All published articles of this journal are available on ScienceDirect.
Mental Well-being of the First and Final-Year Medical and Dental Students of Kermanshah University of Medical Sciences
Abstract
Background and Aim:
Medical and dental students are predisposed to developing psychiatric disorders owing to heavy physical, intellectual, and emotional activities. This study was conducted to evaluate the mental health status of medical and dental students.
Materials and Methods:
This cross-sectional study was conducted on the first- and final-year medical and dental students at Kermanshah University of Medical Sciences in 2016. The mental health status was measured by the General Health Questionnaire-28 (GHQ-28) involving somatic, social, anxiety, and depression domains. Scores > 6 (out of 28) and > 2 (out of 7) were considered to show psychiatric disorder for each domain, respectively. Data were analyzed by SPSS-18 using Kruskal-Wallis and Chi-square tests (P< 0.05).
Results:
The participants consisted of 246 students (39.4% first- and 37.8% last-year medical students; 8.1% first- and 14.6% last-year dental students) aged 18-37 years (22.6 ± 3.3). Psychiatric disorder, somatic symptoms, social dysfunction, anxiety, and depression were experienced by 44.7, 42.7, 46.3, 49.6, and 28.5% of the students, respectively. The prevalence of psychiatric disorder was comparable between the first- and final-year medical students (40.2% and 48.4%, respectively; P = 0.258). The final-year dental students significantly underwent more psychiatric disorder than the first-year dental students (61.1% and 20%, respectively; P = 0.003). There were no significant differences between the medical and dental students in the first (P = 0.089) and final (P = 0.196) years. There was also no significant association between the occurrence of psychiatric disorder and gender and age group (P> 0.05).
Conclusion:
Psychiatric disorder was common among dental and medical students. Hence, preventive and control measures are suggested to improve their mental health.
1. INTRODUCTION
Health-related university degree programs, including medicine, dentistry, and nursing have been recognized as the most difficult educational programs. Students involved in such university programs are at the risk of developing psychiatric disorders due to emotional exhaustion, particularly in the final years of their education [1]. Medical educational centers are stressful environments which negatively affect the students’ academic performance, physical health, and mental health [2-4]. However, students with good mental health are more successful academically [5]. Studies have shown that a significant percentage of medical students [6] and dental students [7, 8] have undesirable mental health. A study on dental students showed that dentistry program was associated with stressful factors that could have a negative impact on the emotional status of these students [9].
Various tools and questionnaires are used in scientific research to assess mental health. A questionnaire which is very popular among researchers is the General Health Questionnaire (GHQ) (Table 1). It has two versions, one is GHQ-28 which has 28 items and the other one is a short form with 12 items (GHQ-12). Malakouti et al., verified the validity of the Persian version of the GHQ-28 [10, 11]. Mental health status affects students’ academic achievement and performance. Therefore, assessment of the mental health of medical/dental students is a necessity for the authorities of medical and dental schools. Evidence shows that students are predisposed to different stressful events at different academic levels [4]. The educational environment has become an essential area to understand the reasons for this phenomenon as well as to intercept and prevent future burnout events through a correct psychological preparation among medical students. The aim of this study was to evaluate the mental health of the first- and final-year medical and dental students studying in Kermanshah University of Medical Sciences, Kermanshah, Iran in 2016.
