All published articles of this journal are available on ScienceDirect.
The Effect of Chin-cup Therapy in Class III Malocclusion: A Systematic Review
Abstract
Background:
The treatment of Class III malocclusion has been challenging for orthodontists. Among a plethora of treatment modalities, the chin-cup is considered a traditional appliance for early orthopedic intervention.
Objective:
The present study aims to investigate the current scientific evidence regarding the effectiveness of chin-cup therapy in Class III malocclusion of prognathic growing patients.
Method:
A systematic review of the literature was conducted using PubMed/Medline and the Cochrane Central Register of Controlled Trials from January 1954 to October 2015. Articles were selected based on established inclusion/ exclusion criteria.
Results:
The search strategy resulted in 3285 articles.14 studies were selected for the final analysis. They were all CCTs, 13 of retrospective and 1 of prospective design. Methodological quality was evaluated by a risk of bias assessment, as suggested by the Cochrane Risk of Bias Assessment Tool for Non-Randomized Studies on Interventions. The reported evidence presented favorable short-term outcomes both in hard and soft tissues improving the Class III profile, as well as desirable dento-alveolar changes, positively affecting the Class III malocclusion.
Conclusion:
There is considerable agreement between studies that chin-cup therapy can be considered for the short-term treatment of growing patients with Class III malocclusion, as indicated by favorable changes both in the hard and soft tissues. The existence of considerable risk of bias in all selected studies and the unclear long-term effectiveness of chin-cup therapy highlight the need for further investigation to draw reliable conclusions.
INTRODUCTION
Skeletal Class III malocclusion is clinically presented as a result of maxillary retrusion, mandibular protrusion or a combination of the two [1-3]. It is often associated with complex dento-alveolar problems, which include an anterior edge-to-edge relation or anterior and/or posterior crossbite [4]. Patients with Class III malocclusion exhibit potential esthetic problems presenting a concave profile, and a vertical function pattern [3, 4], which limits their function to vertical movements.
The prevalence of Class III malocclusion presents a wide variety among and within populations [5, 6], as declared by a high 23% rate in Asian populations contrasted to a smaller 5% rate in Caucasians [1, 7]. Treatment of Class III malocclusion has been a challenge for orthodontists [1]. Among various treatment modalities, the chin-cup is considered a traditional appliance for the early orthopedic management of prognathic growing patients [2, 8-11]. Its clinical effectiveness has been investigated over the years with many studies confirming a general improvement of Class III malocclusion through backward and downward mandibular rotation, retardation of mandibular growth, remodeling of the mandible and the temporomandibular joint (TMJ), retroclination of mandibular incisors and closing of the gonial angle [1, 2, 7, 10, 11].
Despite the plethora of the available evidence, clinical results achieved with the chin-cup constitute a controversial issue among researchers. Owing to the absence of a standard protocol concerning the chin-cup’s appropriate use and the contradicting results of the reported outcomes and outcomes measures, a clear interpretation of data is not possible [1, 2, 7,12]. Although a great number of studies focus on the skeletal and dento-alveolar changes [2, 7, 10-12], the effects of chin-cup therapy on facial soft tissues remain uninvestigated. Furthermore, the vast majority of studies report outcomes of the chin-cup use obtained over a short-term period [2, 7, 10, 12], while there is a lack of studies examining the long-term effectiveness of chin-cup therapy.
For the aforementioned reasons the purpose of the present systematic review is the investigation of the short- and long-term effects on both the hard and soft tissues induced by chin-cup therapy in the Class III malocclusion of growing patients, based on the existing scientific evidence.
MATERIALS AND METHODOLOGY
Type of Participants
Prognathic growing patients (pre-pubertal, pubertal) with Class III malocclusion receiving chin-cup therapy for the improvement of their skeletal, dento-alveolar and facial characteristics.
Type of Interventions
Chin-cups. (Potential confounders and co-interventions were specified and taken into account).
-Secondary: Short and long-term effectiveness of chin-cup therapy, if provided, in order to assess the stability of the results.
All reported time-points after the completion of the treatment, judged by the authors of the trials were included. The short-term effectiveness is related to the outcomes obtained upon the end of the active treatment with chin-cup therapy, while the long-term effectiveness is related to the ones obtained at a post-treatment observation after the end of the active treatment.
Search Strategy
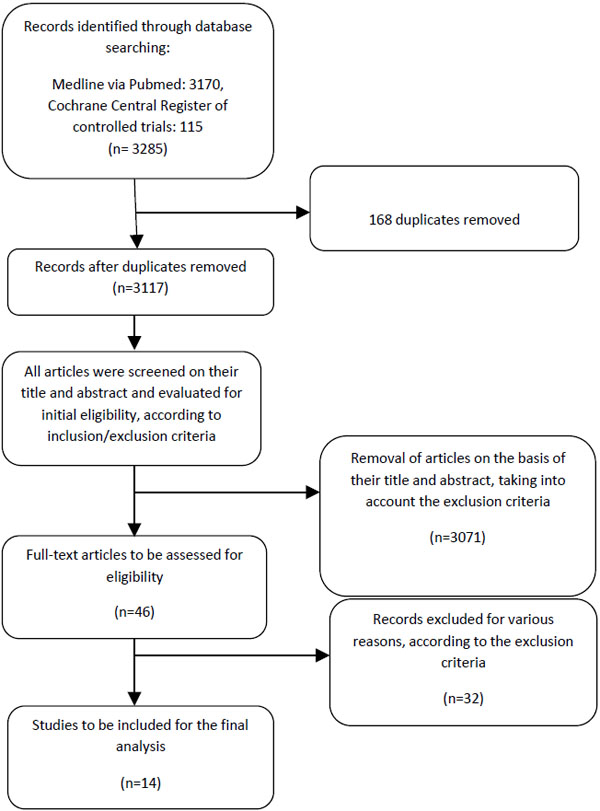
A literature search was carried out by applying the Medline database (PubMed www.ncbi.nih.gov) and the Cochrane Central Register of Controlled Trials covering the period from January 1954 to October 2015 and using the following Medical Subject Heading (MeSH) terms; “Malocclusion, Angle Class III”, “chin-cup therapy”, “chincap therapy”, (Table 1). A schematic representation of the search strategy is shown in Fig. (1).
