All published articles of this journal are available on ScienceDirect.
Recurrent Peripheral Giant Cell Granuloma: A Case Report
Abstract
Objective:
This article describes a case of a Peripheral Giant Cell Granuloma (PGCG) in a girl.
Introduction:
PGCG is a relatively infrequent benign reactive lesion of the gingiva or alveolar ridge that develops in response to local irritation. Clinical appearance consists of a firm or soft smooth surface nodule in dissimilar colors of varying size with sessile or pedunculated implantation base. Radiographic features are generally nonspecific, thereby definitive diagnosis depends on microscopic examination to confirm the entity of PGCG.
Case Report:
A 6-year-old female patient was referred to the outpatient clinic of an Oral & Maxillofacial Surgery Department with the chief complaint of an intraoral swelling. The intraoral examination showed a painless sessile mass with exophytic growth similar to a tumorous lesion located on the mandibular alveolar ridge extending from distal aspect of right mandibular primary canine to mesial aspect of first permanent molar of the same side.
Conclusion:
Peripheral giant cell granuloma is a relatively uncommon lesion in children and potential for collaboration with the treatment in young patients should be considered for a successful therapeutic approach.
1. INTRODUCTION
The Peripheral Giant Cell Granuloma (PGCG) has been well documented as a reactive hyperplastic extra-osseus lesion characterized by non-neoplastic nodular swellings that develop in response to chronic tissue injury leading to exuberant tissue response originated from periosteal or periodontal ligament cells [1-4]. Irritating factors including dental plaque and calculus, food impaction, chronic infections, periodontal disease or periodontal surgery, defective restorations, ill-fitting appliances and trauma from tooth extractions are described as possible etiological factors of PGCG [5, 6].
While a wide range of factors could be related to the emergence of PGCG, it is a relatively uncommon lesion [4] that occurs in the young as well in the elderly population, although occurrences seem to increase with age [3]. So that only about 20-30% of cases manifest in the1st and in the 2nd decades of life [7]and just 9% of thecasesoccurin children aged up to 10 years [8].
Peripheral giant cell granuloma clinically manifests as a painless smooth surface lesion, the size of which ranges from a few millimeters to several centimeters, brown, reddish or purple colored with sessile or pedunculate implantation base and consistency that varies from soft to firm [1, 8, 9]. Microscopically, a distinctive feature of PGCG is the abundance multinucleated giant cells [8] which enable it to be differentiated from similar other reactive oral lesions like pyogenic granuloma and peripheral ossifying fibroma, but is the same characteristic of central giant cell granuloma [7]. Therefore, only radiological evaluation can establish the distinction between peripheral form and central giant cell granuloma, which is an intrabony benign neoplasm of the jawbone [10].
The treatment of choice of PGCG is to eliminate the entire base of the lesion and also local factors [8, 11]. The recurrence rate after local excision is around 10% [8], probably attributed to the surgical technique used to excise the lesion [12].
Thus, the present case report describes the clinical and histopathological features of a PGCG and the atypical management of a recurrent lesion in a 6-year-old non-cooperative girl.
2. CASE REPORT
A 6-year-old female patient was referred to the outpatient clinic of an Oral and Maxillofacial Surgery Department with a chief complaint of an intraoral swelling. First and second primary molars were extracted by a general dentist and after that, the reactive lesion has been progressively growing. It was reported that the patient had undergone a surgical procedure twice to excise the lesion in another dental service, with signs of recurrence.
Preliminary inquisition of medical history includes no complication and hematological reports were noncontributory. There was nothing noteworthy at the extraoral physical examination, with no palpable regional lymph nodes.
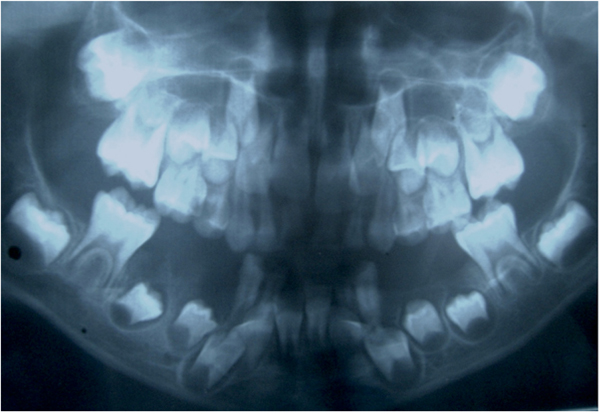
The patient was in mixed dentition with some active carious lesions and poor oral hygiene. The intraoral examination showed a painless sessile mass with exophytic growth similar to a tumorous lesion located on the mandibular alveolar ridge extending from distal aspect of right mandibular primary canine to mesial aspect of first permanent molar of the same side. The lesion was light pink to purple colored, well defined and rounded, with approximately 3 cm in its largest diameter (Fig. 1). On palpation, the lesion had a smooth surface and firm consistency with no tendency to bleed.

