All published articles of this journal are available on ScienceDirect.
Influences of Masticatory Function Recovery Combined with Health Guidance on Body Composition and Metabolic Parameters
Abstract
Background:
Tooth loss reduces masticatory function. Insufficient masticatory function causes an increase in carbohydrate intake while decreasing the intake of foods with a low Glycemic Index (GI) and high in protein, antioxidants, dietary fiber, vitamins, and minerals. Protein-energy malnutrition may lead to metabolic syndrome, frailty, and faster onset of Non-Communicable Diseases (NCDs). Individuals with tooth loss resulting in problematic eating habits require behavior modification and health guidance.
Objective:
This report aims to evaluate the influence of dental prostheses combined with health guidance on body composition and metabolic parameters.
Methods:
Data were collected from three subjects: Two with molar loss and one with edentulism. Masticatory function was restored in each subject through prosthodontic treatment. Masticatory performance was evaluated before and after the prosthodontic treatment by having the subjects chew a gummy jelly and measuring the glucose extraction. Questionnaires were used to assess food intake and lifestyle habits. Health guidance based on the results of the questionnaires was conducted simultaneously with the prosthodontic intervention. Body composition and blood pressure were measured and blood tests were performed at baseline and around 90 days after the first health guidance session.
Results:
Masticatory ability, body-mass index, basal metabolism standard value, body-fat percentage, and intake of certain nutrients improved in all cases. Blood pressure and hemoglobin A1c improved in two cases.
Conclusion:
Masticatory function recovery combined with health guidance was effective in preventing the onset or deterioration of NCDs in patients with masticatory dysfunction.
1. INTRODUCTION
The World Health Organization (WHO) categorizes diseases that can be prevented by improving lifestyle habits as Non-Communicable Diseases (NCDs). NCDs, including cancer, diabetes, cardiovascular disease, and respiratory disease, are the leading cause of death worldwide [1].
The habit of eating high-calorie low-nutrient meals such as those included in high carbohydrate diets and high-fat diets is thought to induce NCDs [2, 3]. These dietary habits seem to be related to masticatory function and health behavior, and the amount of tooth loss due to caries and periodontitis is related to masticatory performance [4, 5].
Impaired eating habits may also be caused by malocclusion due to various reasons such as skeletal deformity of the jaws, misshapen teeth, or temporomandibular joint disorder. Isola et al. [6], stated that up to 93% of patients with Juvenile Idiopathic Arthritis (JIA) may present with early inflammatory findings indicating temporomandibular joint disorder, and that their quality of life, including eating, smiling, oral hygiene, and daily activities, may deteriorate. The masticatory function of these patients decreases during the process of orthodontic treatment. Isola et al. [7] also stated that biologically active substances such as inflammatory cytokines are expressed in response to the consecutive mechanical stress caused by the application of an orthodontic force. Thus, a prosthodontic treatment that restores masticatory function, as well as orthodontic and aesthetic treatments, should be promoted with consideration of the relationship with comprehensive metabolism and nutritional status.
Tooth loss significantly impairs masticatory performance and causes the intake of sufficient nutrition difficult. Individuals with tooth loss frequently consume soft meals with high carbohydrate content (high-calorie, low-nutrient meals) [8]. As they are easy to swallow, these types of food tend to induce fast eating, overeating, and postprandial hyperglycemia, which may trigger a deterioration of carbohydrate metabolism and metabolic syndrome [9, 10].
These individuals also tend to avoid vegetables and meat that require masticatory ability. As a result, they may develop Protein-Energy Malnutrition (PEM); this can happen even with sufficient calorie intake. PEM may lead to chronic hypoalbuminemia (3.4 mg/dl or less), sarcopenia (decrease of skeletal muscle mass), or a long-term decrease in bone mass [11]. In the elderly, sarcopenia is a factor that contributes to the deterioration of an individual’s quality of life, eventually shortening his or her lifespan [12].
It has been reported that improvement in NCDs is promoted by optimizing nutrition intake and preventing an increase in the Glycemic Load (GL) [13, 14]. However, when the masticatory performance of a patient with NCDs is low, it is difficult for him or her to consume adequate nutrition and become disease-free [8]. Improving masticatory function through prosthodontic treatment seems to be the first step needed to improve the status of NCDs. Therefore, restoration of masticatory function through prosthodontic intervention seems to favorably affect the prevention of NCD onset and the deterioration of health.
Meanwhile, even when the masticatory function is normal or has been restored through dental treatment, ideal eating habits cannot always be obtained [15]; this is because we use gustation to sort out food [16, 17]. Moreover, the reasons for tooth loss include patients’ inadequate eating habits and health behaviors. Therefore, it seems that behavior modification through health guidance, which should be carried out simultaneously with the recovery of masticatory function, is necessary for patients with masticatory dysfunction to acquire ideal dietary habits.
