All published articles of this journal are available on ScienceDirect.
Effect of Clinical Use and Sterilization Process on the Transition Temperature Range of Thermally NiTi Alloys
Abstract
Background:
Thermally activated nickel-titanium wires have been widely used by orthodontists due to more constant forces, generation over longer activation spans, greater resistance to permanent deformation, superelasticity characteristics when cyclically loaded, better spring-back and less hysteresis.
Objective:
The purpose of this study was to evaluate the influence of clinical use and sterilization process on the Transition Temperature Range (TTR) of thermoset nickel-titanium wires using Differential Scanning Calorimetry (DSC).
Methods:
Sections from four nickel-titanium wires (0.019 × 0.025-inch) belonging to four different brands were assessed in four different states. Two of the wires were assessed in the “as received” state, one after 60 days of clinical use, and one after 60 days of clinical use and subjected to a sterilization process (autoclaving). The segments of each archwire were tested using DSC at temperatures ranging from −80°C to 150°C at a rate of 10°C/min.
Results:
All the nickel-titanium memory thermoset wires presented with desirable property for clinical use. The shape memory property was not influenced by clinical use and sterilization process.
Conclusion:
There was no change in TTR of the nickel-titanium wires after clinical use and sterilization.
1. INTRODUCTION
Nickel–Titanium (NiTi) wires were introduced to orthodontics in the 1970s because they presented with desirable mechanical properties for orthodontic movement, such as flexibility, low modulus, high resilience, and shape memory, thereby allowing the wires to return to their original shape upon deformation and promoting alignment of the teeth [1]. Since then, several studies have been conducted to enhance the physical properties of these archwires with the aim of improving their use in clinical practice. These studies resulted in the development of a new NiTi wire, which had both shape memory characteristics and superelasticity [2, 3].
Thermally activated NiTi wires belong to the new generation and are characterized by their thermoelastic effect (shape memory), which is related to the Transition Temperature Range (TTR) of the alloy releasing low and continuous forces even in large deflections. The complete transformation of martensite to austenite occurs at a certain temperature called the Austenite Finish Temperature (Af). This Af temperature should correspond to a temperature of the oral cavity. This is particularly important in orthodontics because it determines the mechanical performance of the NiTi archwire during treatment [4, 5].
Nowadays, thermally activated NiTi wires are widely used by orthodontists owing to several factors, including the generation of constant forces over longer activation spans, high resistance to permanent deformation, superior stability, good superelasticity characteristics when cyclically loaded, improved spring-back properties, and low hysteresis. The desirable mechanical properties of NiTi alloy wires and their relatively high cost have prompted many clinicians to recycle these wires. In a survey conducted by Buckthal et al. it was noticed that approximately 52% of the orthodontists who use NiTi wires recycle them [6]. The aim of the present study was to evaluate the influence of the clinical use and sterilization process on TTR of thermally activated NiTi archwires using the Differential Scanning Calorimetry (DSC) method.
2. MATERIALS AND METHODS
The study was conducted on four segments (0.019 × 0.025-inch) of thermally activated NiTi wires from four commercial brands: NeoSentalloy F200 (GAC, Bohemia, USA); Copper NiTi 35°C (Ormco, Glendora, USA); Flexy Thermal 35°C (Orthometric, Marília, Brazil), and Heat Activated NiTi (Highland Metals, San Jose, USA).Two of the arch wires were used “as received,” one after 60 days of clinical use, and one after 60 days of clinical use and subjected to sterilization process using autoclaving (Table 1).
| Commercial Wires | Model | Dimension | Country | Batch Number | Number of Wires |
|---|---|---|---|---|---|
| Ormco Corp. | Cooper NiTi 35°C | 0.019x0.025” | USA | 090924641 | 4 |
| GAC | NeoSentalloy | 0.019x0.025” | USA | K442 | 4 |
| Orthometric | Flexy Thermal Smart 37°C | 0.019x0.025” | Brazil | 1008925208 | 4 |
| Highland Metals | Heat Activated NiTi Arches | 0.019x0.025” | USA | 38222 | 4 |
Specimen preparation for DSC analysis comprised sectioning of 8 mm segments from the premolar area (straighter portion of the arch) in each arch form. The segments weighed approximately 8 mg on a precision electronic scale with 10 µg accuracy (semi-analytical electronic scale, Sartorius, 60905472 Serial number, Goettingen, Germany). The specimens were obtained using a diamond saw connected to a pneumatic sectioning machine under cooling and at low speed in order to avoid mechanical stresses and heating that could alter the microstructure of the wire.