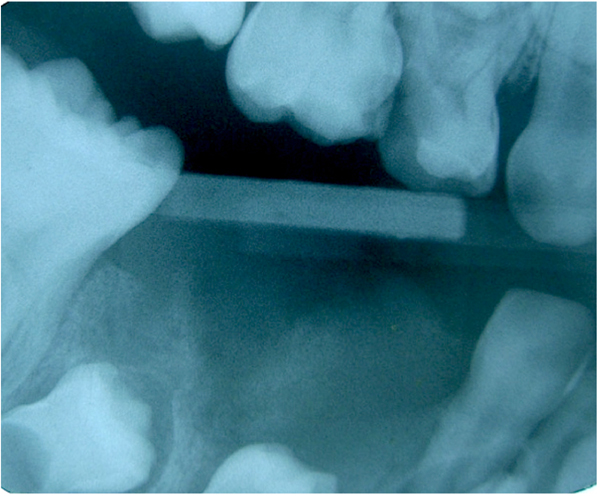
No radiographic change was observed, since there was no bony involvement of the lesion (Figs. 2 and 3). Axial section of cone beam computed tomography revealed a nodular image with soft-tissue density, partially clear limits, measuring approximately 2.0 x 2.0 x 1.0 cm located in the soft tissues of the right side of the mandible.
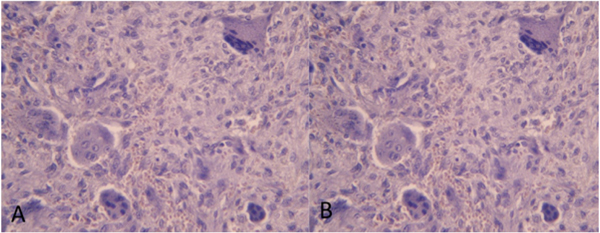
These clinical and radiographic findings indicated a benign lesion and definitive diagnosis was confirmed after histopathologic examination of incisional biopsy specimen. Microscopic examination showed abundant multinucleated giant cells organized in foci through dense fibrous connective tissue, which exhibited collagen fibers arranged in parallel bundles and bulky fibroblasts sometimes ovoid sometimes spindle-shaped (Figs. 4A and 4B). The presence of these features is indicative of Peripheral Giant Cell Granuloma (PGCG).
3. RESULTS
A decision was thus made to excise the lesion. The surgical procedure was performed under general anesthesia with nasotracheal intubation and local infiltration of Prilocaine Hydrochloride 3% + Felipressin 0.03 IU / ml (Cristália Produtos Químicos Farmacêuticos, Itapira, SP, Brazil) with a sterilized cold scalpel nº 15 (Lamedid Com. Serv., Osasco, SP, Brazil). Care was taken to remove the entire base of the lesion. Then, the surgical wound was cauterized with an electric scalpel (Mastercut 70W, Medical Cirurgica Ltda., São Paulo, SP, Brazil) followed by irrigation with 0.9% saline solution and removal of debris. After achieving proper hemostasis, interrupted sutures were placed to close the defect with 3-0 silk suture. Excised lesion measuring approximately 2.5x 2.0 x 1.0 cm was stored in 10% formalin and sent for histopathological examination to confirm the diagnosis of PGCG.
Sutures were removed after 7 days and the treated area was still in healing phase. The child and her caregivers were advised of the importance of oral hygiene procedures for complete tissue healing.
4. DISCUSSION
Reactive Lesions (RLs) comprise Pyogenic Granuloma (PG), Fibrous Hyperplasia (FH), Peripheral Ossifying Fibroma (POF) and Peripheral Giant-Cell Granuloma (PGCG) [13]. All these reactive lesions are typically developed in response to chronic inflammation caused by various forms of low-grade chronic irritations to the oral mucosa [13]. In looking at factors that may have contributed to the development of PGCG lesions, some authors pointed out that in a total of 279 lesions pathology request forms indicated that only 18 referenced a recent extraction site [3], the presumed etiology of the lesion presented by our patient.