The main goal of prosthodontics and orthodontics is aesthetic recovery and improvement in masticatory function [18]. However, this goal must include primary prevention of NCDs through improvement in nutritional intake, body composition, and metabolism. This broad approach including a range of goals requires tailor-made health guidance for patients in addition to the restoration of masticatory function.
It is important to quantitatively evaluate whether the recovery of masticatory function can contribute to the prevention of onset and deterioration of NCDs.
This case report is a preliminary study of three subjects with molar tooth loss, the most common cause of masticatory dysfunction. This study aims to observe and evaluate the influence of recovery of masticatory performance through prosthodontic treatment, combined with the improvement of eating habits through proper health guidance, on health-status indicators.
2. MATERIALS AND METHODS
Data were collected from three subjects, two males and one female, between the ages of 67 and 82 years; two subjects were obese and had molar loss, and one was edentulous and malnourished. The inclusion criteria were molar loss and a body type that deviated from the subjective standard. Exclusion criteria were subjects classified as Eichner classification A (occlusal support exists on both sides), and subjects with a Body Mass Index (BMI) within the reference of 20 to 26. In addition, as a confounding factor affecting carbohydrate metabolism and body composition, we confirmed that the subjects included in the study were not taking any supplements or prescribed medications.
We conducted prosthodontic treatment to restore the masticatory function and provided personal health guidance to improve subjects’ eating habits. Among the variables related to NCDs, we focused on carbohydrate metabolism, lipid metabolism, and body composition, as these reflect the influence of dietary habits.
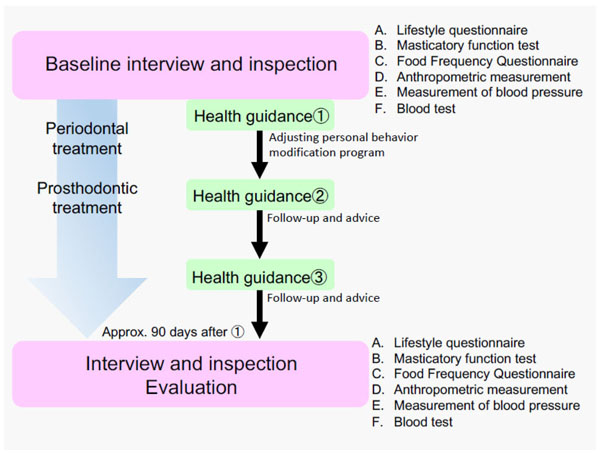
The same intervention protocol was followed for all subjects (Fig. 1).
2.1. Baseline Interview and Inspection
The following interview and inspection were conducted before treatment intervention.
2.1.1. Lifestyle Questionnaire
We conducted a face-to-face interview using a questionnaire to elicit information on the subjects’ medical history, dietary habits, physical activities, lifestyle habits, family composition, socio-economic conditions, etc. (Table 1).
2.1.2. Masticatory Function Test
The subjects’ masticatory function was measured before and after prosthodontic treatment. The subjects chewed a gummy jelly containing glucose for 20 s, then rinsed lightly with 10 ml of water. The concentration of glucose eluted from the gummy jelly in the water was measured with a glucose measuring device, the Gluco-Sensor GS-II (GC Corporation, Tokyo, Japan) [19]. The average of the values measured three times on each subject’s deficient side was considered the level of masticatory ability, and Standard Deviation (SD) was calculated accordingly.
