patient before leaving home or before entering the operating areas of the dental office. In general, a potentially infected patient is not accepted in the dental office and must be quarantined after notifying the infection control department. It is fundamental to contact the patient by phone and ask a few questions about his/her state of health, especially if he/she has a fever (>37.5°C), cold, cough, breathing difficulties, muscle pain, headache, which has arisen in the last 14 days. In addition, it is necessary to ask the patient if he/she has visited areas at risk, or if he/she has been in contact with infected people or people coming from an infectious outbreak, or with people who had symptoms, in the last 14 days. If the patient presents one of the above symptoms, it would be wise to suggest a drug therapy to the patient by telephone, considering his/her medical history. If the patient's condition requires intervention at the dental office, body temperature should be measured on arrival, preferably with a thermometer without direct contact. A questionnaire must be submitted, with the same questions asked by telephone, in order to identify any risks (Table 2).
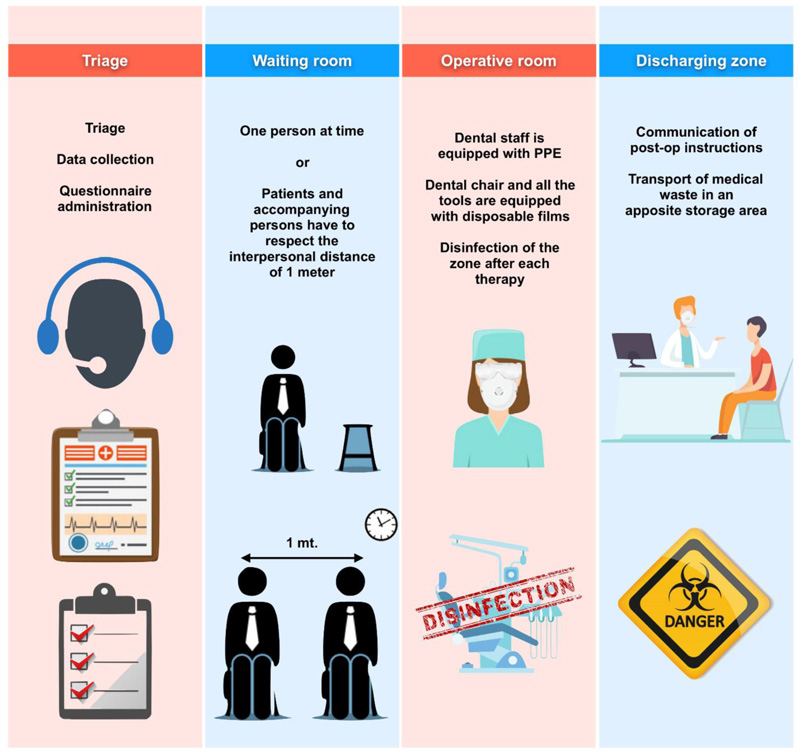
If the patient answers “no” to all questions and has no fever and/or respiratory symptoms, he/she can be treated by observing specific precautions (Fig. 2). Patients who fulfilled only one of the criteria for suspected COVID-19 infection should be considered as potentially infected.
3. PREVENTION OF CROSS INFECTION IN NON-CLINICAL AREAS
It is necessary to provide secretarial staff with personal protective equipment PPE; ( Table 3). Staff, patients and accompanying persons must respect the interpersonal distance of one meter (1m) in these areas. Patient numbers and accompanying people should be dramatically reduced. They should wait for patients outside the dental office. Children and non-autonomous patients should be accompanied only by one person. Promiscuous material from the waiting room (books, magazines, newspapers, toys) should be removed, covering chairs with disposable towels. Disinfectant dispenser should be places and it should be checked whether the patients sanitize their hands. Personal items (clothes, backpacks, bags) should remain in non-clinical areas. It is possible to bring personal items in the clinical area if they are placed in sealed plastic bags. It is necessary to disinfect handles, devices and surfaces after each contact and to ventilate the rooms frequently.
