Comparative Evaluation of Retreatability of Endodontically Treated Teeth using AH 26, Fluoride Varnish and Mineral Trioxide Aggregate-based Endodontic Sealers
Abstract
Background and Objectives:
Endodontic sealers are used to fill the gap between the root filling material and canal walls. Retrievability is an important requirement for sealers and root filling materials in non-surgical endodontic retreatment. This study sought to assess the retreatability of fluoride varnish, AH 26 and Mineral Trioxide Aggregate (MTA)-based sealers using Cone-Beam Computed Tomography (CBCT).
Materials and Methods:
This in vitro, experimental study evaluated 45 extracted single-rooted, single-canal human mandibular premolars. Teeth with cracks or fracture were excluded. The root canals were prepared using ProTaper Universal rotary system up to size F4 according to the manufacturer’s instructions. The teeth were then randomly divided into three groups of 5% fluoride varnish, AH 26 and MTA Fillapex. CBCT scans were obtained of the teeth with 200 μm voxel size. MATLAB R2012 software was used to quantify the amount of sealer remaining in the canal. Two observers evaluated the images. Data were analyzed using SPSS via the Kruskal-Wallis and Mann Whitney tests.
Results:
The amount of sealer remaining in the root canals was significantly different among the three groups (P<0.05). The amount of AH 26 sealer remaining in the root canals (1.91±1.46) was significantly greater than MTA Fillapex (0.62±0.26) and fluoride varnish, but the latter two were not significantly different in this respect (P>0.05).
Conclusion:
Considering the adequate adhesion of fluoride varnish to dentin, its cariostatic effect and low cost, it seems to be a suitable alternative to the commonly used endodontic sealers.
1. INTRODUCTION
Non-surgical endodontic retreatment is performed to remove the root filling materials and clean, shape and disinfect the root canal system for the second time [1]. Gutta-percha and sealers are commonly used for filling of the root canal system [2]. Endodontic sealers are applied to fill the porosities and the gap between the root filling material and the root canal walls [3-5]. Retrievability is an important requirement for sealers and root filling materials in endodontic retreatment [6, 7]. The success of non-surgical endodontic retreatment depends on efficient cleaning, shaping and disinfection of parts of the root canal system that remained intact in the primary endodontic treatment [8]. These intact areas often contain necrotic tissues and harbor residual bacteria that are responsible for post-operative endodontic complications [9]. Root filling materials, however, serve as a mechanical barrier and prevent the contact of irrigating solutions and endodontic instruments to the root canal walls. They consequently hinder the elimination of necrotic tissues and residual bacteria [10]. Complete removal of root filling materials provides a path from the coronal towards the apical region that allows mechanical and chemical disinfection of the root canal system and dentinal tubules and subsequent reduction of bacterial load [11].
Many sealers are available for root canal treatment. Epoxy resin sealers such as AH 26 provide high bond strength to dentin [12, 13] and reportedly, high amounts of these sealers remain in the root canal system following non-surgical endodontic retreatment [14]. Moreover, these sealers have high penetration depth into root dentin, which complicates their elimination from the root canal system [15]. Mineral Trioxide Aggregate (MTA) based sealers were introduced to the market and soon gained popularity due to their optimal bio-compatibility and sealing properties [16]. It has been reported that these sealers also remain in the root canal system following endodontic retreatment [17]. These sealers result in the formation of hydroxyapatite crystals between dentinal canal walls and sealer and therefore, their elimination from the root canal wall and dentinal tubules is challenging [18].
Fluoride varnish is commonly used as a cariostatic solution for caries prevention, as a coating material for avulsed teeth with delayed replantation and also for the treatment of dentin hypersensitivity [19, 20]. Fluoride varnish, combined with zinc oxide eugenol and calcium hydroxide, was recently used as a root canal filling material in primary teeth [20]. Evidence shows that fluoride varnish has optimal sealing ability and biocompatibility comparable to those of AH 26 [21].