| Have you ever had any of the following illnesses? | Hypertension/diabetes/periodontal disease/stomach or duodenal ulcer/stroke/cerebral infarction/intracranial hemorrhage/hyperlipidemia/liver disease/cancer/angina/myocardial infarction/none |
| Do you currently take any medicines? | Yes (number of medicines: …..)/No |
| What time do you get up and sleep? | Get up at about …../Sleep at about…… |
| What time do you have each meal of the day? | Breakfast at about ……./No breakfast Lunch at about ……./No lunch Dinner at about ……./No dinner Midnight snack at about ……./No midnight snack |
| How often do you eat out? (including take-out food) | Every day/Sometimes (….. times a week)/ No eating out |
| Do you pay attention to sugar intake? | Yes, very much/Sometimes/No |
| Do you pay attention to the order of eating (i.e., vegetables first)? | Yes, very much/Sometimes/No |
| How do you eat your meal every day? | Eat until full/Finish before getting full/Eat small |
| How do you drink water every day? | 1 – 2ℓ consciously/When thirsty/Rarely |
| Do you take any nutritional supplements? | Yes (number of supplements:……)/No |
| How do you sleep at night? | Sufficient/Not enough/Not at all |
| When do you go to bed? | More than 2 hours after dinner/1-2 hours after dinner/Within an hour after dinner |
| What do you think of your body type? | Fat/Thin/Standard |
| Do you think you lack exercise? | Yes/No |
| Do you feel a decrease in muscle strength? | Yes/No |
| Do you continue exercise of more than 30 minutes more than twice a week for more than a year? | Yes/Yes, but for less than a year/No such exercise |
| Do you feel stress in daily living? | Not at all/Sometimes/Yes, on a daily basis |
| Is there a lot of trouble? | Not at all/Sometimes/Yes, on a daily basis |
| Do you smoke? | Yes (….. tobaccos a day/for ….. years)/No/I used to, but I quit …...years ago |
| How many times do you drink alcohol? | Every day/….times a week/….. times a month/ Rarely/I used to, but I quit |
2.1.3. Food Frequency Questionnaire (FFQ)
Surveys on food intake and frequency per week were conducted using questionnaires on 29 food groups and 10 different cooking methods. From the results of the questionnaires, habitual nutrient intake per day was estimated and evaluated. Nutrients such as protein, vitamin B1, B6, C, folic acid, calcium, and zinc were evaluated for sufficiency rates against the adult general intake standard based on the Dietary Reference Intakes for Japanese (2015) by Ministry of Health, Labor and Welfare in Japan [20]. Food Intake Frequency Survey FFQ Ver. 3.5 (Kenpakusha, Tokyo, Japan) was used for data analysis.
2.1.4. Anthropometric Measurements
Body composition was determined with bioelectrical impedance analysis (BIA) (ITO-InBody 370: InBody Japan Co., Ltd., Tokyo, Japan) [21, 22]; the values of body weight, BMI, basal metabolism standard value, body-fat percentage, and visceral-fat level were used for analysis.
2.1.5. Measurement of Blood Pressure
Blood pressure was measured using a digital automatic sphygmomanometer (HEM-7070: OMRON Corporation, Kyoto, Japan) by winding the manchette around the upper arm.
2.1.6. Blood Test
Blood samples were collected from the median cubital vein in the morning after fasting for more than 12 h; data were collected on the level of Hemoglobin A1c (HbA1c) as a glucose metabolism index and the Levels of Albumin (Alb), Total Protein (TP), HDL-Cholesterol (HDL-C), LDL-Cholesterol (LDL-C), and Triglyceride (TG) as the parameters for nutritional status. The investigation was entrusted to a clinical laboratory testing company (SRL, Inc., Tokyo, Japan).
2.2. Recovery of Masticatory Function with Dental Prosthesis and Health Guidance
Prosthodontic treatment was started immediately after the initial examination. The prosthodontic treatment was performed with dental implants (cases 1 and 2) and complete dentures (case 3), according to conventional procedures. Periodontal therapy was administered to the subjects with symptoms of periodontitis (cases 1 and 2), and inflammation was controlled.
In parallel with the prosthodontic treatment, we extracted information regarding the subjects’ eating and lifestyle habits from the results of the lifestyle questionnaire and FFQ. Based on the anthropometric measurements, we created a tailor-made health guidance program for each subject to optimize his or her lifestyle; the guidance was provided using our original teaching material. The contents of the health guidance program are summarized in Table 2.
2.3. Questionnaires and Clinical Examination after Intervention and Evaluation
After prosthodontic and periodontal treatment and 90 days after the initiation of health guidance, we again carried out the survey and clinical inspection (detailed in sections 2.1.1 through 2.1.6) and performed a comparative analysis.
The timing of the evaluation was determined considering the necessary interval for a change in body composition after the initiation of behavior modification.
3. CASE REPORTS
3.1. Case 1: 67-Year-Old Male Subject
3.1.1. Baseline Oral Condition and Prosthodontic Intervention
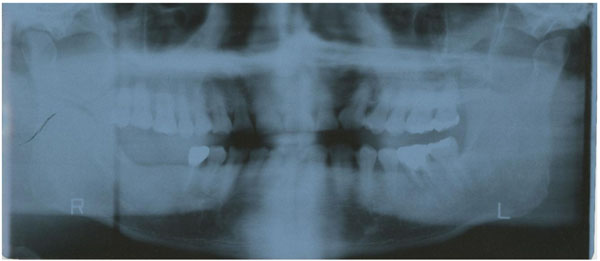
The subject had decreased masticatory function due to loss of the right lower first and second molar teeth (Eichner classification B1) and persistent chronic inflammation due to moderate periodontitis, which could cause an aggravation of NCDs (Fig. 2a).
