All published articles of this journal are available on ScienceDirect.
Mandibular Behavior after Rapid Maxillary Expansion: A Clinical Study
Abstract
Background:
Rapid Maxillary Expansion (RME) is a primary part of the contemporary orthodontic treatment plans. In addition to the maxilla, it is important to know its effect on the other dentofacial components. Some studies showed dentofacial changes after RME in the sagittal and vertical planes. The clinical importance of these changes is controversial.
Objective:
To investigate the mandibular changes after RME as the only treatment intervention in the sagittal and vertical planes.
Methods:
Twenty-eight growing patients aged 4-14 years were included in the current study. The bonded acrylic splint expander was used. Lateral cephalometric radiographs were taken at the beginning of the treatment (T1) and after a retention phase of six months (T2). The mandibular changes were assessed using vertical parameters (SN.MP, MMA, LAFH/TAFH, S.AR/AR.GO) and sagittal parameters (SNB, S.N.POG, N.A.POG). The changes between T1 and T2 were examined by paired samples T-test.
Results:
Two parameters showed a backward rotation in the vertical plane. The parameter S.AR/AR.GO showed a significant increase. The skeletal convexity increased with no clinical significance.
Conclusion:
There were statistically significant changes in the sagittal and vertical planes with no clinical importance. RME may affect the mandibular condyle position.
1. INTRODUCTION
Rapid Maxillary Expansion (RME) is a routinely used orthopedic treatment for many clinical conditions [1-3]. The earliest published paper was written by E.C. Angell (the father of rapid maxillary expansion) [4]. After the reintroduction of this procedure by Haas, RME has been commonly used in the field of orthodontics [5, 6]. Several appliances have been introduced with new modifications in the expander or the appliance design. The bonded acrylic splint expander, Transverse Sagittal Maxillary Expander (TSME) [7], Ragno expander [8], the memory screw [9, 10], and the differential maxillary expander [11], have new mechanisms of action. Some concerns have been raised regarding the oral hygiene and food control in patients wearing orthodontic appliances [12], especially in patients with restorations [13, 14] or those with incorrect behavior [15]. However, some types of expanders are considered more hygienic than others [16].
Many studies investigated different aspects of the RME procedure. Some studies were histological [17]. Others investigated the relapse [18], stability [19] and the side effects related to RME [20].
Increasing the Vertical Dimension (VD) after the maxillary expansion is a primary consideration in treatment planning [21]. Some authors did not find any statistically significant increase [22]. Others claimed that there was a statistically significant increase without any clinical importance [21]. Lineberger stated that the VD increasing had no prejudicial effects on the vertical skeletal relationships. According to long term studies, it was a transient effect [23].
A maxillary displacement after RME has been reported [24]. Mandibular displacement is more controversial, keeping in mind that the mandible is the dynamic part of the dentofacial structures. Some authors reported an anterior mandibular displacement, which improved class II malocclusion, either through dental casts studies [25] or by cephalometric evaluation [20]. The “foot and shoe” theory and the “spontaneous correction of class II malocclusion” phenomenon were introduced [26]. In fact, these had been pointed in the German literature since the early 1900s by korbitz [26, 27]. However, the mandibular backward rotation induced by the maxillary expansion has been described [28].
Despite the large number of clinical studies that investigated the effects of RME, there is a lack of information regarding patients treated by RME as the only treatment intervention. The aim of this study was to investigate the mandibular sagittal and vertical changes subsequent to rapid maxillary expansion.
2. MATERIALS AND METHODS
The lateral cephalograms used in this study were obtained from a previous thesis and no patient was treated, especially for this article. The sample consisted of twenty-eight patients (16 males and 12 females) with indications for transverse expansion aged 4-14 years [9 ± 1.12], and without needing any mandibular intervention during the activation and retention periods. To determine the sample size, G*Power 3.1 (Heinrich-Heine-Universitat, Dusseldorf, Germany) program was used based on the results of a similar previous study [29]. Including a control group was unfeasible due to ethical reasons. It is unethical not to intervene when a diagnosed transverse discrepancy is present [30].
The inclusion criteria were:
- Maxillary constriction.
- Posterior crossbites.
- Class III face mask therapy [phase one].
- Functional therapy of class II [phase one].
Exclusion criteria were:
- Previous orthodontic treatment.
- Syndromes or congenital disorders.
- Class II division two.
- Asymmetries in another plane.
- Need for mandibular orthodontic intervention.