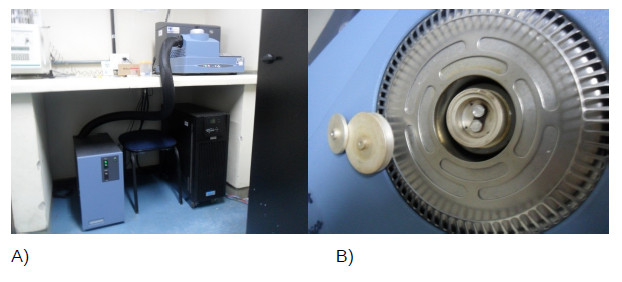
The tests were performed following the guidelines of the International Organization for Standardization (ISO), ISO 15 841 (ISO, 2006), and the American Society for Testing and Materials (ASTM), ASTM D3418-08 (ASTM, 2008). DSC (model Q20; TA Instruments, New Castle, DE, USA) was used for scanning of the thermally activated arch wires (Fig. 1).
Each specimen was reweighed in a precision electronic scale with 10 µg accuracy, placed in an aluminum crucible, and sealed. An empty aluminum crucible was used as inert reference. DSC was calibrated prior to testing, and the heating chamber was filled with nitrogen atmosphere (50 ml/min) in order to prevent water condensation and oxidation of the material. The heating and cooling rates were determined at 10°C/min with temperatures ranging from −80°C to 150°C. All samples were subjected to two cycles to ensure complete heating and cooling of the alloy.
Graphs of the curves of the exothermic and endothermic reactions during cooling and warming, respectively, were obtained via the Platinum Software® (TA Instruments, New Castle, DE, USA), which demonstrated the manner in which the intersection of the tangents to peak slopes are used to determine various transition temperature points.
The temperatures and enthalpy changes related to phase transformations obtained in the DSC tests during cooling and heating is described in Tables 2 and 3.
3. RESULTS
Tables 2 and 3 show the results of DSC and the enthalpy for cooling and heating, respectively. Variations in the martensite start and end temperatures under the different conditions tested are shown in Table 2. This TTR characterizes formation of the martensite phase of the thermal NiTi alloy. The alloys that were tested did not present large variations in temperatures in the different conditions analyzed.
In case of the heating endset measures, only small differences were observed between the wires “as received 1”, “as received 2”, “60 days in clinical use”, and “60 days in clinical use + sterilization process” for each commercial brand, with exception of the Highland Metal archwires, which showed a difference of 7.75°C (Table 3). NeoSentalloy GAC appeared to be greatly influenced by the conditions tested in the heating onset.
Af is characterized by complete formation of the austenite phase in the thermal NiTi alloys and should be close to the oral temperature for better clinical applicability of the archwires. Orthometric Flexy Thermal 37°C presented with Af values closest to that of the oral cavity, which remained unchanged under the conditions tested (Table 4).
| Commercial Wires | Condition | Cooling Onset (°C) | Cooling Endset (°C) | Enthalpy (J/g) |
|---|---|---|---|---|
| Copper NITI ORMCO | “As received” 1 | 13.50 | -10.38 | 13.36 |
| Copper NiTi ORMCO | “As received” 2 | 14.02 | -9.98 | 14.97 |
| Copper NiTi ORMCO | “60 days in clinical use” | 13.69 | -10.55 | 13.50 |
| Copper NiTi ORMCO | “60 days in clinical use + sterilization process” |
14.14 | -9.88 | 14.48 |
| NeoSentalloy GAC | “As received” 1 | -22.39 | -59.44 | 5.96 |
| NeoSentalloy GAC | “As received” 2 | -23.42 | -59.39 | 6.14 |
| NeoSentalloy GAC | “60 days in clinical use” | -22.93 | -51.83 | 8.04 |
| NeoSentalloy GAC | “60 days in clinical use + sterilization process” |
-22.29 | -51.15 | 8.51 |
| Orthometric Flexy Thermal 37°C | “As received” 1 | 17.80 | -0.48 | 17.88 |
| Orthometric Flexy Thermal 37°C | “As received“ 2 | 17.50 | -1.57 | 17.70 |
| Orthometric Flexy Thermal 37°C | “60 days in clinical use” | 17.33 | -1.53 | 17.42 |
| Orthometric Flexy Thermal 37°C | “60 days in clinical use + sterilization process” |
17.46 | -1.40 | 16.86 |
| Highland Metals | “As received” 1 | -31.35 | -61.03 | 2.27 |