| MeSH Terms | Articles Retrieved |
|---|---|
| “Malocclusion, Angle Class III” | 3208 articles |
| “Chin-cup therapy” | 53 articles |
| “Chincap therapy” | 24 articles |
Selection Criteria
Articles selected for this study fulfilled the criteria for inclusion, (Table 2). The criteria included randomized clinical trials (RCTs), prospective and retrospective clinical trials (CCTs) with untreated control groups. The retrieved studies had to use cephalometrics for analyzing the effects of chin-cup therapy contrasted to untreated Class III control groups. Table 2 also presents in detail the exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 1. Articles published from January 1954 to October 2015 | 1. Reviews and Meta-analysis |
| 2. RCTs | 2. Case reports/case series |
| 3. Prospective-Retrospective CCTs | 3. Studies on adults |
| 4. Studies on growing patients | 4. Treatment combined with extractions |
| 5. Studies based on lateral cephalograms | 5. Treatment combined with surgery |
| 6. Articles in English | 6. Studies about the relationship between Class III and TMJ disorders |
| 7. Laboratory studies | |
| 8. Commentary/Opinion articles | |
| 9. Abstracts | |
| 10. Articles, whose objective is out of the scope of interest of the present study |
Data Extraction
Two independent reviewers (SM, EF) made the assessment of the articles individually in predefined data extraction forms. No blinding to the authors during data extraction was made and any inter-examiner conflicts were resolved by discussion with a third reviewer (IT). The same reviewers performed the risk of bias assessment of the articles, with one author (AT) acting as the coordinator.
Quality Analysis
For the qualitative evaluation of the retrieved studies the risk of bias was assessed by two reviewers (SM, EF) independently. The assessment was based on the following tool: A Cochrane Risk of Bias Assessment Tool for Non-Randomized Studies on Interventions (ACROBAT-NRSI) [13]. This tool addresses seven domains of bias; bias due to confounding, bias in selection of participants into the study, bias in measurement of interventions, bias due to departures from intended intervention, bias due to missing data, bias in measurement of outcomes and bias in selection of the reported result.
Important confounders with regard to chin-cup therapy were considered those that could have an impact on the reported results. Thus, the following confounders were taken into account both for patients and controls: ethnicity (as Asian populations have a higher prevalence of Class III malocclusion) [1, 7,14-16], age in relation to the skeletal maturity stage, pre-treatment skeletal Class of malocclusion (when it was not skeletal Class III both for patients and controls), soft-tissue profile individual variation in thickness and in tension, and pre-treatment overjet. Moreover, co-interventions were considered the use of additional appliances, such as an occlusal bite plate, a quad-helix appliance, a lingual arch, etc., and the utilization of force magnitude of the chin-cup traction.
Three different outcomes were investigated; skeletal, dento-alveolar and soft-tissue effects of chin-cup therapy in Class III malocclusion both in the short- and in the long-term. For every different outcome of each study an initial risk of bias for every domain was assessed, as indicated by the ACROBAT-NRSI [13]. Because same issues applied to all outcomes, a grouped assessment was made. Finally, an overall risk of bias judgement for each study was achieved.
RESULTS
Our search strategy resulted in 3285 articles. After selection, according to the inclusion/exclusion criteria (Table 2), 46 studies were gathered and read in full-text. Finally, 14 studies were retrieved for the final analysis. The remaining 32 articles were excluded, mainly, because there were no untreated controls or the controls were not skeletal Class III patients, the treatment was combined with extractions or surgery and their objective was out of the scope of interest of the present study. Table 3 summarizes the data of the 14 included studies.
Clinical heterogeneity among studies (different outcome assessment, variable age of patients and different follow-up duration), and the high risk of bias in general precluded the quantitative synthesis of results in a meta-analysis.
Skeletal Effects
The majority of the studies showed a general improvement of skeletal Class III malocclusion, through increased ANB [17-22], Wits appraisal [17, 22] and decreased SNB [17-22], SNPg [23]. Moreover, the anterior facial height [17, 18, 22, 24], the mandibular plane angle (SN-MP) [18-20, 22] and the FMA [23] were significantly increased, whereas the gonial angle [20, 23, 25, 26] was significantly decreased, indicating a tendency towards a backward and downward rotation of the mandible induced by the chin-cup. Furthermore, restraint of the mandibular length was pointed out in five studies [23, 25-28] by significant decreases in mandibular body length [23, 27], total mandibular length [23, 26-28] and anteroposterior compression of the distance between the condyle and the coronoid process [25]. Significant reduction of the ramus height was also noted [22, 23, 25, 27]. With regard to the skeletal changes in the cranial base and the midface, two studies [8, 27] reported significant closure of the cranial flexure angle (N-S-Ba), indicating inhibition of the downward vertical growth of the midface [8] and less downward mandibular displacement relative to the cranial base [27].