The lost molar teeth were restored with dental implants according to conventional procedures (Platon Japan Co., Ltd., Tokyo, Japan) (Fig. 2b).
3.1.2. Baseline General Condition (Table 3a)
The FFQ showed that high GI carbohydrates such as noodles and rice accounted for 66% of the subject’s total calorie intake, while the intake of protein, vitamin A, B1, C, D, calcium, iron, zinc, and dietary fiber was below the required amount [20]. The protein-energy ratio was less than 10%. The total quantity of physical activity and exercise was smaller than the normal standard of activity for Japanese males over 65 years of age [23].
3.1.3. Results (Table 3b)
After prosthodontic treatment, the masticatory ability of his right jaw improved from 136 mg/dl (SD ± 15.0) to 237 mg/dl (SD ± 34.6).
Chronic inflammation caused by periodontitis also recovered. The subject’s intraoral condition was conducive to an improvement in NCDs after prosthodontic intervention and health guidance. BMI, body-fat percentage, visceral-fat level, and HbA1c improved, and blood pressure approached the reference value. Lifestyle habits and physical activity status also improved. As for nutrient intake, the intake rates of vitamin B1 and C, folic acid, calcium, and zinc improved.
3.2. Case 2: 71-Year-Old Female Subject
3.2.1. Baseline Oral Condition and Prosthodontic Intervention
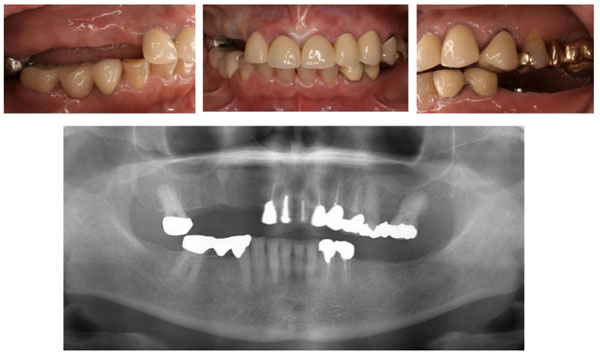
Teeth from 3 to 6 in the upper right quadrant and 5 to 7 in the lower left quadrant were missing (Eichner classification B3) (Fig. 3a). The subject complained of pain caused by the partial dentures she was wearing. She experienced difficulty and stress during mastication.
We conducted periodontal treatment to control chronic inflammation and restored masticatory function with dental implants (Platon Japan Co., Ltd., Tokyo, Japan) according to conventional procedures (Fig. 3b).

| Nutrition and meal intake | Meals regularly taken three times a day and finished before getting full |
| Types of carbohydrates and blood glucose level monitored | |
| Staple foods replaced with low GI carbohydrates(like whole grain bread or millet) | |
| Types and intake frequency of lipids monitored | |
| Difference between saturated fatty acids and unsaturated fatty acids discussed | |
| Trans-fatty acids avoided | |
| Recommendations given for intake of omega-3 polyunsaturated fatty acids | |
| Intake of meat, fish, and vegetables increased after recovery of masticatory function | |
| Vegetables discussed as a source of vitamins, minerals, and dietary fiber | |
| Discussion regarding failure of calorie restriction diets without considering nutrition | |
| Target basal metabolic rate calculated from thebasal metabolism standard value for each age and sex | |
| Understanding of basal metabolism and exercise guidance | Target amount of exercise suitable for the subjects set basedon the criterion of physical activity for those over 65 years of age(10 METs*-hours/week, regardless of exercise intensity) [23] |
| Physical activities planned according to each subject’s lifestyle (combiningaerobic exercise and anoxic exercise, sports, and daily activities) | |
| Influence on the body of lack of physical activities discussed | |
| Relationship between muscle mass, basal metabolism, and anti-aging effects discussed | |
| Diet therapy of charting daily weight ** [24] | 1) Body weight measured twice, in the morning and at night |
| 2) Subject filled in measured weight on a 100 g scale chart and drew a line graph | |
| 3) When the graph increased or decreased, they wrote the reason in the comment field | |
| 4) The target weight change was 50 to 100 g per day | |
| Understanding on sleep | Sleep and stress control, circadian rhythm, etc. discussed |
| Smoking and drinking | None of the subjects smoked Low-carb alcoholic beverages were recommended |
| Eating habits of swallowing and fasting |
| Habit of frequent eating out |
| Frequent intake of fried foods (omega-6 fat) Imbalance of fatty acids due to excessive intake of omega-6 and inadequate intake of fish (omega-3) |
| High intake of white rice and sweet bread |
| High intake of salt (9.6 g/day) |
| Drinking habits |
| Obesity |
| Metabolic disorders (hypertension and dyslipidemia) Common use of drugs for dyslipidemia |
