All published articles of this journal are available on ScienceDirect.
All-On-Four Protocol With Immediate Load on Short Implants in an Atrophic Mandible: A Case Report with a 4-Year Follow-Up
Abstract
Purpose:
Edentulism has been demonstrated to have negative social and psychological effects on individuals that include adverse impacts on facial and oral esthetics, masticatory function and speech abilities, that when combined, are translated into significant reductions in patients’ quality of lives. It is well-known that immediate placement of implants is a challenging surgical procedure that requires proper treatment planning and surgical techniques. Therefore, the present study describes a 4-year follow-up case report where short implants were placed in an atrophic mandibule and were loaded with the utilization of an all-on-four prosthetic protocol.
Case report:
A 54 year-old woman dissatisfied with her oral and facial esthetics, masticatory function and speech ability came to the implantology clinic of the Positivo University seeking for oral rehabilitation treatment. After detailed physical and clinical examination, a Computer Tomography scan (CT-scan) was performed to determine the patient’s bone ridge density, dimensions and eligibility for the placement of dental implants. The CT-scan results have indicated the presence of an extremely atrophic mandibular bone ridge. The CT-scan was also used as an aid during the final restoration treatment planning in terms of vertical dimension of occlusion, masticatory function, and stabilization of the lower denture. An all-on-four protocol supported by short implants was then treatment-planned to reduce time, costs and morbidity, and also to achieve superior immediate esthetic results and masticatory function. To reconstruct the patient’s atrophic edentulous mandibule, 4 short implants, including 2 distally tilted, were placed with a final torque of 45 Ncm.
Results:
Following the development and implementation of a complex treatment plan, the patient displayed stable soft and hard tissues at 4-year postoperative follow-up assessment, demonstrating the effectiveness of the all-on-four technique supported by short implants.
Conclusion:
Within the limits of this study, the present case report demonstrated that the all-on-four prosthetic protocol with immediate loading on short implant was effective in an atrophic mandible over a 4-year follow-up.
1. INTRODUCTION
Edentulism is a current and relevant oral-health problem faced by many patients and clinicians in Brazil. It is typically associated with significant bone loss, adverse volumetric dimensional changes (atrophic mandibles) and consequent functional, esthetic, social and psychological problems [1-3]. In cases where the mandibular bone height is less than 12.0 mm, tissue augmenting techniques including bone ridge expansion and bone grafts are typically made necessary to allow the placement of traditional dental implants. Despite their wide-spread use, these techniques are clinically very challenging and display higher levels of tissue and implant morbidity. Modern oral rehabilitation strategies based on the utilization of dental implants and immediate loading techniques, have been demonstrated to allow for the rapid and efficient restoration of patients with superior esthetic and masticatory properties, while reducing the morbidity and damage to both soft and hard tissues.
Maló et al., introduced the “all-on-four” treatment concept in 2003 where the utilization of multiple abutments of different angulations [two straight (q = 90°, anterior) and two angled (35° < q < 45°, posterior)] allowed, for the first time, to fully restore complete arches based on the placement of four immediately loaded implant fixtures [4]. This treatment approach made it possible to attain satisfactory mandibular anchorage without interfering with the mental foramen or inferior alveolar nerve [4-6]. When compared to extensive surgical approaches or the utilization of removable prostheses (partial or complete dentures), this technique has been proven to be a viable and more economical treatment option for patients with edentulous mandibles and high demands for short treatment times, less invasive procedures, low morbidity, favorable prognosis and immediate quality of life [6-10].
Therefore, the aim of the present case report was to demonstrate the utility and clinical advantages of an oral rehabilitation technique based on the placement of four short implant fixtures immediately loaded with an all-on-four prosthetic protocol in an extremely atrophic mandibular bone ridge, and report the status of the case after 4 years of follow-up.
2. CASE DESCRIPTION
This case report was carried out in accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 2013.