|
aArticle- Authors- Y.o.p |
Study design | Participants (number-age- gender) | Intervention | Treatment’s duration | Observational period | Outcomes | Method of Outcome Assessment | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| Ritucci-Nanda[8], 1986 | retrospective | 10 F treated; 7F untreated (age not reported) |
10 CC; 7 untreated | Not reported | From age of 5y until the beginning of pubertal growth spurt. | Effects on growth and development of the cranial base and midface produced by the CC. | Lateral cephalometric radiographs (semiannually for treated patients; annually for controls) and menarche data (to assess the skeletal maturity stage). | Significantly decreased N-S-Ba angle, imposed downward vertical growth of the midface and Mx incisors’ eruption rate. More horizontal displacement of Mx 1st molars. | Closure of cranial flexure angle, inhibition of the downward vertical growth of the midface (posteriorly more evident). No effect on anteroposterior dimension. Increased mesial Mx molars’ movement. No soft-tissue changes reported. |
| Alacrόn et al.[25], 2011 | retrospective | 50 (25M,25F) treated, (8.5 ± 0.5 y); 40 (20M,20F) untreated (8.6 ± 0.4 y) |
50 CC; 40 untreated | 36m | Until the end of the treatment. | Mandibular shape changes in prognathic children treated with CC. | Lateral cephalometric radiographs + geometric morphometric analysis. | More rectangular corpus-ramus relationship, anteroposterior compression of the distance between the condyle and the coronoid process- relative vertical posterior ramus and gonial area compression, decreased gonial angle, increased symphysis height and narrowing. | Wide modification of the mandibular shape (more rectangular Mn configuration, forward condyle orientation, gonial area compression and symphysis narrowing. |
| Arman et al.[17], 2004 | retrospective | group 1: 31 (9M; 22F), 11.0 ± 0.24 y; group 2: 14 (8M; 6F), 11.1 ± 0.49 y, group 3: 14 (3M; 11F), 11.6 ± 0.61 y and 20 untreated controls (gender not reported), 10.5 ± 0.24 y. |
group 1: CC, group 2: CC+OBP, group 3: RHG; 20 controls. | group 1: 1.0 ± 0.15 y, group 2: 1.2 ± 0.15 y, group 3: 0.9 ± 0.09 y | Until the end of treatment for the treated groups; 1.0 ± 0.09 y for controls. | Skeletal, dentoalveolar and soft-tissue changes of CC, CC+OBP, RHG. Comparison of the treated groups with untreated controls and with each other. | Lateral cephalometric and hand-wrist radiographs. | Significant changes: decreased SNB, increased ANB, Wits appraisal, facial convexity angle (NAPg) and anteroposterior facial heights, increased overjet and decreased overbite, Mx incisors’ protrusion (U1i-HR) and proclination (U1- HR), Mn incisors’ retrusion (L1I-VR) and retroclination (L1-HR) and vertical movement (L1i-HR). Significant A(S)+upper lip’s forward movement (A(S)-VR, UL-VR), lower lip’s retraction (LL-VR, LL- E Ricketts, backward movement of B(S) (B(S)-VR) and backward position of soft chin (Pg(S)-VR). | Significant dentoskeletal improvements of skeletal Class III growing patients. More evident soft-tissue changes in the CC group. Long-term evaluation of stability is required. |
| Wendell et al.[27], 1985. | retrospective | 10F (age range: 5y 4m - 15y 6m; 7F (age range: 6y – 15y. | 10 CC; 7 untreated. | mean time: 3y 1m (until the correction of Class III Malocclusion). | Variable for treated patients (not specified). 6y 2m for the controls. | Effects of CC therapy on mandibular growth and dentition studied in young Japanese females. | Lateral cephalometric radiographs (semi-annually for the treated patients, annually for the controls. | 60-68% significant reduction of the ramal length (Ar-Go), body length (Go-Pg), and total Mn length (Ar-Pg). Continued reduction after the end of active treatment (55-61%). Significant closure of the N-S-Ba angle and significant decreases in anterior facial height (N-Me) during treatment. 50% further sign. anterior displacement of the 1st molars (M6x) during and 90% after the active treatment. | Significant reduction of the absolute Mn length during and after the end of the active treatment. Less downward Mn displacement relative to the cranial base. Significant dental changes declaring a favourable migratory dental displacement into Class I occlusion. |
| Alacrόn et al.[28], 2015 | retrospective | 42 (21M,21F), 8.5 ± 0.5 y; 25 (12M,13F), 8.5 ± 0.5 y. |
42 CC; 25 untreated. | 36 ± 6 m. | Until the age of 11 ± 0.6 y on average for the treated patients; Until the age of 11 ± 0.5 y on average for controls. | Soft-tissue changes in association to any skeletal and dentoalveolar changes induced by CC. | Lateral cephalometric radiographs. | Significant changes: inhibition of the sagittal growth of the mandible and the Mn incisors’ alveolus (B-GD, Pg-GD, Id-GD), inhibition of the total Mn length (Co-Pg), decreased facial convexity angle, lower lip’s inclination (Linf-E Ricketts), upper lip thickness, upper lip protrusion (Lsup-E Ricketts). Similar correlations of changes both in the hard+soft tissues apart from that one between the Pg retrusion and the reduction in the facial convexity angle. | Short-term soft facial profile improvement by favourable soft-tissue alterations following the underlying skeletal and dentoalveolar changes except for a significant correlation of Pogonion retrusion and reduction in the facial convexity angle. |
| Tuncer et al.[18], 2009 | retrospective | 20 (10M, 10F) 10.31 ± 1.15 y; 18 (10M, 8F) 9.89 ± 1.55 y. |
20 CC + OBP; 18 untreated |
9.78 ± 0.93 y. | Until the end of the treatment for the treated patients; 11.14 ± 0.24 y for the untreated controls. | Examination of the sagittal pharyngeal dimensions after CCtherapy. | Lateral cephalometric and hand-wrist radiographs. | Significant changes: decreased SNB and increased Sn-GoGn angles, increased total (N-Me) and upper heights. increased nasopharyngeal area and downward movement of the hyoid bone (H-SN). | Short-term downward and backward rotation of the mandible, increased vertical height, increased nasopharyngeal airway area. |
| Gökalp and Kurt [29], 2005. | prospective | 13 (3M,10F), 9.06y; 7 (1M,6F) 8.90y. |
13 CC; 7 untreated |
1y 7m. | Until the end of the treatment. | Investigation of skeletal Class III improvement after CC therapy. | Lateral cephalometric radiographs and Magnetic resonance imaging. | Significantly increased Mn body length and overjet. | CC alters the condylar growth pattern by producing morphological changes of the TMJ components and remodelling of the mandible towards an improved skeletal Class III malocclusion. |
| Sakamoto et al.[23], 1984. | retrospective | 26F, (age range: 6-9 y). 1F from the treated group was cross-sectionally contrasted to 423F (age range: 3-30y) to illustrate the reported skeletal changes induced by CC. |
26 CC (+additional double spring lingual arch in some cases). 423 untreated. |
