All published articles of this journal are available on ScienceDirect.
Healing without Surgery: A Case of Supernumerary Tooth,
Abstract
Background:
Supernumerary teeth are present in 0,2-3% of the population. Multiple supernumeraries are often associated with syndromes such as cleidocranial dysplasia and Gardner's syndrome. They often hinder the permanent eruption’s teeth, causing cavities, periodontal lesions, pulp necrosis, and in some cases follicular cysts. Reactive lesions such as fibroma, local fibrous hyperplasia, pyogenic granuloma, and peripheral ossifying fibroma are frequent gingival lesions.
Materials and Methods:
We reported a case of a 9 years old patient with the missed eruption of a permanent element caused by a supernumerary tooth, associated with an exophytic palatine lesion. The deciduous incisor was still present and the supernumerary included. It was decided to proceed with the extraction of the deciduous and to wait for scheduling checks every two months. After a few months, the conoid shape supernumerary tooth erupted in the maxillary arch, so a fixed orthodontic therapy was performed to create the space for the central incisor’s eruption.
Results:
After a few months, the tooth began to erupt in the arch thanks to orthodontic traction. The patient was instructed to correct and specific oral hygiene maneuvers to lower the plaque index and try to reduce gingival hypertrophy.
Conclusion:
Supernumerary teeth often hinder the eruption and development of the related permanent tooth causing localized periodontal problems. Corrective fixed orthodontics requires more strict oral hygiene to avoid periodontal complications.
1. INTRODUCTION
The supernumerary teeth are extra teeth compared to the normal number, 20 for deciduous dentition and 32 for permanent dentition. They can be single, double, or multiple, included or erupted in the dental arches [1]. There are supernumerary incisors, mesiodens, canines, premolars, and molars. On the basis of the morphology, there are four different types of supernumerary: conical, tuberculous, supplemental, and odontoma [2]. The upper jaw is the region with the highest incidence of supernumerary and the most frequent morphology is the conoid [3]. The supernumeraries are less common in the primary dentition with respect to final dentition [2].They represent an uncommon human dental anomaly in the case of multiple supernumeraries while the single phenomenon is more frequent [1]. The prevalence in the literature has been reported between 0.2 and 3% and males are more affected than females. The etiology is heterogeneous, highly variable, and in most cases is idiopathic [4]. Multiple supernumeraries are often associated with syndromes or developmental abnormalities such as cleidocranial dysplasia, Gardner's syndrome, tricorinofaringeal syndrome, and lip cleft [1]. Supernumerary teeth often hinder the eruption and development of the related permanent tooth (also called definitive dental element, any of the second set of teeth that follow the primary teeth), causing crowding, diastema, retention or delayed/ectopic eruption, root resorption, caries, periodontal lesions due to compression of adjacent roots, necrosis of the pulp, and in some cases follicular cysts [1, 4]. They cause a delayed eruption or a failure to erupt in 21.6% of cases [1]. The correct localization of supernumerary teeth is very important for diagnosis, treatment, and before any surgical intervention. Traditionally supernumerary teeth have been diagnosed and localized using Two-Dimensional (2D) methods such as panoramic and intraoral radiographs. With the introduction of Cone-Beam Computed Tomography (CBCT) in dental medicine, this Three-Dimensional (3D) imaging technique is now increasingly used for the exact localization of supernumerary teeth and the diagnosis of root resorption of adjacent teeth [5].
The purpose of this article is to present a case of a patient with a supernumerary tooth history and subsequent onset of localized gingival hypertrophy developed with the corresponding permanent tooth arch eruption.