| Physical activity: 5 METs*-hour/week (commuting by walk) |
| Exercise: 3.5 METs-hour/week (playing golf twice a month) |
| Parameters of Body Condition and Metabolism | Before Intervention | After Intervention | Items in which Favorable Change was Found (+) |
|---|---|---|---|
| Level of masticatory ability (right jaw, mg/dl) | 136 (SD ± 15) | 237 (SD ± 34.6) | + |
| Body Mass Index | 29.5 | 25.2 | + |
| Body weight (kg) | 91.95 | 78.55 | + |
| Basal metabolism standard value (kcal/kg/day) | 19.6 | 21.6 | + |
| Body-fat percentage (%) | 30.3 | 25.3 | + |
| Visceral-fat level | 18 | 14 | + |
| Systolic/diastolic blood pressure (mmHg) | 150/95 | 135/85 | + |
| Hemoglobin A1c (HbA1c) (%) | 5.7 | 5.3 | + |
| Albumin (g/dl) | N/A | N/A | N/A |
| HDL-Cholesterol (mg/dl) | N/A | N/A | N/A |
| LDL-Cholesterol (mg/dl) | N/A | N/A | N/A |
| LDL-Cholesterol/HDL-Cholesterol | N/A | N/A | N/A |
| Triglyceride (mg/dl) | N/A | N/A | N/A |
| Protein sufficiency rate (%) | 70 | 87.4 | + |
| Vitamin B1 sufficiency rate (%) | 72 | 78 | + |
| Vitamin B6 sufficiency rate (%) | 97 | 93 | N/A |
| Vitamin C sufficiency rate (%) | 66 | 120 | + |
| Folic acid sufficiency rate (%) | 105 | 155 | + |
| Calcium sufficiency rate (%) | 74 | 103 | + |
| Zinc sufficiency rate (%) | 75 | 78 | + |
3.2.2. Baseline General Condition (Table 4a)
The subject started a trial of improving dietary habits by herself, one year before the start of health-guidance intervention. Her body weight was reduced by 3 kg in one year; it was difficult for her to completely refrain from eating sweets because of the stress caused by being her husband’s sole nursing-care provider at home. As her lack of exercise had been inhibiting weight loss, the target value for basal metabolism was raised. She was provided information regarding Metabolic Equivalents (METs) and directed to practice higher intensity physical activities to increase fat-combustion efficiency.
3.2.3. Results (Table 4b)
The masticatory ability recovered from 70 mg/dl (SD ± 49.1) to 179 mg/dl (SD ± 10.6) and from 127 mg/dl (SD ± 7.2) to 163 mg/dl (SD ± 31.3) in the right and left jaws, respectively, after prosthodontic treatment.
After prosthodontic treatment and health guidance, BMI, body-fat percentage, visceral-fat level, and blood pressure improved, and HbA1c improved remarkably. Lifestyle habits also improved, and physical activity increased. As for nutrient intake, the rates of calcium and zinc intake improved.
| Excessive intake of free sugars due to eating between meals |
| Meat and egg intakes were half of the required amount |
| Excessive food intake at dinner |
| Obesity |
| Metabolic syndrome/history of diabetes (HbA1c: 7.0%) |
| Physical activity: 3 METs*-hour/week (dog-walking) |
| No habit of exercise |
| Parameters of Body Condition and Metabolism |
Before Intervention | After Intervention | Items in which Favorable Change was found (+) |
|---|---|---|---|
| Level of masticatory ability (right jaw, mg/dl) | 70 (SD ± 49.1) | 179 (SD ± 10.6) | + |
| Level of masticatory ability (left jaw, mg/dl) | 127 (SD ± 7.2) | 163 (SD ± 31.3) | + |
| Body mass index | 41.5 | 36.1 | + |
| Body weight (kg) | 87.15 | 75.9 | + |
| Basal metabolism standard value (kcal/kg/day) | 13.7 | 15.5 | + |
| Body-fat percentage (%) | 59.7 | 50.7 | + |
| Visceral-fat level | 18 | 16 | + |
| Systolic/diastolic blood pressure (mmHg) | 131/63 | 119/58 | + |
| Hemoglobin A1c (%) | 9.5 | 7.5 | + |
| Albumin (Alb) (g/dl) | 4.2 | 4.1 | - |
| HDL-Cholesterol (mg/dl) | 50 | 55 | + |
| LDL-Cholesterol (mg/dl) | 167 | 137 | + |
| LDL-Cholesterol/HDL-Cholesterol | 3.3 | 2.5 | + |
| Triglyceride (mg/dl) | 273 | 149 | + |
| Protein sufficiency rate (%) | 85.8 | 87 | + |
| Vitamin B1 sufficiency rate (%) | 163 | 135 | - |
| Vitamin B6 sufficiency rate (%) | 95 | 86 | - |
| Vitamin C sufficiency rate (%) | 107 | 78 | - |
| Folic acid sufficiency rate (%) | 102 | 78 | - |
| Calcium sufficiency rate (%) | 69 | 89 | + |
| Zinc sufficiency rate (%) | 69 | 76 | + |
3.3. Case 3: 82-Year-Old Male Subject
3.3.1. Baseline Oral Condition and Prosthodontic Intervention
The subject was edentulous with no dentures (Eichner classification C), resulting in masticatory dysfunction. Masticatory function was restored with complete dentures.