Not reported. | More than 2 y after the end of CC therapy. | Skeletal changes and post-treatment stability after CC therapy. | Lateral cephalometric radiographs. | During treatment: decreased SNPg, increased ANB, FMA angles, restraint of growth (Mn body, ramus, Mn length, facial length), decreased gonial angle. 1y after the removal of CC: Forward Mn displacement (increased SNPg, decreased ANPg angles). 2 y after the removal of CC: no changes not maintained. | Restraint of growth was noted during CC therapy, but relapsed after the end of the treatment. No obvious changes in the cranium and the maxilla. Similar growth in Mn increments before and after the removal of CC. |
| Deguchi and McNamara [26], 1999. | retrospective | 22F, 9y 4m; 20F, 9y 7m. |
22 CC (+ additional lingual arch to flare the upper incisors); 20 untreated. | 1y 9m. | 28 ± 7.9 m for the treated patients; 30 ± 12m for the controls. | Investigation of the orthopedic effect of CC in the posterior displacement of the mandible and the glenoid fossa. | Lateral cephalometric and hand-wrist radiographs. | Significantly decreased gonial angle, less incremental increase in Mn length (Gn-Cd), posterior movement of points B and Pg, not increased anterior facial height. | Reduction in Mn growth increments. |
| Akin et al.[19], 2015. | retrospective | 25 (9M,16F), 9.8 ± 1.6 y, 25 (10M,15F), 10.3 ± 1.5 y; 17 (8M,9F), 10.1 ± 1.3 y. |
25 CC + OBP (flat surface Essix plate); 25 facemask; 17 untreated. |
Not reported. | Until the end of the treatment for the treated patients; 6m for the untreated. | Orofacial airway dimensional effects of facemask or CC compared to untreated controls. | Lateral cephalometric and hand-wrist radiographs. | Significant changes: decreased SNB, increased ANB and Sn-GoGn angles, forward movement and proclination of Mx incisors (increased U1-NA), backward movement and retroclination of Mn incisors (L1-NB), increased UL-E Ricketts, indicating protrusion of the upper lip. Changes in the perpendicular distance from hyoid (H) to the C3-Me line compared to controls. | CC therapy is found to induce clockwise Mn rotation. Although it does not significantly affect the pharyngeal airway dimensions, it moves the hyoid bone to a more inferior position in comparison with both the facemask and the untreated patients groups. |
| Lin et al.[20], 2007. | retrospective | 20 (10M,10F), 9y 11m; 20 (10M,10F) 9y 6m. |
20 OMA; 20 untreated. |
1y 4m. | Until the end of the treatment for the treated patients; 1y 5m for the untreated. | Skeletal and dental changes induced by an orthopedic OMA. | Lateral cephalometric radiographs. | Significant changes: Forward movement of point A, increase in Mx length, increased SNA, horizontal change of point B, increase in the Mn plane (Sn-MP) and the ramus plane angles, decreased SNB and gonial angles, labial tipping of Mx incisors, horizontal change in the Mn incisors’ tip, increased overjet. | OMA induces short-term favourable skeletal (forward growth of the Mx complex, backward and downward rotation of the Mn, restraint in forward Mn advancement) and dentoalveolar effects (labial tipping of Mx incisors). |
| Barrett et al.[21], 2010. | retrospective | 26 (11M,15F), 8.5 y treated patients divided in: group 1: 12 patients; group 2: 14 patients; 20 (6M,14F), 7.3y untreated. |
group 1: 12 CC + QH; group 2: 14 CC only; 20 untreated. |
2.6 y for the CC, 2..4 y for controls. | Until the end of treatment. | Skeletal and dentoalveolar changes induced by CC. | Lateral cephalometric radiographs. | Significant changes: a) skeletal: decreased SNB, increased ANB, decrease in palatal plane angle (FH-PP), b) dentoalveolar: uprighting of Mn incisors (decreased IMPA), decreased L1-APg and L1 horizontal movement, increased overjet, c) soft-tissue: decreased LL-E Ricketts and increased nasolabial angle. | Limited Class III correction with light force CC (fewer than 50% of the patients) mostly by dentoalveolar (uprighting of Mn incisors) rather than orthopedic changes. |
| Abu Alhaija and Richardson [24], 1999. | retrospective | 23 (14M,9F), 8.11 ± 0.96 y; 23 matched (age not reported). |
23 CC+URA; 23 untreated. |
3.01 ± 1.61 y | 3.34 ± 1.80 y after the end of treatment; 4.12 ± 1.86 y for the untreated. |
Short-and long-term effects of CC therapy combined with an URA in Class III patients. | Lateral cephalometric radiographs. | Significant changes: a) at the end of the active treatment: increased Mn length and facial height, retroclination of lower and proclination of upper incisors, increased overjet, nasolabial angle and improvement of soft-tissue profile, b) post-treatment: further Mn growth (increased SNB, Wits appraisal), increased facial height, maintained overjet, forward movement of the upper- and the lower lip, forward inferior movement of the chin. | Long-term proclination of the upper incisors, retroclination of the lower incisors, downward redirection of Mn growth and soft-tissue profile improvement. |
| Abdelanby and Nassar [22], 2010. | retrospective | group 1: 20 (10M,10F), 9.6y; group 2: 20 (9M,11F), 10.1 y; group 3: 10 (5M,5F), 9.2y. |
20 CC+OBP (600 gr per side); 20 CC+OBP (300 gr per side); 10 untreated. |
1 y. | 1 y for the untreated patients. | Skeletal and dental effects of CC using 2 force magnitude (300,600 gr per side) in Class III growing patients. | Lateral cephalometric and hand-wrist radiographs. | Significantly decreased SNB, Mn ramus height (Ar-Go), increased ANB, Wits appraisal, anterior, facial height (N-Me) Mn plane angle (SN-MP) and retroclination of Mn incisors. | Limited skeletal changes irrespective of utilization of force magnitude per side except for the reduction of the ramus height. |
Dento-Alveolar Effects
The main dento-alveolar changes produced by the chin-cup were the achievement of a significant overjet [17, 20-22, 24, 29] and retroclination of the lower incisors [17, 19, 21, 22, 24]. More precisely, Ritucci and Nanda [8] declared that transition in overjet occurred with a marked degree of flaring of the maxillary incisors, followed by a variable amount of uprighting, based on lateral cephalograms. Overjet correction was, also, reported byAlacrόn et al. [25], mainly achieved by mandibular incisor retroclination. Moreover, Barrett et al. [21] noted the uprighting of the lower incisors, indicated by the decreased IMPA, as the most significant dental change between the chin-cup and the control groups. Significant proclination of the upper incisors [8, 17, 19, 20, 24] was also pointed out. However, the aforementioned results, especially those regarding the proclined upper incisors, should be carefully interpreted in order to clarify whether they constitute net effects of the chin-cup alone or the additional appliances that were used and were co-interventions.