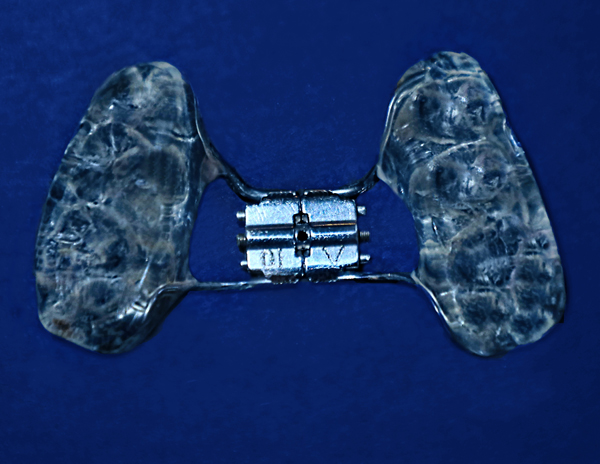
This study was conducted according to the World Medical Association (WMA) guidelines (Fortalenza, Brazil, October 2013). Patient health and safety were the primary considerations [31]. Informed consents were performed. Lateral cephalometric radiographs (Cranex® Excel Ceph, Soredex, Tuusula, Finland) were taken before treatment (T1). The appliance design was similar to McNamara design (bonded rapid maxillary expander with occlusal acrylic coverage), as shown in Fig. (1). Hyrax® expander (Dentaurum, Pforzheim, Germany) was used. The expander was activated one turn per day until the palatal maxillary cusps reach the buccal mandibular cusps. Overcorrection of 2-3 millimeters was gained. The overcorrection was visually estimated. The appliance was left in place during the retention phase. The average retention period ranged from 164 to 192 days (178 ± 7). After the retention phase, lateral cephalograms were taken (T2).
2.1. Cephalometric Analysis
Lateral cephalograms were exported as DICOM (Digital Imaging and Communications in Medicine) files. They were digitized using Facad cephalometric software (Ilexis AB, Sweden) installed on x64-based PC (Hewlett-Packard, Palo Alto, California, USA) running the windows 10 professional edition (Microsoft, Redmond, Wash). Five cephalograms were digitized in every session. Frankfort plane was rotated to be horizontal before landmarks identification. The auto-contrast function was used for almost every point detection. The vertical assessment was based on: SN-MP, MMA, LAFH /TAFH, S.AR/AR.GO. The sagittal assessment was based on: SNB, S.N.POG, N.A.POG. Ten cephalograms were digitized one month later to test the intraoperator reliability. Table 1 shows the definition of the used landmarks.
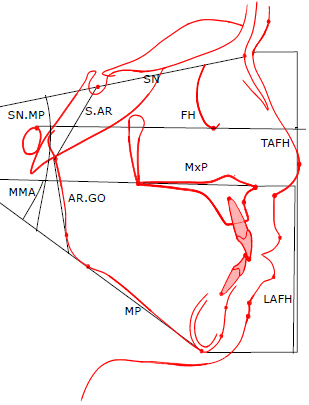
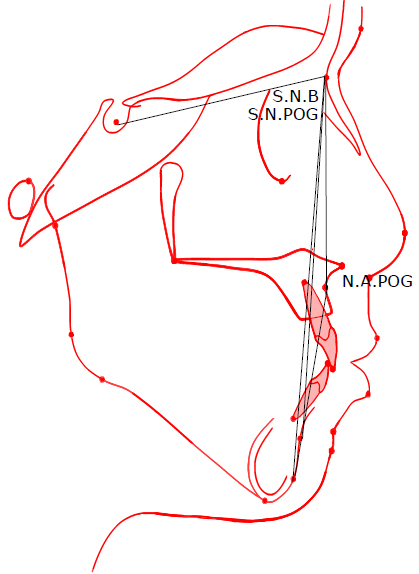
The variables shown in Fig. (2) (The vertical parameters) and Fig. (3) (The sagittal parameters) were defined as follows:
- SN.MP: The angle formed between the anterior cranial base [S.N] and the mandibular plane [line between menton and constructed Gonion].
- MMA: The angle formed between the nasal line [ANS, PNS] and the mandibular plane [ME. GO].
- LAFH: The vertical distance from Menton to the anterior nasal spine.
- TAFH: The vertical distance from Menton to Nasion.