| HAVE YOU RECENTLY | |
|---|---|
| 1. | Been feeling perfectly well and in good health? |
| 2. | Been feeling in need of a good tonic? |
| 3. | Been feeling run down and out of sorts? |
| 4. | Felt that you are ill? |
| 5. | Been getting any pains in your head? |
| 6. | Been getting a feeling of tightness or pressure in your head? |
| 7. | Been having hot or cold spells? |
| 8. | Lost much sleep over worry? |
| 9. | Had difficulty in staying asleep once you are off? |
| 10. | Felt constantly under strain? |
| 11. | Been getting edgy and bad-tempered? |
| 12. | Been getting scared or panicky for no good |
| 13. | Found everything getting on top of you? |
| 14. | Been feeling nervous and strung-up all the time? |
| 15. | Been managing to keep yourself busy and occupied? |
| 16. | Been taking longer over the things you do? |
| 17. | Felt on the whole you were doing things well? |
| 18. | Been satisfied with the way you’ve carried out your task? |
| 19. | Felt that you are playing a useful part in things? |
| 20. | Felt capable of making decisions about things? |
| 21. | Been able to enjoy your normal day-to-day activities? |
| 22. | Been thinking of yourself as a worthless person? |
| 23. | Felt that life is entirely hopeless? |
| 24. | Felt that life isn’t worth living? |
| 25. | Thought of the possibility that you might make away with yourself? |
| 26. | Found at times you couldn’t do anything because your nerves were too bad? |
| 27. | Found yourself wishing you were dead and away from it all? |
| 28. | Found that the idea of taking your own life kept coming into your mind? |
2. MATERIALS AND METHODS
This cross-sectional study was approved by the Research Deputy of Kermanshah University of Medical Sciences, Kermanshah, Iran (#97069). We didn’t perform sample size calculation because all of the first- and final-year students participated in this study. The list of the first- and final-year students was obtained from the education offices of the medical and dental schools. The inclusion criteria were being the first or final-year medical or dental student, admission to the university through the Iranian National University Entrance Examination (i.e., Konkoor), and consent for participation in the study. The exclusion criteria consisted of graduate students, students being transferred from other universities, and students of oral and dental hygiene.
The students were contacted in person by the research team in classrooms (in case of first-year students) or in clinical departments (final-year students). Firstly, the objectives of the study were explained to them, and if they agreed, they were asked to fill out a checklist and the GHQ-28.
The checklist was used to collect demographic characteristics, including age and gender and academic variables, including academic major and academic level. To assess the students’ mental health status, the GHQ-28 was administered. The GHQ-28 contains 28 items which assess four subscales (each subscale has 7 questions). The four subscales are somatic symptoms (items 1 to 7), anxiety /insomnia (items 8 to 14), social dysfunction (items 15 to 21), and depression (items 22 to 28).
The total score of the questionnaire is calculated by summing the scores of all items. The scoring method was as follows: zero was allocated to options “A” and “B” and 1 was allocated to options “C” and “D”. In this method, the total scores were calculated by summing the scores of 28 items. Scores ≥6 were considered to indicate a psychiatric disorder. For the four-item scales, scores 2 and >7 were considered to show psychiatric disorder.
The prevalence of psychiatric disorder was calculated generally and separately in the four subscales based on the scores. These frequencies were then compared between the subgroups (i.e., first-year medical students, final-year medical students, first-year dental students, and final-year dental students).
2.1. Statistical Analyses
The data were analyzed by SPSS software (ver. 17.0). Since Kolomogrov-Smirnov test showed that data of variables’ levels don’t have a normal distribution (P <0.001) so non-parametric tests were used to compare. The subgroups were compared by Chi-square test. The significance level was set at 0.05.
3. RESULTS
A total of 246 students aged 18-37 years with a mean age of 22.6 ± 3.3 years were studied. Table 2 presents the frequency distribution of the studied students based on demographic characteristics (age and gender) as well as educational variables (academic major and academic level).
Of the students, 110 (44.7%) suffered from a psychiatric disorder. Somatic symptoms, anxiety/insomnia, social dysfunction, and depression were observed in 42.7%, 46.3%, 49.6%, and 28.5% of students, respectively (Fig. 1).
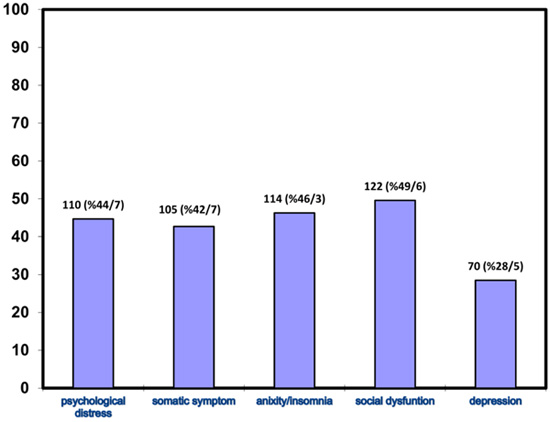
Table 3 presents a comparison of the frequencies of the psychiatric disorder, according to demographic and educational characteristics. There was no significant difference in the frequency of psychiatric disorder between the male and female students (P= 0.428) and among various age groups (P= 0.156). The prevalence of psychiatric disorder was 40.2% in the first-year medical students, 48.4% in the final-year medical students, 20% in the first-year dental students, and 61.1% in the final-year dental students (P = 0.018).