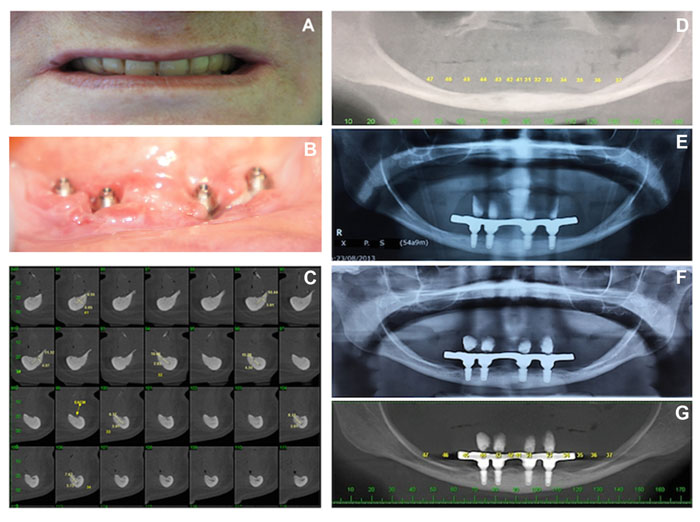
A healthy 54 year-old woman reporting chewing and prosthesis stabilization difficulties came to the implantology clinic of the Positivo University seeking for implant-based oral rehabilitation procedures. The patient was then subjected to detailed general physical and clinical examinations that revealed a set of complete dentures (upper and lower) displaying very poor adaptation, marginal sealing and loss of vertical dimension (Fig. 1A) due to strong alveolar bone resorption (both maxilla and mandibula) and the wear of resin-based prosthetic teeth. The patient was then subjected to a cone-beam computerized tomography scan (I-CAT® cone-beam CT scan, Imaging Science Corp, Hatfield, PA) that demonstrated a severely atrophic mandibular ridge with compromised bone height (10.0 mm) and width (3.0 mm) (Fig. 1B).
The treatment plan was designed based on patient’s complaints clinical conditions (atrophic mandibula) X-ray and CT scan exam (Figs. 1A, 1C and 1D). The advantages and limitations of the treatment plan proposed were explained to the patient, who accepted the treatment terms and provided signed consent. The treatment protocol was divided into two halves. The first half involved the fabrication, adjustment and delivery of a set of complete dentures (maxillary and mandibular) for long-term assessment of vertical dimension of occlusion, esthetics satisfaction and comfort levels with the newly-fabricated dentures. After several months, the patient returned to clinic and reported high satisfaction levels with the oral and facial esthetics provided by the set of complete dentures, but the instability of the mandibular prosthesis during masticatory function decreased her overall enthusiasm regarding the treatment.
The second half involved the design and fabrication of the final all-on-four restoration, as well as, the surgical planning and placement of four short implants in the atrophic mandibular ridge. The all-on-four procedure involved the utilization of four morse tapered implants (3.5 mm x 7.0 mm, Osteofit®, DSP-Biomedical, Campo Largo, Brazil) that were treatment-planned to prevent fenestration and perforation of mandibular cortical bone while reducing the chances for iatrogenic mandibular fracture during implant-placement procedures. Since the patient was satisfied with the esthetic outcomes attained by the set of complete dentures, the lower prosthesis was duplicated to serve as a multifunctional guide. One hour prior to surgical procedures, two ampules of Dexamethasone (4 mg/each) were intramuscularly administered to reduce the postsurgical edema.
2.1. Surgical Procedure and Technique Description
An incision of approximately 8.0 cm in length was made in the keratinized mucosa at the top of the lower alveolar ridge to provide an optimal surgical flap. Mucoperiosteal detachment was then performed until the mental foramen was exposed. Next, a surgical stent was used to guide the positions of the perforations. The drilling sequence recommended by the manufacturer was then used with constant irrigation using sterile saline solution. The implants were placed in a position to maintain the shoulder of the implant approximately 1.0 -1.5 mm below the crestal bone. All implants were installed with a final torque of 45 Ncm. The edges of the flap were then re-approximated and sutured using a nylon thread (5.0, Shalon Medical Ind., Indianapolis, IN, USA). Immediately after the implant insertion, abutments were loaded over a standard of 32 Ncm. Mini-abutment transfers were fixed to the surgical stent using pattern resin (GC® America Inc. Chicago, IL, USA). A condensation silicone impression material (Speedex®, Coltene/Whaledent Inc.) was then used to take impressions and fabricate a model containing the surgical stent. Mini-abutment protectors were then placed during the final surgical step.