- S.AR/AR.GO: The ratio between the posterior cranial base [representd as a line from S to AR] and the hight of mandibular ramus [a line from AR to constructed gonion]
- SNB angle: Angle formed by points S, N and B
- S.N.Pog angle: Angle formed by points S, N and Pogonion
- N.A.Pog angle: Angle formed by points N, A and pogonion
| Landmarks | Definition |
|---|---|
| Sella (S) | The center of sella turcica |
| Nasion (N) | The most anterior point on the frontonasal suture |
| Menton (ME) | The most inferior point on the symphyseal outline |
| Pogonion (POG) | The most anterior point on the mandibular symphysis |
| Anterior nasal spine (ANS) | Tip of the anterior nasal spine |
| Posterior nasal spine (PNS) | The tip of the posterior nasal spine |
| Orbitale (OR) | The most inferior point on the lower border of the bony orbit |
| Porion (P) | The most superior point on the outline of the external auditory meatus |
| Constructed Gonion (GO) | The intersection of the mandibular plane with a plane through Articulare, Posterior and along the portion of the mandibular ramus inferior to it |
| A point (A) | The deepest point of the curve of the maxilla between the anterior nasal spine and the dental alveolus |
| B point (B) | the deepest point on the bony curvature between the crest of the alveolus and pogonion |
| Articulare (AR) | The point of intersection between the posterior border of the mandibular condyle and the lower border of the cranial base |
2.2. Statistical Analysis:
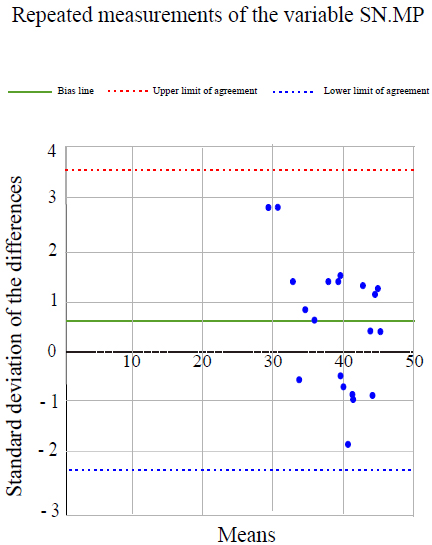
Intraoperator reliability was examined by the correlation coefficient test. In addition, the Bland-Altman method was used. Treatment changes were examined by paired samples t-tests. Statistical significance was tested at P < .05. Table 2 shows descriptive statistics for the measurements before and after treatment, and the results of paired samples t-tests. Microsoft Office / Excel 2016 (Microsoft, Redmond, Wash) was used for statistical analysis.
3. RESULTS
The intraoperator error was limited (average correlation results: r=0.98). As an example, Fig. (4) shows all the repeated measurements of the variable SN. MP is between the upper and lower limit of agreement, which validates the tracing method. The null hypothesis was rejected for three vertical parameters and one sagittal parameter. Descriptive statistics and treatment changes for the cephalometric variables derived before and after orthodontic treatment are shown in Table 2
| - | Pretreatment | Posttreatment | - | ||||||||
| Vertical | unit | MEANS | SD | MIN | MAX | MEANS | SD | MIN | MAX | DF | P VALUE |
| SN-MP | deg | 38.85 | 5.09 | 28.3 | 44.5 | 39.51 | 3.96 | 32.2 | 44.8 | 0.66 | * |
| MMA | deg | 29.79 | 6.33 | 20.8 | 39.2 | 30.69 | 6.28 | 21.1 | 37.8 | 0.9 | ** |
| LAFH/TAFH | % | 55.45 | 1.59 | 52.3 | 58 | 55.58 | 1.77 | 52.1 | 58.2 | 0.13 | NS |
| S.AR/AR.GO | % | 83.46 | 7.90 | 73.8 | 98.3 | 87.23 | 13.49 | 71.7 | 113 | 3.77 | * |
| Sagittal | - | ||||||||||
| SNB | deg | 75.33 | 4.05 | 70.8 | 85 | 75.27 | 3.20 | 71.2 | 81.3 | - 0.06 | NS |
| S.N.POG | deg | 75.69 | 4.18 | 70.7 | 85.8 | 75.63 | 3.26 | 71.9 | 81.9 | - 0.06 | NS |
| N.A.POG | deg | 3.24 | 6.33 | -7.7 | 13.8 | 4.4 | 5.65 | -6.7 | 11.8 | 1.16 | * |
3.1. Vertical Assessment
SN-MP angle increased significantly from T1 to T2 (0.66 degree, p < 0,05), and Maxillomandibular Angle (MMA) increased a mean of 0.9 degree (p < 0,05). These increases had no statistical effect (p > 0,05) on the ratio of lower anterior facial height to the total anterior facial height (LAFH/TAFH). S.AR/AR.GO increased significantly (3.77%, p < 0,05).
