All published articles of this journal are available on ScienceDirect.
Bond Strength of Repaired Acrylic Denture Teeth Using Visible Light Cure Composite Resin
Abstract
Background:
Although bonding to denture teeth after surface treatment with chemical agents is desirable, there is little information on the use of Visible Light Cure composite resin (VLC) as bonding denture materials.
Objectives:
To determine the effect of various surface treatments on shear bond strength between Visible Light Cure composite resin and the acrylic denture teeth interface.
Methods:
Forty cylindrical sticks of acrylic resin with denture teeth mounted atop were prepared. Various treatments were implemented upon the acrylic resin teeth surfaces. The samples were divided into four groups (n = 10). Light-cured composite resin (LC) was applied over all treated and untreated surfaces of tested groups. The shear bond was tested using a universal tensile testing apparatus with the knife-edge of a 0.8mm shear tester. Data were statistically analyzed using one-way ANOVA performed at a confidence level of 95% and significant P-value of (P ≤ 0.05).
Results:
Analysis of variance (ANOVA) showed statistically significant difference (P < 0.05) between treated and untreated teeth surfaces. The treated surfaces exhibited various levels of bond strength depending on the type of treatment.
Conclusion:
Application of VLC bonding agent with prior treatment of methylmethacrylate (MMA) on the acrylic resin denture teeth resulted in maximum bond strength with composite resin.
1. INTRODUCTION
Acrylic artificial teeth are most commonly used to fabricate complete and partial dentures. This might be related to the chemical bond to denture materials and its ease of adjustment [1-4]. The combination of the acrylic artificial teeth were bonded to acrylic base using polymethylmethacrylate (PMMA) which is copolymerized with cross bonding substance. Cross-bonding material may be used in high proportion to restrict fracturing of acrylic teeth. Good chemical bonding is usually achieved between acrylic teeth and denture base materials; however, separation may occur, as can fracturing of the teeth. This may result due to traces of wax remaining on the ridge laps of the teeth, or to careless application of separating moulding medium during processing procedures [5, 6]. Such fractured teeth could be repaired with composite materials [3, 7], and visible light-cured composites [8, 9].
Visible light cured composite (VLC) have become used widely for many restorative applications because of the improvement in the wear properties, especially with new materials [10]. VLC composite resins could be used to replace fractured or deboned denture teeth [11]; this may eliminate the need for alternative time-consuming procedures. In addition, it is used to substitute broken or lost denture teeth [7], esthetic modification of artificial teeth to be harmonized with the characteristics of adjacent natural teeth [12], and remodeling of abraded anatomical tooth surfaces of masticatory artificial teeth [3, 13]. The success of such procedures may also depend on the adhesion of composites to acrylic resin [14, 15]. There are limited studies in the literature review with fewer references in journals related to the light-cured composite resins bond to the acrylic resin [16, 17]. Few studies reported the thickness of composite resin as a denture repair material. However, they focused mostly on the type of surface treatment rather than composite thickness as denture teeth repaired material. Swift et al. (1992) conducted the use of composite thickness of 2.5mm as a simple shape [18]. On the other hand, 4mm thickness of composite resin was used to bond cold-cured acrylic resins to acrylic denture teeth. This applied as two increments, each of approximate 2mm depth. Yet, 1 to 1.5mm approximate depth of the bonding region on to the acrylic resin teeth was noticed. Different bonding behavior may be observed in other regions of the acrylic resin teeth, this may depend on the extent of cross-linking of the resin molecules and the structural layering of the resin [16]. One study by Caswell and Norling (1986) detected such bonding differentiation for certain brands of denture teeth [19]. Therefore, the aim of this project is to estimate the shear bond strength of the composite resin to acrylic denture teeth after different surface treatment. The denture teeth surfaces that are treated by different methods could affect the bond strength to VLC composite resin.