Retrieval and retreatability of root filling materials during endodontic retreatment have been evaluated using stereo-microscopy, scanning electron microscopy and periapical radio-graphy. Some studies have used Cone-Beam Computed Tomography (CBCT) for evaluation of root morphology. CBCT provides three-dimensional (3D) images in axial, sagittal and coronal planes without superimposition of the adjacent structures. CBCT is capable of visualizing the root canal system as accurate as in a cleaned extracted tooth. Low patient radiation dose, high resolution and short scanning time are among the advantages of CBCT compared to other imaging modalities such as Computed Tomography (CT). CBCT provides a 3D view of the roots and details of the root canals non-invasively and can also precisely reveal the periapical lesions early in their development [22]. This study aimed to assess the retreatability of fluoride varnish, AH 26 and MTA-based endodontic sealers using CBCT.
2. MATERIALS AND METHODS
Sample size was calculated to be 15 samples in each group assuming alpha = 0.05 and beta= 0.20 using PASS 11 software. The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1396.572). The teeth were disinfected using 1% sodium hypochlorite solution and were stored in 0.1% thymol. Teeth with cracks or fracture were excluded. A #10 K-file (Dentsply Maillefer, Ballaigues, Switzerland) was introduced into the canal until its tip was visible at the apical foramen. Working length was determined to be 1 mm short of this length. The root canals were instrumented by ProTaper Universal rotary system (Dentsply Maillefer, Ballaigues, Switzerland) up to size F4 using the crown-down technique according to the manu-facturer’s instructions. The canals were rinsed with 5.25% sodium hypochlorite solution during filing. Also, 17% ethylenediaminetetraacetic acid (Asia Chemi Teb Co., Tehran, Iran) was used for 1 minute for smear layer removal. All canals were then rinsed with saline and dried. The teeth were randomly divided into 3 groups (n=15) as follows:
- Group 1: Root canals were filled with gutta-percha and AH 26 sealer (Dentsply DeTrey, Konstanz, Germany).
- Group 2: Root canals were filled with gutta-percha and MTA-based sealer (MTA Fillapex; Angelus, Londrina, PR, Brazil).
- Group 3: Root canals were filled with gutta-percha and 5% fluoride varnish as sealer (Duraflur; Pharma-science, Montreal, Quebec, Canada).
Since, the fluoride varnish appears radiolucent on CBCT scans, it was mixed with meglumine (Darupakhsh, Tehran, Iran) in 1:1 ratio to confer opacity to the sealer for enhanced visualization on CBCT scans.
A standardized gutta-percha master cone size 30 was fitted with tug back to the working length. The sealers were introduced into the canal using a Lentulo spiral (Dentsply Maillefer). Cold lateral compaction with accessory gutta-percha cones size 15 was performed until accessory cones could not be introduced into the root canal for more than 5 mm. The excess gutta-percha was removed with a heated plugger to ensure standardized length of the root filling. Subsequently, the quality and apical extension of the root canal filling were evaluated on digital radiographs in the buccolingual and mesiodistal directions.
The teeth were radiographed (Minray; Soredex, Tuusula, Finland) with the exposure settings of 60 kVp, 6 mA and 0.20 s time with different angulations to verify the quality of the root filling. Specimens exhibiting voids were discarded and replaced.
All endodontic procedures were performed by the same operator.
The access cavity in all teeth was restored and sealed with composite resin. The teeth were then incubated at 37°C and 100% humidity for 2 months.
ProTaper Universal Retreatment system (Dentsply Maill efer, Ballaigues, Switzerland) operating at 300 rpm was used to remove the root canal filling materials from the root canal system using the crown-down technique. The canals were rinsed with 5.25% sodium hypochlorite solution during the process. A final rinse with 5 mL of 17% ethylenediaminetetraacetic acid was also carried out and the canals were dried with paper points. All endodontic procedures were performed by the same operator.