4. DISCUSSION
The aim of the present study was to investigate the mandibular changes in the sagittal and vertical planes after RME as the only treatment intervention. RME was performed using the bonded acrylic splint expander.
One of the limitations of this study was the absence of a control group. The maxillary transverse deficiency is not a self-corrected malocclusion. It is not ethical to leave patients with maxillary deficiency without intervention. Pandis also considered the use of historical control groups problematic [32]. Another limitation was the unbalanced population (16 males versus 12 females), caused by the additional criterion used in the present study (the absence of necessity for mandibular intervention). This criterion decreased the number of patients available for the present study. It was challenging to find patients who need only maxillary orthodontic intervention during the first six months of the treatment period. However, the unbalanced population would not affect the biomechanical behavior of the mandible after maxillary expansion because it is not fully controlled by hormones. For the same reason, it was unfeasible to divide the patients into groups according to each type of malocclusion, or to increase the sample size.
Schudy emphasized that increasing the VD may exacerbate the sagittal discrepancy [33]. Almost every orthodontic malrelationship has a vertical, sagittal and transverse component [21]. The present study results showed a mandibular clockwise rotation and a bite opening effect after RME. As MMA increased significantly (p < 0,05), it could be concluded that the clockwise rotation resulted from the dentoalveolar changes rather than the maxillary vertical displacement, which might affect the ratio of LAFH/TAFH. The LAFH/TAFH showed no significant changes after RME (p > 0,05). The dentoalveolar changes could be like a flexion of the alveolar ridges [34], in addition to the tipping and extrusion of the anchor teeth [35, 36]. These changes could be compensated in the next stage if the patient had to go through a fixed appliance phase of treatment. This could be accomplished through the modification of the maxillary posterior teeth torque. However, the present study results were favorable because if the maxillary vertical displacement was responsible for the clockwise rotation, it should be controlled through extraoral appliances (like vertical pull chin cap), as suggested earlier [37]. Furthermore, this could be the reason for controversy between short term and long term clinical studies. The short term studies recorded VD increases after RME [24]. The long term studies suggested that the VD increase was transient and had no long term deleterious effect [23]. The long term study, because of duration, would include a second phase of fixed appliances therapy with many variables to control; like the torque and prescription of posterior teeth brackets. The short term study may include a phase of fixed appliances therapy and may not.
The significant increase in S.AR/AR.GO (p < 0,05) was caused either by S.AR increase or by AR.GO decrease. AR.GO decrease could be a result of condylar repositioning into a more upper or centric position. This may be produced by the elimination of the deviating contacts after expansion. The increase in S.AR could be induced if the expansion affected the spheno-occipital synchondrosis as suggested by some authors [38]. However, the lateral cephalometric radiographs are insufficient to evaluate the RME effect on the mandibular condyle position in its fossa. Further investigations are needed using other methods like Magnetic Resonance Imaging (MRI) and Cone Beam Computed Tomography (CBCT).
There was no mandibular displacement in the sagittal plane. However, there was a clockwise rotation which could camouflage any forward repositioning. The angle of convexity increased a mean of 1.16 degree (p < 0,05), which could be resulted from the mandible clockwise rotation or the advancement of point A. Haas reported a forward displacement of point A after RME [6]. However, this convexity increase (1.16 degrees) in the growing patients could be compensated by the continuous growth of the mandible. Pancherz reported a late skeletal growth after the age of twenty [39].
CONCLUSION
Within the limitation of this study, the results indicate:
- There was a clockwise rotation of the mandible and a bite opening effect after rapid maxillary expansion.
- The skeletal convexity increased after RME.
- Mandibular clockwise rotation and increased skeletal convexity are not contraindications for rapid maxillary expansion.
- RME may affect the condyle position and the posterior cranial base.
LIST OF ABBREVIATIONS
| RME | = Rapid Maxillary Expansion |
| VD | = Vertical Dimension |
| MRI | = Magnetic Resonance Imaging |
| CBCT | = Cone Beam Computed Tomography |
| DICOM | = Digital Imaging and Communications in Medicine |
| WMA | = World Medical Association |
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The Study Was Approved by The Institutional Review Board of Tishreen University, Syrian Arab Republic Under Approval No.1143.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consents were performed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Department of Orthodontics, Faculty of Dentistry, Tishreen University, Lattakia, Syrian Arab Republic [www.tishreen.edu.sy].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors acknowledge Dr. Hasan Ali (MSc. in Pediatric Dentistry) for the aid in study design, and Dr. Majed Amran (MSc. in Endodontics) for the aid in manuscript revision.