3.3.2. Baseline General Condition (Table 5a)
The subject was in a state of frailty and sarcopenia. He was anxious about walking by himself and regularly used a wheelchair. Health guidance focused on food selection and a cooking method suitable for the improved masticatory ability after prosthodontic treatment, including protein-rich meat and vegetables rich in vitamins, minerals, and dietary fiber.
3.3.3. Results (Table 5b)
The baseline level of masticatory ability was 39 mg/dl (SD ± 26.0) because of the lack of dentures, but after prosthodontic treatment, the level increased to 151 mg/dl (SD ± 18.6).
Improvement was noted in BMI, body-fat percentage, muscle mass, and bone mass. However, visceral-fat, HbA1c, and blood-pressure levels deteriorated. Almost all the nutrient sufficient rates improved.
The subject was in a state of sarcopenia and unable to walk. However, after prosthodontic treatment and health guidance, he no longer needed a wheelchair and started walking on his own.
4. DISCUSSION
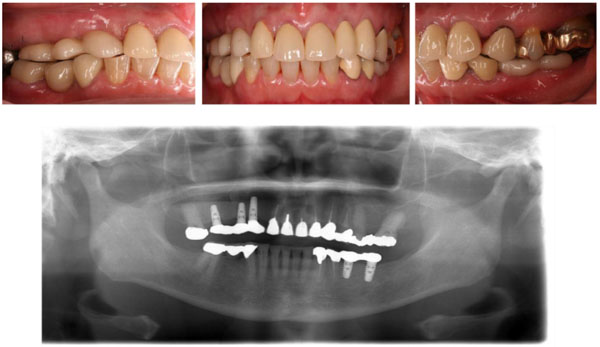
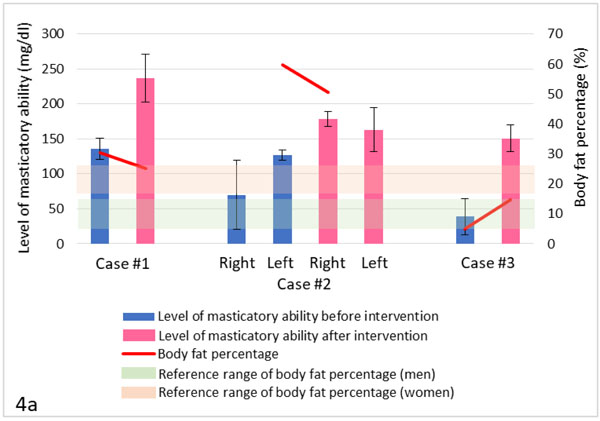
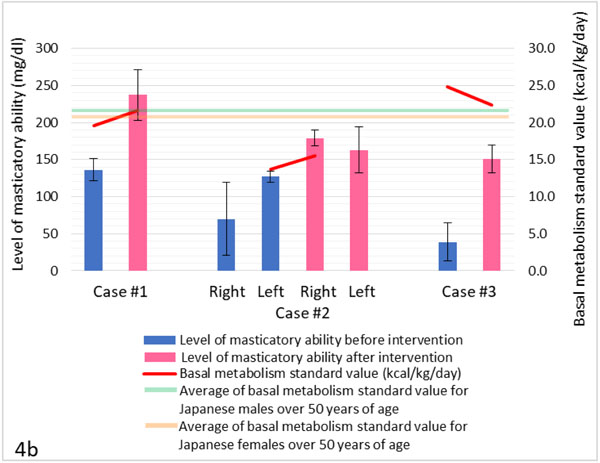
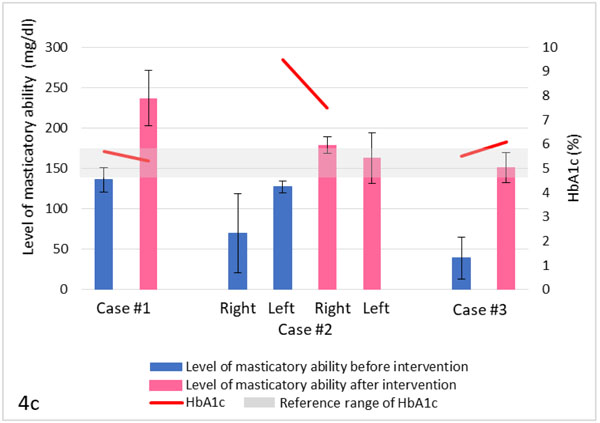
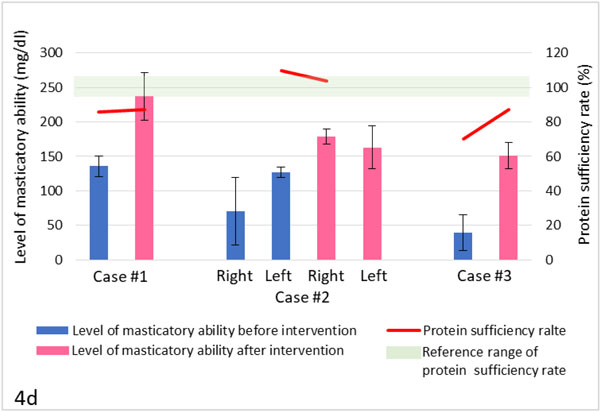
In this case report, the masticatory function of all subjects improved with dental prosthodontic treatment (Figs. 4a-4d). Due to prosthodontic treatment and health guidance, improvements were also confirmed in a wide range of items, including body composition (Fig. 4a), metabolism (Figs. 4b-4c), and nutrient sufficient rates (Fig. 4d).
There are two important features of this case report. First, recovery of masticatory function was achieved through the simultaneous use of prosthodontic treatment and health guidance. Second, we defined numerical variations in nutritional status, body composition, and metabolic parameters as the end points of prosthodontic treatment.
In cases 1 and 2, the levels of masticatory ability significantly increased after prosthodontic rehabilitation with dental implants. Even with complete dentures in case 3, the level was increased. In cases 1 and 2 with a high carbohydrate diet, HbA1c levels improved after intervention (case 1: 5.7% to 5.3%; case 2: 9.5% to 7.5%). The improvement was especially significant in case 2, although the subject was more obese than the subject in case 1. These results seem to be due to a decrease in carbohydrate intake and an increase in the intake of low-GI foods.