RLs often pose diagnostic challenges due to their overlapping clinical features [14]. Therefore, the differential diagnosis of PGCG includes besides the other reactive lesions [13], fibrous epulis, peripheral odontogenic fibroma, papilloma, hemangioma, lymphangioma, metastatic tumors of gingiva, nevi or other nodular melanomas and other inflammatory hyperplastic lesions [15, 16] all of which present with similar clinical and radiographic findings. Thus, careful medical history followed by complete physical, imaginological, and histopathological examination are critical procedures in the diagnosis process, aiming for a correct treatment plan, thereby reducing the possibility of recurrence and morbidity for patients [17, 18].
Regarding clinical characteristics, majority of the studies indicate that PGCG is more common in the mandible than in the maxilla [3, 8, 19, 20] and it occurs in the incisor and canine region [7], although according to some other authors, these lesions are located posteriorly more than anteriorly [19, 20], as observed in the present case. The lesion seems to have a slight female predilection and although it may develop at any age, it is most often observed in adults and the elderly people [1, 3, 8, 15, 19].
Consequently, few reports have been described of PGCG in children [16, 17, 20, 21], in which these lesions might show a rapid growth as well as aggressive and recurrent behavior in younger patients [5]. Moreover, dentoalveolar problems, including alveolar bone loss and tooth displacement or resorption of the subjacent teeth roots may arise [15]. PGCG may also interfere with the eruption of adjacent teeth [20] as was identified in the present case in which the crown of the underlying premolar can already be observed in the postoperative control.
Malignant transformation of PGCG has never been reported but some authors recently described an unprecedented case of giant cell lesions of the jaws [21], wherein a peripheral giant cell granuloma recurred exclusively as a central giant cell lesion in a young patient. The present case did not show any significant involvement of bone on radiological examination, which was also confirmed during the intra-operative procedure.
For the case described, considering the occurrence of successive recurrences that determined the need for repeated invasive clinical procedures in a short period of time and, in the face of this, a not very cooperative behavior identified in the clinical examination, it was decided to perform incisional biopsy due to the extensive size of the lesion and expected wound management complication. Despite similar cases of PGCG in children treated in dental outpatient clinics [16, 17, 21], in the management of the present case after the diagnosis was confirmed, surgical removal of the lesion under general anesthesia was chosen so that the child's lack of collaboration was not a reason for incomplete removal of the lesion during the surgical procedure, since it is believed that recurrences are related to the lack of inclusion of the periosteum or periodontal ligament in the excised lesion [19] and a superficial excision is prone to be performed in a patient with unfavorable behavior.
Accordingly, recommended management of peripheral giant cell granuloma aims at elimination of the entire base of the growth accompanied by eliminating any local irritating factors, as was followed in our case. The various modalities used to excise the lesion are cold scalpel, electrocautery and carbon dioxide laser and literature shows no difference between cold scalpel and CO2 laser resection of PGCG [2].
Regardless of the technique employed, successful treatment involves obtaining a precise diagnosis throughout histopathologic analysis, complete removal of the lesion accompanied by eliminating any local irritating factors, particularly emphasizing recommendations of oral hygiene maintenance [11], as was followed in the presented case.
Close follow-up is also indicated because of the recurrence rate in order to early diagnose complications or lesion relapses aiming at a more conservative management [4]. In our case, reassessments after postoperative control were not established because the treatment was performed in a dental service inserted in a hospital with urgent and emergency care. However, it is assumed that successive relapses of the lesion occurred due to the excision technique not steered precisely, lacking inclusion of entire base of the lesion in the excised specimen [6].
CONCLUSION
Peripheral giant cell granuloma is a relatively uncommon lesion in children and potential for collaboration with the treatment in young patients should be considered for a successful therapeutic approach. The successive recurrences of the PGCG lesion, in this case, were attributed to inappropriate surgical technique induced by the child's lack of collaboration during the excision procedure. Therefore, general anesthesia was used to enable complete removal of the lesion, minimizing the risk of recurrence also talking into account the psychologically comfort of the young patient.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Committee on Ethics of the State University of Paraiba, school of Dentistry, Campina Grande, Brazil.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Patient’s consent was requested and approved by the patient himself and by his mother.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