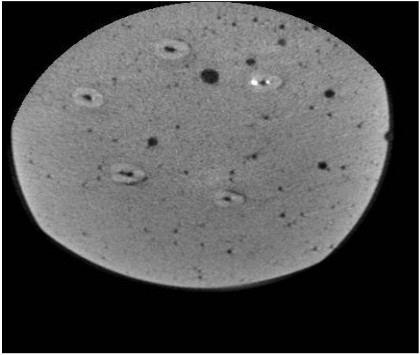
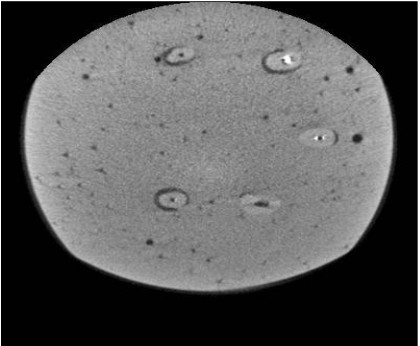
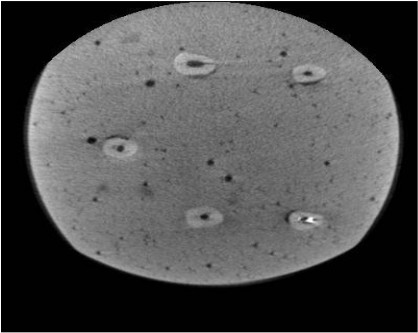
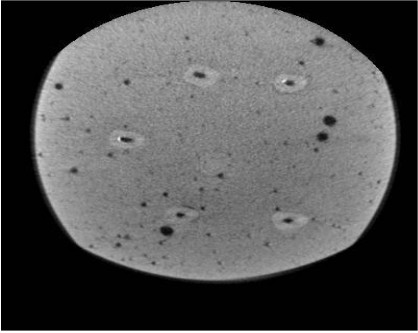
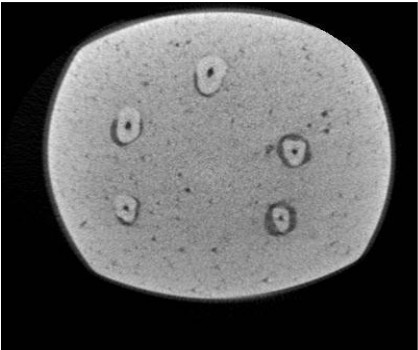
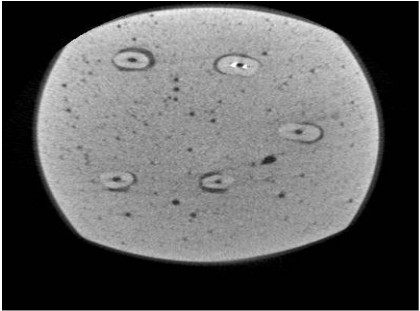
All teeth were then subjected to CBCT (Cranex 3D, Soredex, Tuusula, Finland) with 200 μm voxel size, 0.5 mm slice thickness and 0.5 mm slice interval. The axial and coronal sections of the teeth were inspected using On Demand 3D Dental software (CyberMed, Seoul, Korea) and saved in DICOM format. MATLAB R2012 (V.14) was used to quantify the amount of residual sealer in the root canal system such that image reconstruction was first performed (Figs. 1-6). Each tooth was considered individually. Gaussian and nonlinear diffusion filters were used for noise reduction. By applying a threshold, the residual sealers were cropped and separated from other parts of the image. These areas were summed up for each tooth and served as the total volume of sealer remaining in each canal.
Two observers (one oral and maxillofacial radiologist with 8 years of clinical experience and one endodontist with 10 years of clinical experience) evaluated the images. Data were analyzed using SPSS version 24 (SPSS Inc., IL, USA). The three sealers were compared using the Kruskal-Wallis test, and pairwise comparisons were carried out using the Mann Whitney test at P < 0.05 level of significance.
3. RESULTS
The intra- and inter-observer agreements were found to be 86% and 83%, respectively, which indicated high agreement in the assessment of images. Comparison of the amount of residual sealers revealed that the amount of residual sealer was 1.91 ± 1.46 for AH 26, 0.62 ± 0.26 for MTA Fillapex and 0.26 ± 0.14 for 5% fluoride varnish (Table 1). The Kruskal-Wallis test found a significant difference in this respect among the three groups. Pairwise comparisons by the Mann Whitney test (Table 2) revealed that the amount of AH 26 sealer remaining in the root canals was significantly higher than that of MTA Fillapex and 5% fluoride varnish (P<0.05). The amount of 5% fluoride varnish and MTA Fillapex remaining in the root canals was the same (P>0.05).