Amoxicillin (500 mg) and Ibuprofen (600 mg) were prescribed during the postoperative period for seven and five days, respectively. The patient was instructed to perform traditional oral hygiene techniques and to utilize a 0.12% chlorhexidine gluconate-containing mouth wash (2x / day) for 15 days to allow for proper plaque control. The day after surgery (S+1), the bar and teeth were assembled, and the prosthetic restoration was attached to the implant on occlusal loading within 48 hours of the placement of the implants and abutments. After one week, the sutures were removed.
3. FOLLOW-UP ASSESSMENT
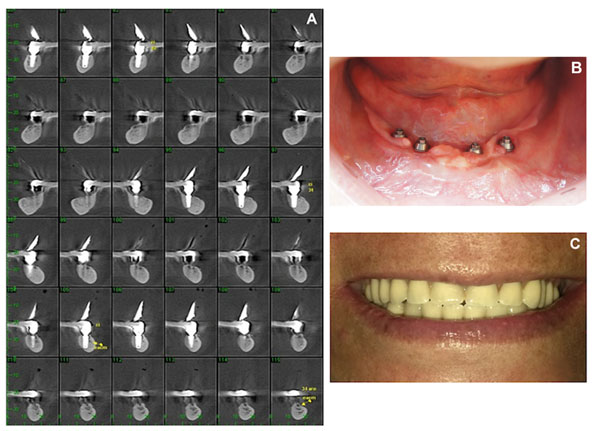
The first follow-up assessment took place at thirty days after surgery (S+30). A detailed clinical examination of the patient revealed that implants placed displayed good stability and peri-implant soft tissues did not exhibit any signs of inflammation, swelling or bleeding on probing. The patient was healthy, motivated and reported high levels of satisfaction regarding the esthetic and functional outcomes achieved with the proposed treatment. An orthopantomo- graphic assessment was then conducted to assess the bone/implant osseointegration and positioning of implant fixtures, abutments and bar, that together with the normal motor control and sensitivity of the lower lip, have indicated the attainment of initial clinical success with the oral rehabilitation strategy proposed. The patient was then enrolled in an annual oral health-care maintenance program to ensure good oral hygiene throughout the pre-determined follow-up period. The last clinical examination took place 56 months after the surgery (S+1,680), where it was possible to observe the stability of peri-implant bone levels and proper positioning of placed implants, abutments and bar (Figs. 1E and F). The cumulative overall marginal bone loss on mesial and distal aspects of the implant was 0.95 mm and 1.12 mm, respectively, which was measured using image analysis software (ImageJ®, National Institutes of Health, 1997). The maintenance of the bone crest can be observed in Figs. (1E-G). At 4 years of follow-up (Figs. 2A-2C), the patient reported high satisfaction levels in regard to the esthetics, functional and speech outcomes. The oral rehabilitation protocol proposed was shown to result in 100% survival rates for both the implants and prosthetic restoration, thereby confirming the long-term clinical success of all-on-four restorations supported by short implants in atrophic mandibule alveolar bone.
4. DISCUSSION
It has been found that bone atrophy levels tend to significantly vary in a time-dependent manner after the point at which edentulism occurs [11]. Atrophic mandibles with bone levels lower than 12.0 mm have been demonstrated to result in poor prosthetic retention, increased mobility and recurrent damage to soft-tissues, that when combined, result in mucosa hyperesthesia, subsequent loss of vertical dimension and lip support, and increased risk of maxillofacial fractures [12-15]. Oral rehabilitation techniques based on the “all-on-four” concept that was first introduced by Maló et al., [4], aimed to maximize the utilization of the available atrophic bone (especially in posterior regions) to allow for immediate functional loading and avoid the necessity for regenerative procedures (grafts, expansion, etc.) that increase not only the treatment costs associated, but also the morbidity of tissues and dental implants, which are well-known inherent complications of these types of surgical procedures [4, 6].