Changes regarding overbite varied, depending on the appliance that was used. More specifically, Arman et al. [17] noted a significant decrease in overbite in all the treated groups (chin-cups only, chin-cups with removable bite plate, reverse headgear with rapid maxillary expansion devices).
Regarding the molar relationship after the active treatment, Ritucci and Nanda [8] declared that chin-cups accelerate the mesial movement of maxillary molars, without any effect on their eruption rate, while Wendell et al. [27] manifested that the initial Class III occlusion was corrected to Class I relationship in all of the patients.
Soft-Tissue Effects
The effects of chin-cup therapy on the soft tissues were reported in five studies [17, 19, 21, 24, 28]. Significant forward movement of the upper lip was declared in four studies [17, 19, 24, 28] with a concomitant forward movement of the soft-tissue point A [17], while the movement of the lower lip presented differing results. Arman et al. [17], Alacrόn et al. [28] and Barrett et al. [21] stated a decreased distance of the lower lip to E plane (LL-E Ricketts line [17, 21, 28]) and lower lip’s retraction (LL-VR [17]) with a concomitant backward movement of the soft-tissue point B [17] and the soft chin (Pg(s) [17, 28]). However, Abu Alhaija and Richardson [24] showed significant forward movement of the lower lip [24]. A general soft-tissue facial profile improvement was attributed to the chin-cup by Alacrόn et al. [28], who demonstrated similar correlations between the changes in the hard and in the soft tissues, especially the one between a significant reduction of the facial convexity angle and a significant pogonion retrusion in the chin-cup group.
Stability
Two studies [23, 24] reported information concerning the stability of treatment outcomes, using cephalometric x-rays at a post-treatment observation. Abu Alhaija and Richardson et al. [24], following a one-year post-treatment cephalometric observation, reported a significant increase in mandibular length, which was in accordance with Sakamoto et al. [23], whose study found a forward displacement of the mandible in one-year post-treatment observation and total relapse in the original mandibular growth pattern after two years. Both studies [23, 24] showed a significant increase in the anterior face height.
As for the dental effects, the significantly increased overjet achieved by chin-cups was maintained one year after the end of the treatment [24].
Although stability in the soft-tissue profile was evident at the post-treatment observation, the upper, the lower lip and the chin continued to grow forward following the skeletal pattern [24].
Quality Analysis
The overall judgement for the risk of bias was found serious for all the retrieved studies, (Table 4). All had a serious risk of bias concerning the selection of participants into the study (selection bias). Based on the ACROBAT-NRSI [13], all the studies were found to have some important problems in the corresponding domains, indicating cautious interpretation of the reported results.
DISCUSSION
In this systematic review, our primary goal was to search the existing literature for randomized and control clinical trials regarding the short- and long-term effects of chin-cup therapy on hard and soft tissues of growing patients. These had to include untreated patients as controls.
| a Authors- Article- Y.o.P. | Bias due to confounding | Bias in selection of participants into the study | Bias in measurement of interventions | Bias due to departures from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported result | Overall Judgement |
|---|---|---|---|---|---|---|---|---|
| Ritucci-Nanda[8], 1986 |
Outcomes: O1, O2. Risk: Moderate SfJ: confounding expected (pre-treatment overjet), but probably eliminated since as it was stated “the occlusion changed from one with an underjet to one with an overjet”. |
Outcomes: O1, O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2. Risk: Moderate SfJ: Intervention status is well defined, but data were determined retrospectively in a way that could have been affected by knowledge of the outcome. |
Outcomes: O1, O2. Risk: Low SfJ: No bias due to departures from intended intervention is expected. |
Outcomes: O1, O2. Risk: Low SfJ: Data were reasonably complete. |
Outcomes: O1, O2. Risk: Serious SfJ: Outcome measure was subjective, the assessor was aware of the received intervention and any systematic error in measurements was related to intervention status. |
Outcomes: O1, O2. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (selection of the participants), detection bias, measurement bias and observer bias. |
| Alacrόn et al.[25], 2011 |
Outcomes: O1, O2. Risk: Low SfJ: No confounding expected. |
Outcomes: O1, O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2. Risk: Moderate SfJ: Intervention status is well defined, but data were obtained retrospectively. |
Outcomes: O1, O2. Risk: Low SfJ: No bias due to departures from intended intervention is expected. |
Outcomes: O1, O2. Risk: Low SfJ: Data were reasonably complete. |
Outcomes: O1, O2. Risk: Low SfJ: Comparable outcome assessment methods between the 2 groups and blinded assessor to intervention status and any systematic error in measurements unrelated to intervention status. |
Outcomes: O1, O2. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has an important problem, e.g: serious risk of selection bias (selection of the participants). |
| Arman et al.[17], 2004 |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Critically important confounders (ethnicity, Skeletal Class of malocclusion and soft-tissue profile variation) not measured and not adjusted for in the analysis. |
Outcomes: O1, O2, O3. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2, O3. Risk: Serious SfJ: Intervention status may be well defined, but data were obtained retrospectively and determined in a way that could have been affected by knowledge of the outcome. |
Outcomes: O1, O2, O3. Risk: Serious SfJ: Co-interventions are apparent (OBP, RHG) and not adjusted for in the analysis. |
Outcomes: O1, O2, O3. Risk: Moderate SfJ: Reasons for missingness (for baseline characteristics and confounders) differ minimally across interventions and missing data were not addressed in the analysis. |
Outcomes: O1, O2, O3. Risk:Moderate SfJ:Comparable outcome assessment methods between the groups and outcome measure only minimally influenced by knowledge of the intervention (blinding not reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1, O2, O3. Risk: Moderate SfJ: Relative low risk of selective reporting, because all results were declared for each group in comparison with each other. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants) and performance bias. |
| Wendell et al.[27], 1985. |
Outcomes: O1, O2. Risk: Serious SfJ: Serious residual confounding, because of variation in the onset, duration and amount of the growth peaks of the patients, as well as in the onset and duration of the treatment time. Also the 2 treatment periods of patient 13 indicate time-varying confounding. |