| Sealer | Mean | Standard Deviation | Kruskal-Wallis test Statistics | P value |
|---|---|---|---|---|
| AH 26 | 1.4631 | 1.4631 | 4.21 | 0.044 |
| MTA Fillapex | 0.62771 | 0.2680 | ||
| Fluoride varnish | 0.26048 | 0.1409 |
| Sealer 1 | Sealer 2 | Mean Difference | P value |
|---|---|---|---|
| AH 26 | MTA Fillapex | 1.20 | 0.047 |
| AH 26 | Fluoride varnish | 1.32 | 0.038 |
| MTA Fillapex | Fluoride varnish | 0.128 | 0.625 |
4. DISCUSSION
Failure of primary endodontic treatment leads to persistent periapical disease, postoperatively [23]. Factors such as presence of necrotic tissue and bacterial biofilm in the root canal, coronal leakage and recurrent caries can cause treatment failure [24]. These etiologic factors should be eliminated to allow healing of the periapical lesion. Efficient cleaning of the root canal system and complete removal of all root filling materials from the root canal system are necessary in endodontic retreatment. Evidence shows that maintaining the canal patency and adequate working length in endodontic retreatment increases the rate of successful recovery of periapical tissue [23].
Several endodontic sealers have been introduced to the dental market and the retreatability of these sealers has been evaluated. In this study, fluoride varnish was used as an endodontic sealer and its re-treatability was compared with that of AH 26 and MTA Fillapex using CBCT.
The method used for the assessment of the amount of residual sealers in the root canal system plays an important role in accuracy of the results obtained. Previous studies on this topic mainly sectioned the teeth longitudinally and observed the internal canal walls using digital radiography, scanning electron microscopy or a stereomicroscope. These methods were two-dimensional and destructive, and could not precisely quantify the amount of residual filling material in the root canal system [16]. Micro-CT has been successfully used as a research tool for evaluation of root canal anatomy [25], efficacy of root canal preparation techniques [26], quality of obturation methods and retrieval of root filling materials from the root canal system [27]. However, it is not applicable for clinical use and an alternative method suitable for use in the clinical setting with comparable accuracy is required. Recent studies used CBCT for the evaluation of root canal system. CBCT seems to be a suitable alternative to micro-CT for clinical purposes [28]. Moreover, it has been demonstrated that the accuracy of CBCT is much higher than that of different forms of CT namely spiral CT and peripheral quantitative CT [29, 30]. Low patient radiation dose, high resolution and short scanning time are among the advantages of CBCT over the afore-mentioned imaging modalities. CBCT provides a 3D image of the root and root canal details in a non-invasive manner [29].
The current findings revealed that the amount of AH 26 sealer remaining in the root canals (1.91±1.46) was significantly higher than MTA Fillapex (0.62 ± 0.26) and fluoride varnish (0.26 ± 0.14). The amount of fluoride varnish and MTA Fillapex remaining in the root canals was the same.
Obviously, factors responsible for superiority of a particular sealer as an ideal root filling material can also be responsible for longer substantivity and more difficult retrieval of the sealer from the root canal system during endodontic retreatment [31]. Several physical properties affect the penetration depth of sealers into the dentinal tubules. The surface tension and flow of sealers are important factors determining their penetration depth into the tubules. For instance, the lower the film thickness of a sealer or the higher its flow, the greater the chance of sealer penetration into the tubules and accessory canals [32]. Accordingly, high viscosity of sealers containing MTA results in their poor adaptation to the root canal walls [33, 34]. This can explain the lower amount of MTA Fillapex remnants in the root canal system compared to AH 26 in our study. Adhesion to dentinal walls is another factor affecting the retrievability of materials from the root canal system. Resin sealers such as AH 26 penetrate into dentinal tubules and form a monoblock and therefore, are harder to retrieve [22]. Moreover, the bond strength and quality of the interface layer formed between the sealer and root canal dentin in resin sealers are much higher than those of other sealers such as MTA Fillapex. This is another reason explaining more difficult retrieval of resin sealers from the root canal system [35, 36]. Lower amount of MTA Fillapex remnants in the root canal system following retreatment may be attributed to two factors: low bond strength of MTA Fillapex to root dentin and questionable biomineralization of MTA Fillapex [37, 38].