As reported in the present case report, one of the main concerns associated with the placement of dental implants in atrophic mandibles is mandibular fracture and possible neuronal paresthesia [15], which is concerning because the healing prognosis for patients with iatrogenic fractures of atrophic mandibles is typically not favorable due to insufficient blood supply in the affected region. This significantly increases the morbidity of implants placed (of regular length) and further prevents the oral rehabilitation techniques available to clinicians [16, 17]. Even though previous studies have demonstrated that implant length does not attenuate the transmission of forces to the mandibular bone [18], other studies have suggested that implant diameter and length should be considered since both dimensions may affect that distribution of forces transmitted by the implant to the mandibular bone [19]. In this direction, studies investigating the longitudinal and radial distribution of forces on implant fixtures have demonstrated that implant diameter tends to have a stronger influence on the distribution of forces and that the peri-implant bone crest is subjected to higher mechanical loads when compared to the apical peri-implant areas [20].
In this context, it becomes obvious that when bone-related limitations (insufficient bone height and volume) are present, short implants should be considered during the step of treatment-planning and selection of proper oral rehabilitation strategy, to prevent the occurrence of iatrogenic mandibular fracture in patients with atrophic mandibles. Short implants were found to be associated with more favorable treatment prognosis and superior levels of patient satisfaction, and therefore, may be considered as a viable alternative to the utilization of regular length implants and vertical ridge augmentation techniques [21-23]. The survival rates reported in the present study are corroborated by the findings reported in a recently published systematic review of the literature that indicated that short implants are associated with survival rates of 99.8% for follow-up periods [3] 24 months. Compelling evidence has demonstrated that short implants are typically used in posterior regions of the mandibule with the objective to avoid damage (i.e., sensorineural) to the inferior alveolar nerve [22-25], and in posterior regions of the maxilla to prevent sinus perforation [22]. Furthermore, the placement of short implants represents an important treatment option for elderly patients displaying comorbidities, thereby preventing the need for advanced surgical procedures (i.e., bone graft) prior to implant-based oral rehabilitation techniques [9, 22-25]. Since there is no consensus in the literature regarding the definition of short implants, the present case report, has defined short implants as those that follow the dimensions described on a recent paper published at the 11th European Consensus Conference [26], which considered short implants as those displaying intraosseous lengths equal to or smaller than 8.0 mm.
In a retrospective clinical study, Maló et al., [4], reported the utilization of short morse tapered implants (3.5 mm x 7.0 mm) placed in both the maxilla and mandibula and reported survival rates of 96% over 5-year follow-up period [27]. The authors suggested that short implants are a viable option because they are associated with comparable survival rates to those of traditional implants. In the present study, the clinical survival rates for the implants and prosthesis were both 100%. Moreover, at S+1,680 the marginal bone height was observed to remain constant after the functional loading of the short implants placed. Studies investigating the minimum torque levels during implant placement and the establishment of primary stability, have suggested that values ranging between 30-50 N are acceptable for immediate functional loading techniques [28-30], which corroborate the protocol herein proposed once the implants were placed with a final torque of 45 Ncm.
CONCLUSION
The utilization of the all-on-four protocol with immediate loading and short implants in an atrophic mandible was shown to be a viable alternative option to treat patients with extremely resorbed alveolar ridges. The treatment proposed displayed relevant clinical results even after a four-year follow-up period; however, longitudinal clinical trials with long-term follow-up assessments are needed to further substantiate the utilization of the oral rehabilitation protocol described in the present case report.
LIST OF ABBREVIATIONS
| CT | = Computerized Tomography |
| Ncm | = Newton centimeter |
| mm | = Millimeter |
AUTHOR CONTRIBUTIONS
Conceptualization and writing
Enéias Carpejani Rosa
Data Curation
Tuanny Carvalho de Lima do Nascimento
Investigation and Methodology
Aline Monise Sebastiani, Rafaela Scariot, Tatiana Miranda Deliberador
Supervision
Carmen L. Mueller Storrer, Writing – Review & Editing: João Cezar Zielak and Fernando Luis Esteban Florez
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient prior to being enrolled in the study.
CONFILICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to especially thank the most valuable contributions provided by Drs. Celso Yamashita and Flavia Sukekava.