2. MATERIALS AND METHODOLOGY
2.1. Mould and Denture Teeth Preparation
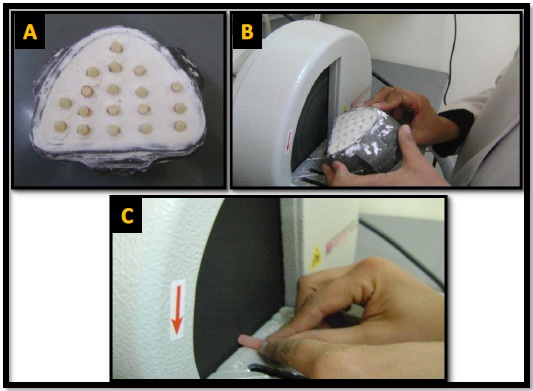
Lateral incisor acrylic resin teeth (SDT-S, China) were used in this study (Fig. 1), and embedded in a cylinder [20] of heat-cured acrylic resin (Pigeon dental, China) (Fig. 2). Each denture tooth ground from a projecting labial surface to be flat to approximately 0.5mm depth to the acrylic cylinder (Fig. 3). 600-grit silicon carbide paper was used to flattening the tested tooth surface [4]. Samples were ultrasonically cleaned 3 times in deionised water (each wash 10 minutes). This was done to simulate the denture teeth that have been in the mouth and were saturated with water; the specimens were stored in incubator with distilled water bath at 37 °C for 30 days (Fig. 4). Keeping the tested denture teeth specimens for bond strength in distilled water is the most commonly used environment to simulate the mouth [16, 18, 19]. Then the surfaces of the grounded acrylic resin teeth and acrylic resin cylinders were uniformly roughened using a trimmer machine at speed of 400 rpm for 20 seconds (Fig. 5).




2.2. Sample Treatment
All the specimens were treated with a layer of light-cured composite resin of 0.5mm thickness (Tetric®N, Ivoclar, Vivadent, Germany), and an adhesive VLC bonding agent was also used to treat surfaces of some groups (Swiss Tech SL, Swaziland). The space of 0.5mm thickness for light-cure composite material was standardized using the mould index technique. Light curing was applied for 40 seconds according to the manufacturer’s recommendation using a light curing unit (Ivoclar, Vivadent, Astralis3, Germany). In addition, autopolymerized MMA (Pigeon dental, China) was applied for 3 minutes to some treated surfaces. After treatment, all the specimens were stored in distilled water for 7 days at 37 °C before starting the testing procedure
2.3. Sample Grouping
The samples (n = 10) were divided into the four groups:
Group (A): denture teeth were repaired with light-cure composite filling material cured for 40 sec without any surface treatment.
Group (B): denture teeth bonding surfaces were treated with cold-cured methylmethacrylate liquid (monomer) for 3 minutes and then repaired with light-cure composite filling material for 40 sec.
Group (C): denture teeth bonding surfaces treated with adhesive bonding agent for 40 sec, and then repaired with light-cure composite filling material cured for 40 sec.
Group (D): denture teeth surfaces treated with cold-cured liquid monomer for 3 minutes, cured with adhesive agent for 40 sec, and then repaired with light-cure composite filling material cured for 40 sec.
2.4. Shear Bond Testing Procedure
The shear bonding was calculated using a Universal tensile testing machine (Instron, England) and a knife-edge shear testing apparatus. The entire samples were tested at room temperature using the same apparatus and at the same day. They were dried before being mounted on the testing parts. Each specimen was secured in a flat position with assistance of a clamp aligned metallic jig. The cross head loading force was applied parallel to the tooth-composite interface until fracture [20]. A metallic blade of 0.8mm edge width was moved perpendicularly at a cross-head speed of 1.5 mm per minute to rupture the surfaces at the tooth-composite interface, and the fracture loads were recorded in MPa.
3. RESULTS
The statistical methods used to analyze the results included analysis of variation (ANOVA) and Tukey (HSD). The test performed at a confidence level of 95% and significant P-value of (P ≤ 0.05). The mean value of the shear bond strengths and standard deviations for the tested groups are illustrated in Fig. (6) and Table 1. Statistically there was significant differences in shear bond strength value (P < 0.05) among treated denture teeth surfaces compared to the untreated surfaces when repaired using light-cured composite filling materials.