The pair comparisons of the psychiatric disorder by Mann-Whitney test showed that it was significantly higher in the final-year dental students than in the first-year dental students (P = 0.003). But no significant difference was observed between the first-year and final-year medical students (P = 0.258). There were also no significant differences between the first-year medical and dental students (P = 0.089) and the final-year dental and medical students (P = 0.196) (Table 4).
| – | – | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 112 | 45.5% |
| Female | 134 | 54.4% | |
| Age group, year | ≤ 20 | 103 | 41.9% |
| 21-24 | 62 | 25.2% | |
| ≥ 25 | 81 | 32.9% | |
| Academic major and level | Medicine (first-year) | 97 | 39.43% |
| Medicine (final-year) | 93 | 37.8% | |
| Dentistry (first-year) | 20 | 8.13% | |
| Dentistry (final-year) | 36 | 14.63% |
| – | – | Good Mental Health (i.e., GHQ-28 Total Score < 6) | Psychiatric Disorder (i.e., GHQ-28 Total Score ≥ 6) | P value* |
|---|---|---|---|---|
| Gender | Male | 65 (58%) | 47 (42%) | 0.428 |
| Female | 71 (53%) | 63 (47%) | ||
| Age group | ≤ 20 | 64 (62.1%) | 39 (37.9%) | 0.155 |
| 21-24 | 33 (53.2%) | 29 (46.8%) | ||
| ≥ 25 | 39 (48.1%) | 42 (51.9%) | ||
| Educational major and level | Medicine (first-year) | 58 (59.8%) | 39 (40.2%) | 0.017 |
| Medicine (final-year) | 48 (51.6%) | 45 (48.4%) | ||
| Dentistry (first-year) | 16 (80%) | 4 (20%) | ||
| Dentistry (final-year) | 14 (38.9%) | 22 (61.1%) |
| – | Psychiatric disorder | P value* |
|---|---|---|
| Medicine (first-year) | 39 (40.2%) | 0.256 |
| Medicine (final-year) | 45 (48.4%) | |
| Dentistry (first-year) | 4 (20%) | 0.003 |
| Dentistry (final-year) | 22 (61.1%) | |
| Medicine (first-year | 39 (40.2%) | 0.088 |
| Dentistry (first-year) | 4 (20%) | |
| Medicine (final-year) | 45 (48.4%) | 0.194 |
| Dentistry (final-year) | 22 (61.1%) |
4. DISCUSSION
The mental health of university students can affect their academic performance and achievement [12, 13]. Given the importance of this factor, the present study examined the mental health of medical and dental students. Mental health status was assessed by the GHQ-28 questionnaire. The GHQ-28 has been used previously in numerous studies for this purpose [14-16]. The educational environment may have an impact on mental health. In order to control the effect of this confounding factor, only students who were admitted to the university through the National University Entrance Examination and were studying at Kermanshah University of Medical Sciences were evaluated.
According to the obtained findings, the prevalence of the psychological disorder in the medical and dental students surveyed was 44.7%. This figure is higher than that of the mental disorders of the Iranian general population older than 15 years, which has been reported to be 20.9% of the urban population and 21.3% of the rural population by the GHQ-28 [11]. In agreement with the high prevalence of mental disorders among the students of medical universities, Farahangiz et al. showed psychological disease disorder among 54.4% of the first-year to fourth-year medical students of Shiraz University of Medical Sciences [17]. The high prevalence of mental disorders (33.7% to 52.3%) among the medical and dental students has also been reported in other countries [1, 18-21].
Psychological disease is related to some risk factors such as genetic factors, undesirable economic and social status, childhood problems, undesirable events of life, and cultural background [22]. According to Mosley et al., medical education centers are stressful environments which affect the physical and psychological health of students adversely [2]. Medical sciences students are predisposed to some additional stressful factors like a large amount of academic activities [23]. Medical students are affected by factors such as a change of residence, leaving friends and acquaintances, making new friends, financial concerns, and a sense of inability in doing assignments [24]. Willcock et al., studied the final-year medical students and reported that psychological disorder aggravated during the 18-month internship period. They concluded that the internship period was a stressful period [25].