| Highland Metal | “As received”2 | -32.90 | -52.41 | 0.30 |
| Highland Metals | “60 days in clinical use” | -31.75 | -65.04 | 1.77 |
| Highland Metals | “60 days in clinical use + sterilization process” |
-31.17 | -60.86 | 3.17 |
| Commercial Wires | Condition | Heating Onset (°C) | Heating Endset (°C) | Enthalpy (J/g) |
|---|---|---|---|---|
| Copper NITI ORMCO | “As received” 1 | 9.04 | 31.16 | 12.91 |
| Copper NiTi ORMCO | “As received” 2 | 8.96 | 30.96 | 14.29 |
| Copper NiTi ORMCO | “60 days in clinical use” | 8.17 | 30.53 | 13.50 |
| Copper NiTi ORMCO | “60 days in clinical use + sterilization process” |
8.86 | 31.20 | 14.23 |
| NeoSentalloy GAC | “As received 1 | 13.79 | 30.72 | 17.53 |
| NeoSentalloy GAC | “As received” 2 | 12.33 | 29.29 | 18.03 |
| NeoSentalloy GAC | “60 days in clinical use” | 19.87 | 28.78 | 17.96 |
| NeoSentalloy GAC | “60 days in clinical use + sterilization process” |
19.92 | 28.80 | 17.96 |
| Orthometric Flexy Thermal 37°C | “As received” 1 | 17.76 | 35.64 | 17.44 |
| Orthometric Flexy Thermal 37°C | “As received “ 2 | 17.16 | 35.42 | 16.80 |
| Orthometric Flexy Thermal 37°C | “60 days in clinical use ” | 17.38 | 35.32 | 16.62 |
| Orthometric Flexy Thermal 37°C | “60 days in clinical use + sterilization process” |
17.38 | 35.50 | 16.51 |
| Highland Metals | “As received” 1 | 10.98 | 32.81 | 16.42 |
| Highland Metal | “As received”2 | 9.95 | 38.70 | 14.01 |
| Highland Metals | “60 days in clinical use” | 10.44 | 30.95 | 16.63 |
| Highland Metals | “60 days in clinical use + sterilization process” |
9.29 | 33.71 | 16.08 |
| Commercial Wires | “As Received” 1 | “As Received” 2 | “60 Days in Clinical Use” | “60 Days in Clinical Use + Sterilization Process” |
|---|---|---|---|---|
| Copper NiTi ORMCO | 31.16 | 30.96 | 30.53 | 31.20 |
| NeoSentalloy GAC | 30.72 | 29.29 | 28.78 | 28.80 |
| Orthometric Flexy Thermal 37°C | 35.64 | 35.42 | 35.32 | 35.50 |
| Highland Metals | 32.81 | 38.70 | 30.95 | 33.71 |
4. DISCUSSION
The different commercial brands used in this study were based upon the previous studies, which had evaluated the thermal transition interval of the wires using DSC and reported good results of the Af temperature [4, 7, 8]. Ren et al., evaluated the TTR of nine commercial thermal NiTi archwires and concluded that the temperature range varies according to the trademarks [9]. Another study evaluated TTR of seven NiTi archwires of 0.019 × 0.025-inch and concluded that the thermally activated NiTi archwires present great variability. In addition, the elastic parameters of each NiTi archwire should be provided by the manufacturers to allow achievement of the best clinical performance possible [8].
The present study was realized with thermally activated NiTi archwires (0.019 × 0.025-inch) because of its ability to present good control over tooth movement during leveling and alignment [10]. DSC used to measure the temperatures and enthalpies has been shown to be effective in several studies [5, 11, 12], although there are other methods, such as conventional X-Ray Diffraction (XRD), that can be used to measure TTR [9, 11, 13]. Two-wires of each commercial brand were used as control to provide parameters that confirmed whether the changes in TTR had occurred because of clinical use and sterilization. Pompeii-Reynolds and Kanavakis [14] rated Af of Copper NiTi archwires (0.016 and 0.016 × 0.022-inch) at temperatures of 27°C, 35°C, and 40°C; statistically significant differences were observed for the 0.016-inch/27°C (P = 0.041) and 0.016 × 0,022-inch/35°C (P = 0.048) wires. The sterilization process using autoclave was chosen as the most commonly used method of sterilization by dentists in clinical practice [15].