Outcomes: O1, O2. . Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2. . Risk: Serious SfJ: Intervention status is not well defined (not explicit timing of intervention), retrospectively obtained and likely to have been influenced by knowledge of the received intervention. |
Outcomes: O1, O2. . Risk: Moderate SfJ: No co-interventions, no switches and probably minor implementation fidelity. |
Outcomes: O1, O2. . Risk: Serious SfJ: The nature of the missing data (on baseline confounders) means that the risk of bias cannot be removed through appropriate analysis. |
Outcomes: O1, O2. . Risk: Serious SfJ: Any systematic error in measurements was related to intervention status and the assessor was aware of the received intervention. |
Outcomes: O1, O2. . Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants), information bias, performance bias, detection bias, measurement bias and observer bias. |
| Alacrόn et al.[28], 2015 |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Critically important confounders (pretreatment overjet, soft tissue variation) not measured and not adjusted for in the analysis. |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Intervention status is well defined but data were obtained retrospectively. |
Outcomes: O1, O2,O3. Risk: Low SfJ: No bias due to departures from intended intervention is expected. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Reasons for missingness (for baseline confounders) differ minimally across interventions and missing data were not addressed in the analysis. |
Outcomes: O1, O2,O3. Risk: Low SfJ: Comparable methods of outcome assessment between the 2 groups, and blinded assessor to intervention status and any error in measuring the outcome unrelated to intervention status. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding and in the selection of the participants). |
| Tuncer et al.[18], 2009 |
Outcomes: O1. Risk: Serious SfJ: one critically important confounder (ethnicity) not measured and not adjusted for in the analysis. |
Outcomes: O1. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1. Risk: Moderate SfJ: Intervention status is well defined but data were obtained retrospectively. |
Outcomes: O1. Risk: Serious SfJ: Co-intervention is apparent (OBP) and not adjusted for in the analysis. |
Outcomes: O1. Risk: Moderate SfJ: Reasons for missingness (for baseline confounder) differ minimally across interventions and missing data were not addressed in the analysis. |
Outcomes: O1. Risk: Moderate SfJ: Comparable method of outcome assessment between the 2 groups, outcome measure is only minimally influenced by knowledge of intervention status and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants), information bias and performance bias. |
| Gökalp and Kurt [29], 2005. |
Outcomes: O1,O2. Risk: Serious SfJ: critically important domains (ethnicity, age, skeletal Class of malocclusion) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1,O2. Risk: Moderate SfJ: Intervention status is well defined but data were obtained retrospectively. |
Outcomes: O1,O2. Risk: Low SfJ: No bias due to departures from intended intervention is expected. |
Outcomes: O1,O2. Risk: Moderate SfJ: Reasons for missingness (missing data on baseline confounders) differ minimally across interventions and missing data were not addressed in the analysis. |
Outcomes: O1,O2. Risk: Moderate SfJ: Comparable method of outcome assessment between the 2 groups, outcome measure only minimally influenced by knowledge of intervention status and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding and in the selection of the participants). |
|
Sakamoto et al. [23], 1984. |
Outcomes: O1. Risk: Serious SfJ: one critically important domain (age) not adjusted for in the analysis (skeletal maturity stage not addressed). |
Outcomes: O1. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1. Risk: Serious SfJ: Intervention status is not well defined (skeletal maturity stage, number of patients with additional lingual arch) and major aspects of the assignments of intervention were determined in a way that could have been affected by knowledge of the outcome. |
Outcomes: O1. Risk: Serious SfJ:Co-intervention (lingual arch) is apparent and not adjusted for in the analysis. |
Outcomes: O1. Risk: Serious SfJ: Because the reported results correspond to the 26 treated patients, while the untreated control group of 423 patients is used supplementarily to illustrate the aforementioned results, judgement is basically based on the missing data regarding the treated patients (data on baseline characteristics and confounders). |
Outcomes: O1. Risk: Serious SfJ: Outcome measure likely to be influenced by knowledge of the intervention status and assessed by outcome assessors aware of the received intervention. Any error in measuring the outcomes was also related to intervention. |
Outcomes: O1. Risk: Serious SfJ: Because there is moderate risk of bias in selective reporting of the results of the study, but critical risk only for the supplementary comparison to untreated controls (1 patient compared to 423 controls). |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants),information bias, performance bias, detection bias, measurement bias and observer bias, outcome reporting bias. |
| Deguchi and McNamara [26], 1999. |
Outcomes: O1,O2 Risk: Low SfJ: No bias due to confounding is expected. |
Outcomes: O1,O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1,O2. Risk: Moderate SfJ: Intervention status is well defined, but data were retrospectively obtained. |
Outcomes: O1, O2. Risk: Serious SfJ: Co-intervention is apparent (upper lingual arch) and not adjusted for in the analysis. |
Outcomes: O1,O2. Risk: Low SfJ: Data were reasonably complete. |
Outcomes: O1,O2. Risk: Moderate SfJ: Comparable method of outcome assessment between the 2 groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1,O2. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (selection of the participants),information bias and performance bias. |
| Akin et al.[19], 2015. |
Outcomes: O1,O2,O3. Risk: Serious SfJ: Critically important domains (ethnicity, individual soft-tissue variation, pre-treatment overjet) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2,O3. Risk: Serious SfJ: Selection into the study was related to intervention (intervention was known and blinding was only performed for the selection of 15 cases for each group) and probably the outcome. |
Outcomes: O1,O2,O3. Risk: Serious SfJ:Intervention status is not well defined (not declared whether CC therapy was continued or ended by the time fixed appliances were placed and for what reason the flat Essix plate was used). |
Outcomes: O1,O2,O3. Risk: Serious SfJ: Co-interventions are apparent (flat Essix plate, possibly simultaneous use of fixed appliances) and not adjusted for in the analysis. |
Outcomes: O1,O2,O3. Risk: Moderate SfJ: Missing data (on baseline confounders) were not addressed in the analysis and reasons for missingness differ minimally across interventions. |