In the studied population, the prevalence rates of somatic symptoms, anxiety/insomnia, social dysfunction and depression were 42.7%, 46.3%, 49.6%, and 28.5%, respectively. Similarly, Aboalshamat et al., reported high levels of depression (69.9%), anxiety (66.4%), and stress (970.9%) among the medical and dental students [26]. Another study by Lohsoonthorn et al., indicated the poor quality of sleep (48.1%) among students (46.8% in males and 48.7% in females) [27]. Leao et al., reported a higher frequency of anxiety (27%) and depression (20%) in the final-year medical students than in the general population [28]. Another study showed that at least 27% of the students had at least one type of sleep disorder [29]. Also, Wege et al., reported higher rates of major depression, depression symptoms, and psychosomatic complaints in the medical students in Germany than in the general population [30].
Mental disorders have detrimental effects on the students’ academic performance and quality of life. Anxiety can cause mental disorders, addiction to narcotics, and even suicide in addition to decreasing the students’ academic achievement [19]. A review study reported that sleep problems could bring about decreased mental attention and academic performance, somnolence in classes, depression, high-risk behaviors, damaged social relationships, and decreased health status. Somnolence and irregular sleep patterns can have negative effects on learning ability and memory [31]. Therefore, considering the high prevalence of anxiety/insomnia in this study (43.3%), it is necessary to implement preventive and therapeutic programs.
There was no significant difference between the male (42%) and female (47%) students regarding the psychological disorder. Likewise, some studies (5, 20) have shown that the mental health of medical students is not associated with gender. However, another study reported that the mental health of the female students was more undesirable than that of the male students [32]. This discrepancy is due to the fact that mental health can be affected by a wide range of individual and environmental factors.
The result of the current study showed that psychiatric disorder was not affected by age. Likewise, Tavabi and Iranpour showed a lack of relationship between mental health and age among medical students [5]. Also, Zaid et al., reported no significant association between the prevalence of mental health disorders and age [20].
Moreover, the findings indicated that the prevalence of psychological disorder was 40.2% among the first-year medical students, 48.4% among the final-year medical students, 20% among the first-year dental students, and 61.1% among the final-year dental students. The first- and final-year medical students were comparable regarding their mental health. This is in line with the findings of Assadi et al., which showed the prevalence rates of 50% and 41.4% for mental problems among the first- and final-year medical students of Tehran University of Medical Sciences, respectively, indicating no significant difference between the two groups [33]. The current study and other studies showed a high prevalence of mental disorders among the first- and final-year medical students. Yet, psychiatric disorders are caused by various factors which need to be investigated by future studies in this field.
The frequency of psychological disease was significantly higher in the final-year dental students than the first-year dental students. Al-Saleh reported a higher frequency of anxiety among the final-year dental students and interns. They attributed this higher rate of anxiety to the clinical activities which are associated with considerable anxiety [34]. In agreement with this finding, another study showed a higher rate of anxiety among the senior dental students [35]. Stewart et al., showed that the mental function of dental students was impaired as they had poor compatibility with problems, low self-esteem, and high isolation, anxiety, depression, and anger [36].
The current study showed no significant differences between the first-year dental and medical students as well as the final-year dental and medical students regarding mental health status. Similarly, Al-Nimer [18] and Costa et al. [1], reported no significant differences between the medical and dental students.
A limitation of the present study was that the students’ mental health was assessed without considering important factors such as familial and economic conditions, marital status, and the course scores which can affect the mental health. Also, there is no specific threshold for the four scales and the cutoff point to recognize suspected students with a mental disorder or those requiring treatment depends on the population [37]. Therefore, in the current study to the cutoff point of more than 6 out of the total score of 28, the cutoff point of 2 was considered for the subscales with a total possible score of seven.
CONCLUSION
The current study showed that psychological disorder was high among the first- and final-year dental and medical students, especially among the final-year dental students. Mental health was not affected by age or gender. The mental health of dental and medical students is suggested to be addressed through educational and therapeutic programs. This can improve the academic status of the students and consequently promote the scientific level of medical universities.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This cross-sectional study was approved by the Research Deputy of Kermanshah University of Medical Sciences, Kermanshah, Iran (#97069).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008.
CONSENT FOR PUBLICATION
All participants signed the study consent before participating in the study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