In cases 1 and 2, blood-pressure levels improved (case 1: 150/95 mmHg to 135/85 mmHg; case 2: 131/63 mmHg to 119/58 mmHg) and the risk of cardiovascular diseases decreased. Regarding nutrient intake, the sufficient rates of calcium and zinc improved in all cases.
Improvement in body composition was observed in all cases. In case 1, the amount of physical activity before health guidance was below the standard criterion for subjects 65 years of age and older (10 METs-hour/week). However, after guidance, the amount of activity exceeded the standard criterion for subjects 64 years of age and younger (23 METs-hour/week). In case 2, the amount of physical activity before guidance was also less than the standard criterion for subjects 65 years of age and older. However, after guidance, the subject achieved her target amount of activity of 12 METs-hour/week. Visceral-fat levels of the subjects in cases 1 and 2 gradually decreased (case 1: 18 to 14; case 2: 18 to 16). Due to the establishment of the habit of exercise as well as an improvement in eating habits, subjects were able to burn fat, maintain muscle mass, and prevent rebound.
Due to difficulties with food intake, the subject in case 3 was in a state of malnutrition with a baseline BMI of 12.8. Prosthodontic treatment made it possible for him to consume various foods, and as a result of prioritizing calorie intake, he showed an increase in BMI (17.3), muscle mass (27.7 kg to 33.6 kg), and body fat percentage (5% to 14.6%). His nutritional status also improved. Moreover, although the prescribed exercise was minimal, he started walking and no longer required his wheelchair; he also demonstrated outstanding improvement in his activity of daily living. These results indicate that, although our focus would have usually been on the nutritional problems concerning the prevention or improvement of sarcopenia and frailty, recovery of masticatory function is equally important.