| Groups | *P-Value | Sig | |
|---|---|---|---|
| (A) Untreated | (B) MMA-treated | .003 | Sig |
| (C) Adhesive-treated | .001 | Sig | |
| (D) MMA-adhesive treated | .000 | Sig | |
| (B) MMA-treated | (C) Adhesive-treated | .995 | Non-Sig |
| (D) MMA-adhesive treated | .253 | Non-Sig | |
| (C) Adhesive-treated | (D) MMA-adhesive treated | .371 | Non-Sig |
4. DISCUSSION
Using VLC composite resins to replace fractured or debonded denture teeth could eliminate the time consuming in conventional procedures. To achieve superior bonding between acrylic resin and composite resin, it is important that a proper bond subsists between these two resin surfaces. Artificial denture teeth are mainly consisting of Polymethyl methacrylate (PMMA) and Polyethyl methacrylate (PEMA). Due to the manufacturer hot processing or cross-linking methods, the level of alteration is relatively high in these materials [15].
Formerly, surface treatments for acrylic resins have been grouped either as polymerizable solvents such as MMA [5, 21-26], or non-polymerizable, such as methylene chloride [27], chloroform [25], ethyl acetate [28] and 4-META [21]. Methyl methacrylate (MMA) seems to encourage the swelling of acrylic resin polymer and monomer and enhance the diffusion within the acrylic resin mass [29]. It has been suggested by Vergani et al. [17] that using MMA to wet heat polymerized acrylic resin surfaces for 3min will dissolve the surface structure of polymethylmethacrylate (PMMA), and increase the bond of restored heat-cured resin. This may provide free double bonds which copolymerize with the composite material. The polymerization processes of MMA and composite medium follow a comparable model of activation and cross-bonding. This is due to the molecules similarity reactive of the methacrylate groups. A number of chemical bondings occur in between composite and acrylic resin if cross-links are supplied on the artificial teeth for bonding to the composite. Nevertheless, in the present study, the mean bond strength value of Group D (45±8 MPa) (MMA-adhesive agent treated) was greater than that of Group A (22±5 MPa) (untreated), and Group C (38±9 MPa) (bonding agent–treated). The findings of the present study showed that the application of MMA to soften the acrylic denture teeth provided adequate active sites to react with composite resin. In restorative dentistry bonding agent such as pure and unfilled resin has long been applied with composite resin on account of the poor wettability properties of high viscosity composites [2, 5, 22]. The infiltration of the resin into microscopic surface irregularities could improve the surface wettability of the bonded surfaces. Guzman and Moore stated that a bonding agent was necessary for the achievement of satisfactory bond strength between heat-cured and light-polymerized resin [30]. Previous studies suggested in regard to bond strength between composite resin and acrylic resin denture teeth that the use of adhesive produced a superior bond compared to use of MMA only [17, 31]. This was exhibited clearly in Group C, where samples treated with bonding agent showed greater shear bond than those in Group B (37±12 MPa) (MMA-treated). The use of bonding agent (Group C) as surface treatment was more effective than monomer treated (Group B); however, neither Group B nor Group C was as effective as Group D. The surfaces treated with both MMA and bonding agent, as shown in Group D results had superior bond strength to other tested groups. Since the surfaces in this group were prepared with MMA, the adhesive-monomer liquid combination appears to exhibit superior linking. This may be produced by the dispersion and polymerization of MMA crossways the acrylic tooth-composite resin interface to form inter-penetrating polymer set of connections [15]. This proposes that higher mean bond strengths value could be achieved as a result of using adhesive bonding agent.
CONCLUSION
It seems that different surface treatments for acrylic denture teeth could influence the shear bond strength in between acrylic resin artificial teeth and composite resin as a repairing material.
The outcome of the current in vitro study pointed out the advantages of bonding agent in supporting adhesion in between composite and acrylic resin artificial teeth in combination with MMA surface treatment.
Although the present experimental technique does not imitate the intraoral situation, this may provide effective means of comparison. Many factors could be responsible for bond degradation in the oral environment and this cannot be simulated exactly in experimental conditions. This in vitro study may limit the prediction toward the success of a material or technique in clinical application. Therefore, the future studies should address the current study limitations. These represented by the use of simple shaped specimen rather than a complex denture design, and the absence of their shelf life in saliva storage or thermo-cycling environments.
CONFLICT OF INTEREST
The author confirms that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