2. CASE PRESENTATION
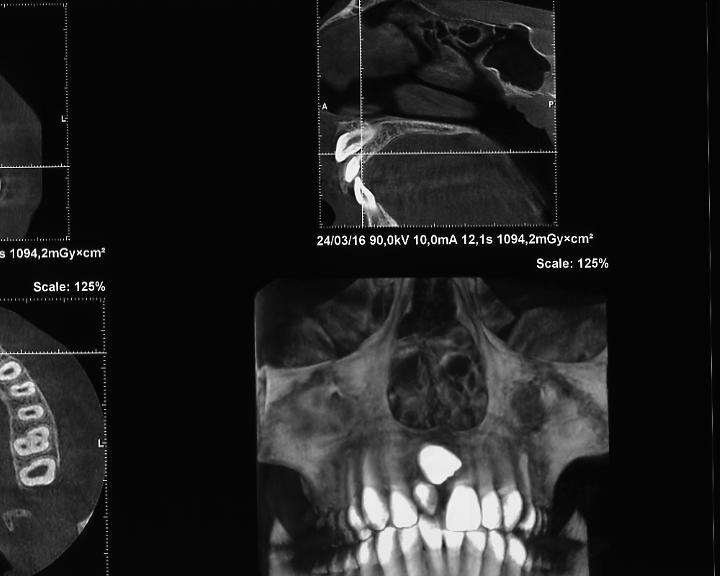
Parents of the patient asked for a visit for their 9 years old son. From initial evaluation, the lack of exchange of the upper central incisor of the first quadrant was evident. A panoramic X-ray was prescribed and performed in a radiological clinic, (Fig. 1) which confirmed the lack of the element 1.1 eruption, due to the presence of an included supernumerary tooth that hindered the commuting of the deciduous incisor. It was decided to proceed with the extraction of the deciduous and to wait for scheduling checks every two months. After a few months, the supernumerary of the conoid shape erupted in the maxillary arch, the permanent was evidently included under the nasal fossa and blocked by the upper labial frenulum and the root of the conoid (Fig. 2). The brackets used have a standard prescription of -7 torque. If there is a lack of space or the palate is tight, the attacks are placed upside down +7 (180 degrees) to prevent exposure of the canine root and subsequent gum recession.
Three years after the OPT, a conical beam computed tomography (Fig. 3) was performed to accurately locate the position of the incisor included in the maxillary bone and evaluate possible lesions to the adjacent teeth. The orthodontist, after the case’s study (impressions, teleradiography, and 8 photos in different projections), planned the treatment with fixed orthodontics to create the space and facilitate the eruption of the central incisor. The supernumerary was extracted.
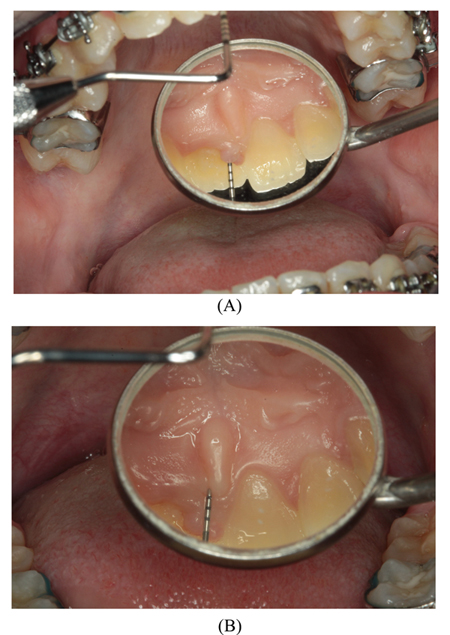
After a few months, the tooth was channelled and began to erupt in the arch through the orthodontic traction. During the orthodontic treatment, specific oral hygiene session (that included motivation to oral hygiene, ultrasonic instrumentation, and final polishing) was performed, and palatal gingival hypertrophy was found near the region of 1.1. (Fig. 4); at the periodontal survey it measured 5.5 mm, showed slight bleeding and the plaque index was 100% (Fig. 5A-5B). At palpation, the tissue involved was compact, of stretched-elastic consistency. The shape of the gingival hypertrophy showed four distinct lobes (Fig. 6). The patient reported discomfort because the increase in gingival volume caused chewing and occlusion. The patient was instructed to use an electric toothbrush to lower the plaque index and try to reduce gingival hypertrophy. The parents provided written informed consent for their son to be involved in the study. We decided to associate treatment with topical probiotics Lactobacillus reuteri DSM 17938 and lactobacillus reuteriATCC PTA 5289, 1 tablet a day for a month. The lesion at follow up healed (Fig 7).