Outcomes: O1,O2,O3. Risk: Moderate SfJ: Comparable method of outcome assessment between the groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1,O2,O3. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants), information bias and performance bias. |
| Lin et al.[20], 2007. |
Outcomes: O1,O2 Risk: Serious SfJ: Critically important domain (ethnicity) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1,O2 Risk: Moderate SfJ: Intervention status is well defined, but data were obtained retrospectively. |
Outcomes: O1,O2 Risk: Serious SfJ: Co-intervention (OMA) is apparent and not adjusted for in the analysis.. |
Outcomes: O1,O2 Risk: Moderate SfJ: Reasons for missingness differ minimally across the 2 groups and missing data were not addressed in the analysis. |
Outcomes: O1,O2 Risk: Moderate SfJ: Comparable method of outcome assessment between the groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1,O2. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants), performance bias. |
| Barrett et al.[21], 2010. |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Critically important confounder (Skeletal Class of malocclusion) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2,O3. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Intervention status is well defined, but data were retrospectively obtained. |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Co-intervention is apparent (QH) and not adjusted for in the analysis. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Reasons for missingness differ minimally across interventions and missing data (on baseline confounder) were not addressed in the analysis. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Comparable method of outcome assessment between the groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1,O2,O3. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants) and performance bias. |
| Abu Alhaija and Richardson [24], 1999. |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Critically important confounders (ethnicity, age, Skeletal Class of malocclusion and soft-tissue variation) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2,O3. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Intervention status is well defined, but data were obtained retrospectively. |
Outcomes: O1, O2,O3. Risk: Serious SfJ: Co-intervention is apparent (URA) and not adjusted for in the analysis. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Reasons for missingness differ minimally across the 2 groups and missing data (on baseline confounders) were not addressed in the analysis. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Comparable method of outcome assessment between the groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1, O2,O3. Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants) and performance bias. |
| Abdelanby and Nassar [22], 2010. |
Outcomes: O1,O2 Risk: Serious SfJ: Critically important domain (ethnicity) not measured and not adjusted for in the analysis. |
Outcomes: O1,O2. Risk: Serious SfJ: Selection into the study was related to intervention and probably the outcome. |
Outcomes: O1,O2 Risk: Moderate SfJ: Intervention status is well defined but data were retrospectively obtained. |
Outcomes: O1,O2 Risk: Serious SfJ: Co-intervention is apparent (utilization of force magnitude) and not adjusted for in the analysis. |
Outcomes: O1,O2 Risk: Moderate SfJ: Reasons for missingness differ minimally across interventions and missing data (on baseline confounder) were not addressed in the analysis. |
Outcomes: O1,O2 Risk: Moderate SfJ: Comparable method of outcome assessment between the groups, outcome measure only minimally influenced by knowledge of intervention status (no blinding reported) and any systematic error in measurements only minimally related to intervention status. |
Outcomes: O1, O2 Risk: Moderate SfJ: Outcome measurements and analysis were clearly defined, internally and externally consistent, there was no indication of selection of the reported analysis from among multiple analyses and no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results. |
Risk: Serious SfJ: The study has some important problems, e.g: serious risk of selection bias (residual confounding, selection of the participants) and performance bias. |
a The cited references of the articles in the first column of the table correspond to the numbered references in the text.Y.o.P: indicates year of publication, O1: skeletal effects, O2: dentoalveolar effects, O3: soft-tissue effects, SfJ: support for judgement, OBP: occlusal bite plate, RHG: reversed headgear, CC: chin-cup, OMA: occipitomental anchorage appliance of maxillary protraction combined with chin-cup traction, QH: quad-helix, URA: upper removable appliance.
Although this was not the first time that this issue has been addressed in the literature, researchers in previous systematic reviews did not investigate the long-term effects of chin-cup therapy [2, 10, 12], the soft tissue changes [2, 10, 12] and the adolescence as a study growth period [10].
Our search strategy resulted in only CCTs, thirteen of retrospective [8, 17-28] and one of prospective design [29], with no RCT found. One possible reason is that RCTs are not common in orthodontics, since various parameters are required. These include patient/observer blinding to treatment and ethical matters regarding the control group whose decision of participation is negatively affected by receiving no treatment.
The final studies were cohort studies with weaknesses due to the serious risk of bias, as it is described in detail in Table 4. All the studies were found to have selection bias, as the selection of both participants and controls was related to the received intervention and likely to the outcomes.
Furthermore, the studies were judged to have a serious risk of bias concerning the outcomes’ measurements when the knowledge of the received intervention by the assessors was likely to influence the outcomes in a way that it could cause statistically significant differences. Thus, three studies [8, 23, 27] received that characterization, as the way that the outcome measure was conducted, was considered to have the potential to significantly affect the outcomes. The risk of bias was judged low, when blinding of outcome assessors was reported [25, 28]. These studies were considered comparable to a well-performed randomized trial with regard to this domain, according to the ACROBAT-NRSI [13]. Consequently, studies pertaining to neither categories, were judged to have a moderate risk of bias [17-22, 24, 26, 29]. Based on the ACROBAT-NRSI [13] in these studies the outcome measure was only minimally influenced by the awareness of the received intervention and any error in measuring the outcome was only minimally related to intervention status. The methods of outcome assessment were comparable across intervention groups both for the studies with a moderate and a low risk of bias.