The subject of case 3 was not in the habit of exercising and had an increase in visceral-fat level (1 to 8; baseline value was too low) and HbA1c (5.5% to 6.1%). There was also a rise in systolic blood pressure (106 mmHg to 151 mmHg). We assume that his acquired habit of exercise will make HbA1c and visceral-fat levels approach proper values.
These findings suggest a correlation between masticatory dysfunction, PEM, and an increase in glycemic load, as well as a correlation among masticatory dysfunction [25], PEM, and decrease in muscle mass (Figs. 4a-4d).
It seems that the evaluation method employed in this study, showing the results of health behavior in numerical values, helped raise the subjects’ awareness of health promotion. In the future, organization of a medical care system for the rehabilitation of masticatory function to promote health and improve NCDs is needed.
The issue remaining to be addressed is how to help patients recognize their own physical conditions at an early stage, understand that tooth loss or masticatory dysfunction will lead to serious health hazards; and move to action.
The main objective of orthodontic and prosthodontic treatment as well as the treatment of temporomandibular disorders has been esthetic improvement and recovery of masticatory function. Moreover, it has been reported that patient satisfaction greatly increases with expansion of the therapeutic effect; this may include an improvement in general health condition, the short-term disappearance of inflammatory response, a shortened treatment period, an improvement in quality of life, better aesthetic results, as well as an improvement in body composition and metabolism [6, 7, 25].
For stronger evidence, we should increase the number of cases, selected randomly, and make a significant difference test. This case report was a preliminary study focusing on three interesting cases; in our future research, we will examine patient satisfaction using a visual analogue scale. In addition, we will classify the selected subjects into the following groups: masticatory-function recovery, health guidance only, and non-intervention. We will examine by correlation analysis the relationships among the groups.
| Daily meals consisted of liquids such as rice porridge |
| Overwhelmingly insufficient intake of meat and vegetables was noted |
| Frailty/Sarcopenia |
| No habit of exercise |
| Wheel chair used regularly |
| Parameters of Body Condition and Metabolism | Before Intervention | After Intervention | Items in which Favorable Change was found (+) |
|---|---|---|---|
| Level of masticatory ability (mg/dl) | 39 (SD ± 26.0) | 151 (SD ± 18.6) | + |
| Body mass index | 12.8 | 17.3 | + |
| Body weight (kg) | 30.8 | 41.5 | + |
| Basal metabolism standard value (kcal/kg/day) | 24.8 | 22.4 | + |
| Body-fat percentage (%) | 5 | 14.6 | + |
| Visceral-fat level | 1 | 8 | + |
| Systolic/diastolic blood pressure (mmHg) | 106/60 | 151/76 | - |
| Hemoglobin A1c (%) | 5.5 | 6.1 | - |
| Albumin (g/dl) | 3.3 | 3.7 | + |
| HDL-Cholesterol (mg/dl) | 49 | 34 | - |
| LDL-Cholesterol (mg/dl) | 125 | 170 | - |
| LDL-Cholesterol/HDL-Cholesterol | 2.6 | 5.0 | - |
| Triglyceride (mg/dl) | 103 | 258 | - |
| Protein sufficiency rate (%) | 110 | 104 | - |
| Vitamin B1 sufficiency rate (%) | 64 | 76 | + |
| Vitamin B6 sufficiency rate (%) | 64 | 75 | + |
| Vitamin C sufficiency rate (%) | 115 | 123 | + |
| Folic acid sufficiency rate (%) | 136 | 153 | + |
| Calcium sufficiency rate (%) | 60 | 80 | + |
| Zinc sufficiency rate (%) | 90 | 103 | + |
Treatment intervention to recover masticatory function combined with appropriate health guidance according to patients’ conditions may contribute to the prevention of onset or deterioration of NCDs through an improvement in nutritional status and body composition.
CONCLUSION
Short-term goals for the treatment of individuals with masticatory dysfunction include recovery of masticatory function, aesthetic restoration, and inflammation control. The final goal, however, seems to be health promotion and prevention of the onset or deterioration of NCDs. It is considered that an inclusive medical care system combining dental prosthetic treatment with personal health guidance is effective for expansion of the treatment effect.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study protocol was approved by the Research Ethics Committee of School of Dentistry, Tsurumi University, Kanagawa, Japan (Approval number 1042).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. The reported experiments were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants before the study started.
FUNDING
This study was supported by the Japan Society for the Promotion of Science, Grant-in-Aid for Scientific Research (C), 2016-2018 (Grant Number JP16K11873).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
This study was supported by the Japan Society for the Promotion of Science, Grant-in-Aid for Scientific Research (C), 2016-2018 (Grant Number JP16K11873).
We would like to thank Editage (www.editage.jp) for English language editing.