Af temperature is of great clinical importance because it is at this temperature that the phase transformation of the thermally activated NiTi archwire occurs, thereby promoting leveling and alignment of the teeth [16]. Therefore, archwires with Af temperature closer to that of the oral cavity (35°C–37°C) are considered to be the best choice [17, 18]. The results of the present study showed that there was a little difference in Af temperature between the brands, except for Highland Metals, which presented with a variation of 7.75°C between the “as received” wires and “after clinical use” wires. Biermann et al. compared TTR of Copper NiTi at Af temperatures of 27°C and 35°C under the conditions “as received” and “used in the mouth for a period of 1–3 weeks” and did not find any statistical differences between the two [19]. In another study, the Af temperature nickel-titanium wires coated black oxide (Black DiamondTM) were evaluated by DSC machine in the forms “as received” and 60 days after clinical use. Statistically significant differences were not found in the thermal transition values in groups [20]. Several studies have evaluated the influence of the sterilization process on the mechanical properties of thermally activated NiTi wires [6, 15, 21-23]; however, there are no studies on the influence of clinical use and the sterilization process on TTR of these NiTi archwires. A study by Alexandrou et al. [24], evaluated the influence of the sterilization process on TTR of 33 endodontic files made from NiTi alloy. They were subjected to 11 cycles of sterilization and proved that the sterilization process had no effect on the TTR of these files. When evaluating one cycle of sterilization in NiTi wires after its use for 60 days in the oral cavity, minor differences were obtained in Af temperatures between the samples “60 days in clinical use” and “60 days in clinical use + sterilization process” (Table 4).
The enthalpy values recorded in the study of thermoset NiTi wires show that there were minor differences between the different states of wires belonging to various trademarks. Because the enthalpy values are considered as a reliable indicator for phase transformations as demonstrated by Brantley et al. [25], these changes can be considered within normal limits. This implies that thermoset NiTi wires maintain their memory properties after clinical use and one cycle of sterilization.
4.1. Clinical Implications
The clinical importance of using thermally activated NiTi archwires is based on the fact that it allows for the insertion of rectangular wires during the early stages of leveling and alignment, resulting in a three-dimensional correction of tooth positioning. As the rectangular, thermally activated NiTi archwires are subjected to deflections of greater magnitude because of the presence of crowding, it requires more time of permanence in the oral environment. Because of the manufacturing process, the costs of these archwires are considered to be too high by the orthodontists, and some suggest sterilization of these wires through autoclave without knowledge of the changes that could occur on the wire properties.
Our results show that there are minor differences in the Af temperatures of the thermoactivated nickel-titanium archwires after 60 days of clinical use and after 1-cycle sterilization process, but these differences do not imply undesirable effects on shape memory property.
CONCLUSION
There was no clinical difference in the TTR of thermally activated NiTi wires after clinical use and 1-cycle sterilization process. More studies are needed to confirm this behavior of thermoactivated nickel-titanium alloys when subjected to more than one sterilization cycle and their influence on their physical and mechanical properties.
LIST OF ABREVIATIONS
| NiTi | = Nickel-Titanium |
| TTR | = Transition Temperature Range |
| Af | = Austenite Finish Temperature |
| DSC | = Differential Scanning Calorimetry |
| XRD | = X-Ray Diffraction |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
International Organization for Standardization (ISO), ISO 15841 (ISO, 2006) and American Society for Testing and Materials (ASTM), ASTM D3418-08 (ASTM, 2008) guidelines and methodology were followed.
FUNDING
None.
AVAILABILITY OF DATA AND MATERIALS
Data sharing is not applicable in this study as no new datasets were generated in the research.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This article is based on research submitted by Dr. Bruno Silva Vieira in partial fulfillment of the requirements for the MSc. degree in Orthodontics at Uningá Faculty. BSV contributed to patient treatment, data collection, statistical analyses, data interpretation and manuscript draft. RHC contributed to project idealizer, research supervisor. KMSF contributed to data checking, manuscript draft and corrections. FPV contributed to data checking, manuscript draft and corrections. RCG contributed to data checking, manuscript draft and corrections. RCGB contributed to data checking, manuscript draft and corrections. All authors read and approved the final manuscript.