Another weakness of the observational studies, both prospective and retrospective, is the presence of confounders. In the present systematic review, we considered confounders, all those factors that were possibly related to the chin-cup therapy and could cause significant changes in the results. Ethnicity was needed to be taken into account, as Class III malocclusion is more frequently seen in Asian populations [1, 7, 14-16] and consequently these patients may be more often treated with chin-cups. Moreover, patients of Asian ancestry may present different baseline characteristics, as well as a different growth pattern than other populations, thus significantly affecting the results. The age of the participants in relation to their skeletal maturity stage was also accounted for. This was mainly due the fact that the prepubertal patients may present different results from patients that are in the peak of their growth or later. Skeletal Class of malocclusion was considered a confounder when there was doubt on whether the treated and/or the control group had skeletal Class III malocclusion or when some controls had skeletal Class I. Soft-tissue individual variation in thickness and in tension was co-estimated, since it could affect the reported results regarding the soft-tissue changes, as it was highlighted by Arman et al. [17] and Alacrόn et al. [28]. Finally, pre-treatment overjet was also considered a confounder.
In addition, co-interventions were addressed. More specifically, the use of additional appliances, such as a lingual arch to flare the maxillary incisors [23, 26] or a quad-helix appliance [21] were considered critically important co-interventions that could significantly alter the outcomes. To illustrate this, in four studies [17, 19, 20, 24] the declared proclination of the upper incisors [17, 19, 20, 24] followed by forward movement of the soft-tissue point A [17] and the upper lip [17, 19, 24] was probably the result of an additional occlusal bite plate [17, 19], an upper removable appliance [24] and of the combination of maxillary protraction and chin-cup traction in an occipitomental anchorage appliance [20]. The significantly increased overjet [17, 19-21, 24] that was noted, was expected to be a result of the aforementioned additional appliances. However, it was also reported in studies where patients, treated solely with chin-cups, were contrasted to untreated controls [8, 28, 29]. One possible reason is the occlusal interferences in the transition of the occlusion from a one with underjet to one with overjet [8], that flare the upper incisors. It could also be the result of the significant retroclination of lower incisors caused by the chin-cup [8, 22]. At last, utilization of force magnitude was considered a co-intervention as well, since significant reduction in ramus height was noted when lighter force in chin-cup traction was used [22].
Patients under chin-cup therapy showed an improved facial profile, merely induced by the backward and downward rotation of the mandible [17-20, 26, 28]. This was documented by a decrease in the SNB [17-22] and closure of the gonial angle [20, 23, 25, 26]. It was also correlated with an increase in the anterior facial height [17, 18, 22, 24]. In contrast, Wendell et al. [27] recorded significant decreases in the anterior face height during chin-cup therapy in comparison with untreated controls. This was attributed to the 43% decrease in the downward displacement of pogonion during treatment, which was not stable at the post-treatment observation, when it was increased by 60% [27]. The backward and downward rotation of the mandible was correlated with an increase in the ANB angle as well [17, 19, 21-23]. However, there is ambiguity in whether only the mandible or both the mandible and the maxilla are responsible for this.
Moreover, there is controversy among researchers regarding the retardation of the mandibular growth during chin-cup therapy. A significant reduction of the mandibular length (ramal, body and total length) was reported in five studies [22, 23, 26-28] indicating an improvement in the skeletal profile of the treated patients. Most interesting were the findings of Wendell et al. [27], whose study presented a reduction in absolute mandibular length, which continued after the end of the active treatment. In contrast, the studies of Gökalp and Kurt [29] and Abu Alhaija and Richardson [24] showed significantly increased mandibular body [24, 29] and total mandibular length [24]. Gökalp and Kurt [29] attributed these alterations in the forward bending of the condyle, as a result of bone deposition between the condylar head and neck during chin-cup therapy.
The aforementioned controversy led to further investigating attempts by researchers in order to elucidate the role of chin-cup therapy in the retardation of mandibular growth. Similar attempts were also made to assess the potential influence of chin-cup therapy in the appearance of Temporomandibular Joint Disorders (TMD). It has been speculated that internal derangement of the TMJ is likely to occur due to the direct application of the backward chin-cup’s force on the mandibular condyle [7]. This was recently evaluated in a systematic review [7] by Zurfluh et al. who, interestingly, concluded that despite the craniofacial adaptations induced by chin-cups in patients with Class III malocclusion, chin-cup therapy does not constitute a risk factor for the development of TMD, as the existence of insufficient or low-quality evidence in the literature do not allow clear statements regarding the influence of chin-cup treatment on the TMJ. Nevertheless, they related TMD with age and a stressful lifestyle that seem to differentiate the effects imposed on TMJ.
As for the soft-tissue effects, although confounding was evident, the documented results indicate a general soft-tissue profile improvement when the chin-cup is used in skeletal Class III patients. However, in the lack of studies that evaluate the long-term stability of the aforementioned changes, no definite conclusions can be reached.
In the basis of these manifestations, it is evident that the effects of chin-cup therapy both in the short-and especially in the long-term need further investigation and better substantiation with more high-quality evidence to draw reliable conclusions.
CONCLUSION
In summary, the present systematic review shows that the chin-cup therapy can be considered for the short-term treatment of growing patients with Class III malocclusion. More specifically, the following are evident:
- The skeletal profile is improved, as it is confirmed by significant changes in measured variables, which indicate a downward and backward rotation of the mandible.
- Favorable dento-alveolar changes, such as a significant increase in overjet are also observed. However, data need to be carefully interpreted in the presence of co-interventions, such as additional appliances that could have an impact on the outcomes.
- The soft tissues show a general improvement in the facial profile, following the accompanying skeletal and dento-alveolar changes, but with uncertain long-term stability.
Nevertheless, existing limitations that do not permit a clear judgement need to be taken into account. The unclear role of chin-cup therapy in the retardation of mandibular growth, the need for further investigation of the long-term effectiveness and the general lack of high quality evidence suggest cautious interpretation of the reported findings and highlight the need for future research with more high-quality evidence-based clinical trials, in order to draw reliable conclusions.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