The concept of biomineralization requires further explanation. The superior performance of MTA has been extensively reported in the literature and can be attributed to its biomineralization ability. MTA can interact with a phosphate-containing fluid and produce calcium-deficient B-type carbonated apatite via an amorphous calcium phosphate phase. The apatite formed as such deposits on collagen fibrils and triggers the formation of an interfacial layer with tag-like structures at the MTA-dentin interface. Moreover, the biomineralization process reportedly increases the resistance to MTA dislodgement from dentin [39-41]. However, the low bond strength of MTA Fillapex has been attributed to the low adhesion capacity of tag-like apatite crystals [37].
MTA is a bioactive material that can form a hydroxyapatite layer on its surface and chemically bond to the internal root canal dentinal walls [42]. However, MTA Fillapex sealer is mainly composed of resin and silica and only contains 13.2% MTA. This results in its lower bond strength and less sealing ability compared to AH 26 [43]. Neelakantan et al. [16], compared retreatability of two MTA-based sealers namely MTA Fillapex and MTA Plus with AH Plus by the ProTaper Universal Retreatment rotary system using CBCT and concluded that although none of the sealers could be completely eliminated from the root canal walls, the amount of MTA Fillapex sealer remaining on canal walls was lower than that of MTA Plus. The amount of AH Plus remaining on the surface was greater than other sealers [16]. They also reported that the time required for retrieval of MTA Fillapex in root canal retreatment was shorter than that for AH Plus resin sealer. Shorter time of retreatment of teeth filled with MTA Fillapex may be attributed to lower bond strength of this sealer to dentin [37,44]. Santos et al. [22], compared MTA Fillapex, AH Plus, Sealapex and Endofill in terms of retreatability and the amount of residual sealer in the root canal system using radiography and scanning electron microscopy. They concluded that MTA Fillapex was better eliminated from the root canal walls than other sealers, and the amount of residual MTA Fillapex in the root canal was less compared to other sealers. Their findings were in agreement with our results. Uzunoglu et al., [45] compared the retreatability of root canals filled with gutta-percha and iRoot SP (Bioceramic sealer), MTA Fillapex (MTA-based sealer) and AH 26 (epoxy resin sealer) using ProTaper Universal Retreatment system and a stereomicroscope. They concluded that none of the tested sealers could be completely eliminated from the root canal system. The amount of iRoot and MTA Fillapex sealer remnants in the root canals was greater than other sealers. Their results were different from our findings, which may be attributed to the use of different methods of assessment (CBCT in our study versus stereomicroscope in their study), duration of sealer remaining in the canal for setting (2 months in our study versus 2 weeks in their study) and adhesive properties of sealers [37]. On the other hand, Reyhani et al. [44], stated that the bond strength of resin sealers to dentin was much higher than that of MTA Fillapex.
In the present study, 5% fluoride varnish was used as a new sealer and the results showed that its retreatability was similar to that of MTA Fillapex. Studies on the application of fluoride varnish as an endodontic sealer and its properties (e.g. its bacterial leakage) such as that of Rao et al. [20], and Parirokh et al. [19] confirmed that it can be successfully used as an endodontic sealer. Also, Forghani et al. [21], evaluated the cytotoxicity of fluoride varnish as an endodontic sealer on human gingival fibroblasts and concluded that its bio-compatibility is comparable to that of AH 26 [21]. Thus, fluoride varnish can be used as an endodontic sealer due to its availability, biocompatibility, insignificant bacterial leakage, optimal antimicrobial properties and fluoride release potential.
Limitations of this study were its in vitro design, not using solvents such as chloroform in endodontic retreatment and not making comparisons with other commonly used endodontic sealers. Further studies are required to address these topics.
CONCLUSION
The results showed that the amount of fluoride varnish sealer remaining in the root canals was comparable to that of conventional commonly used sealers such as MTA Fillapex and less than that of AH 26. Thus, considering the optimal adhesion of fluoride varnish to dentin, its cariostatic effect and low cost, it seems to be a suitable alternative to the commonly used endodontic sealers.
ETHICS APPROVAL AND CONSENT TO PARTI-CIPATE
The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC. 1396.572).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008 (http://www.wma.net/en/20activities/10ethics/10helsinki/).
CONSENT FOR PUBLICATION
The participants provided written informed consent to be involved in this study.
AVAILABILITY OF DATA AND MATERIALS:
The data supporting the findings of the article is available in the Hamadan University of Medical Sciences at [http://dentistry. umsha.ac.ir/].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