3. DISCUSSION
Reactive lesions are relatively common in the oral cavity due to the frequency with which the mucous membranes undergo trauma. They often also arise due to bacterial plaque, tartar, and the presence of foreign bodies such as prostheses and orthodontic appliances [6]. Most reactive lesions in the oral cavity involve the gingiva. Fibroma, local fibrous hyperplasia, pyogenic granuloma, and peripheral ossifying fibroma are commonly found gingiva lesions [7]. According to a recent review of the literature associated with a retrospective study on reactive hyperplastic lesions of the oral mucosa performed on a total of 155 cases, the most common clinical lesion was found to be the traumatic fibroma (36.5%) and the fibrous hyperplasia (37.4%). Clinically reactive lesions presented as sessile lesions (51%) or peduncle lesions (49%). Lesions were more frequent in females, 99 cases, (63.9%) and less frequent in males, 56 cases, (36.1%) [6]. In another study, Babu et al. [8] found the medium size of the reactive lesions ranged between about 0.5-1cm. The most common sites were the anterior jaw followed by a posterior mandible and finally the tongue. Most lesions showed poor oral hygiene status (87.2%) [8].
It is known that patients subjected to fixed orthodontic treatment have a high susceptibility to plaque accumulation on teeth due to brackets, arches, ligatures, or other orthodontic elements that favor the stagnation of bacterial plaque and make oral hygiene more difficult to make. Orthodontic treatment can significantly increase the health status of periodontal tissues but very often it can be followed by several periodontal complications such as recession and gingival hyperplasia [9, 10]. One of the adverse periodontal changes is a hypertrophic form of gingivitis with pseudo pockets formation. Clinical studies concluded that gingival changes during orthodontic treatment are transient without permanent damage to periodontal support tissues [11].
A cross-sectional study of Flores-Bracho et al. [12] evaluated the possible genotoxic effects in oral mucosa cells in carriers of fixed orthodontic appliances. The study comprised 74 patients in orthodontic treatment and 21 control patients between 11 and 35 years of both sexes. The authors concluded that there is no evidence of genotoxic effects even after long periods of orthodontic corrective treatment [12].
A preventive protocol, based on motivation and instruction on the correct oral hygiene maneuvers before and during orthodontic treatment, decrease the risk of dental caries and periodontal disease in patients with fixed corrective devices This statement was demonstrated through a study that assessed periodontal parameters and levels of microbial species after placement of fixed orthodontic appliances in patients who received oral hygiene instructions and were monitored throughout the duration of treatment.The periodontal index registered initially did not change to the 90-day control, the total amount of the purple and red complexes and the candida species decreased at T2 (60 days from the placement of the orthodontic appliance), the green, yellow, and orange complex showed a significant decrease at T3 (90 days from the placement of the orthodontic appliance).[13]. Specific species analysis showed that Prevotella nigrescens, Pseudomonas putida, Fusobacterium periodonticum, Pseudomonas aeruginosa, Peptostreptococcus anaerobius, and Tannerella forsythia showed a high incidence before binding and their level decreased to T2 and T3. Only Porphyromonas gingivalis showed an increase in levels at T2 and the highest level at T3. The Streptococcus spp. decreased levels from T2 onwards [13, 14]. In light of the above, the early diagnosis of supernumerary teeth is important for an accurate treatment plan. Dental alteration can be related to anatomic deviations [15], genetic deficiency [16], or interaction [17]. The viable alternatives for the treatment of mucosal lesions are conventional surgery [18], laser-assisted surgery [19], or non-surgical treatment [20].



Probiotics, Low-Intensity Laser Therapy (LLLT), Photodynamic (PDT), and ozone therapy favoring the reduction of pocket depth and healing of inflamed tissues are a valuable aid for the control of periodontal indexes in gingival hypertrophy for a more conservative approach than surgery [21-24].
CONCLUSION
Supernumerary teeth often hinder the eruption and development of the related permanent tooth causing localized periodontal problems. Corrective fixed orthodontic treatment can hinder oral hygiene with consequent stagnation of plaque that aggravates periodontal complications. It is important the follow up of the patient during orthodontic treatment and professional oral hygiene sessions, periodic checks, and motivational reinforcement must be performed.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
The parents provided written and signed informed consent for their son to be involved in the study and to publish the observational clinical data.
STANDARDS OF REPORTING
This report follows the protocol established by STROBE statement.
FUNDING
This work was supported by grant: “Contributo premiale 2013, Bando di Rilevanza Nazionale, L.R. n. 7/2007” from the University of Cagliari and the Regione Autonoma della Sardegna.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
To Giovanni Mautarelli, specialista in ortognatodonzia Brindisi DDS, Private Practice, Brindisi, Italy.