| SCREENING PATIENT QUESTIONNAIRE COVID-19 | |
|---|---|
| Sex | (Male / Female) |
| Age | (Years) |
| Living address | (City - Country) |
| Travel in the past 6 months | (Yes / No - Where) |
| Self-perceived health status | (Very good, good / Fair / Very bad, bad) |
| Medical consultation in the past 14 days? | (Yes / No) |
| Presence of fever (>37.5°), cold, cough, respiratory symptoms, muscle pain, headache in the last 14 days | (Yes / No) |
| Have you been in contact with people with these symptoms for the past 14 days? | (Yes / No) |
| Have you been in contact with infected people in the past 14 days? | (Yes / No) |

| Hand hygiene | • Alcohol-based hand rubs for the decontamination of hands, e.g. after removing gloves. Two WHO recommended formulations (based on 80% ethanol or 75% 2-propanol) |
|
Personal protective measures - Standard protection |
• Disposable cap • Disposable surgical mask • Disposable white coat • Protective goggles or face shield • Disposable latex or nitrile gloves |
|
Personal protective measures - Secondary protection (Advanced protection) * |
• Disposable doctor cap • Disposable surgical mask • Protective goggles or face shield • Working clothes (white coat) with disposable isolation clothing or surgical clothes outside • Disposable latex gloves |
| Facilities | • Anti-retraction dental handpiece with anti-retractive valves or other anti-reflux characteristics are recommended • Consent and charting are done electronically with touchscreen devices to facilitate decontamination • Monitors, laptop computers, and dental devices surfaces are covered with plastic wrap to decrease the risk of contamination and to facilitate cleaning |
| Disinfection of the clinic settings | • Surface disinfection with 0.1% sodiumhypochlorite or 62-71% ethanol • Public areas andappliances should also be frequently cleaned and disinfected,including door handles, chairs, and desks |
| Management of medical waste | • The medical andcommon waste generated by dental therapies in patients with suspected or confirmed 2019-nCoV infection are regarded asinfectious medical waste. |
| Segregation of staff | • Staff is separated to reduce cross- infection between healthcare facilities • Staff meetings are suspended |
4. PREVENTION OF CROSS INFECTION IN CLINICAL AREA
Only the necessary tools can be placed on the shelves. It is fundamental to protect the dental chair and all the tools with disposable films. Dentist and assistant must sanitize their hands before and after the use of PPE (Table 3). The operators should protect themselves with a filtered mask (N-95 masks, National Institute for Occupational Safety and Health, or FFP2/FFP3-standard masks, European Union) associated with eye and hair protection, face shields, disposable water-repellent white coat.
If possible, it can be useful to leave the windows open (at least partially) during the working session. At the end of the treatment session (which should be as short as possible), the disposable films must be removed with clean gloves, disinfecting all instruments and surfaces with suitable disinfectants (isopropyl alcohol, hydrogen peroxide, e.g.) and disposing properly the disposable material [29, 33]. The room should be ventilated as much as possible.
5. PATIENT EXAMINATION AND TREATMENT
It is recommended to use mouth rinse containing oxidative agents such as 1% hydrogen peroxide or 0.2% povidone considering the susceptibility of coronaviruses [29, 34-36]. The use of disposable instruments is strongly recommended. Aerosol-generating procedures must be minimized and procedures inducing cough like intraoral x-ray and soft palate aspiration should be avoided. The use of the rubber dam is mandatory in order to reduce contamination in all dental emergency procedures (pulpits, apical periodontitis), but it cannot be used in oral surgery procedures [37]. Some precautions described in the amalgam removal protocols may be useful [38].
Despite high-volume saliva ejectors that can minimize aerosol and airborne, it is recommended to use also High-Volume Evacuator (HVE) of large diameter (> 8 mm) that allows removal of high volumes of air in a short time [27, 39].
For restorative dentistry and endodontics procedures, it is advisable to use rotating instruments on contra-angle with low-speed drilling and minimum water irrigation (avoid air-water cooling) or erbium laser if available in the dental office.
In the emergency management of an irreversible pulpitis, it would be advisable to limit the treatment to pulpectomy and dressing, although current techniques allow completing the endodontic treatment in one session in most cases [40].
In case of tooth extraction, minimally invasive procedures are preferred. Surgical technique should limit the use of high-speed drilling, using hemostatic procedures to limit the future access for patients to the hospital. For the same reason, fast absorbable suture is mandatory.
6. TELEMEDICINE: AN OPPORTUNITY TO AVOID RISKS
To observe government decisions, telemedicine (TM) is now largely appreciated to minimize the risk of increased COVID-19 dissemination and cross infections at medical or dental offices [41, 42]. TM is a new concept of healthcare to deliver care across distance using advanced communication technologies (smartphones, tablets and laptops) [43]. TM completely modified the traditional medical approach of working, promoting a virtual method of visits, consultations, and follow-up instead of physical contacts and face-to-face clinical evaluations. Among professionals, this type of digitalization can create a doctor to doctor connection to exchange patients’ data, diagnostic doubts, and therapeutic counselling. Between dental clinicians and patients, this communicative workflow can support questions, remote consultations and follow-up visits, reducing the risk to move to the dental office.
CONCLUSION
COVID-19 has spread worldwide in a pandemic way and infection control measures are mandatory to limit contagion, especially for healthcare professionals who meet potentially infected patients. To date, there is a consensus in providing only emergency dental services, but the situation is constantly evolving. In any case, the reduction of infectious risk remains a challenge for dentists, among the most exposed health professionals.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


