All published articles of this journal are available on ScienceDirect.
Odontogenic Sinusitis Caused by an Inflammation of a Dentigerous Cyst and Subsequent Finding of a Fibrous Dysplasia. A Case Report
Abstract
We report the case of a 38-year old male patient with sinusitis caused by an infected follicular cyst due to an ectopic impacted third molar in the right maxillary sinus.
A 10-day antibiotherapy regimen was administered; subsequently, the cyst and the third molar were removed achieving complete recovery.
Fibrous dysplasia was diagnosed at follow-up examination (occupation of the maxillary sinus by bone tissue was observed in a radiographic examination) and confirmed by biopsy.
In cases of odontogenic sinusitis, thorough examination is crucial, as evidenced by the case reported in this study.
A Literature review was performed in order to identify the diagnostic methods currently available and the clinical features, complications and treatment for both, odontogenic maxillary sinusitis and fibrous dysplasia.
INTRODUCTION
Odontogenic sinusitis is a unilateral infection of the maxillary sinus caused by a dental infection [1].
It can be found mixed with aerobic and anaerobic oropharyngeal flora such as streptococci, bacteroides, veillonella, fusobacterium, etc. [2].
A periapical infection can occasionally reach the maxillary sinus causing odontogenic sinusitis due to proximity of the upper posterior teeth. Other causes of odontogenic sinusitis include periodontitis, perforation of the Schneiderian membrane of the sinus during extraction or surgery, or the presence of root tips or other foreign bodies such as endodontic obturation materials in the sinus [2, 3]. The palatal root of the first molar is the part most frequently associated with odontogenic sinusitis [4].
An ectopic tooth in the maxillary sinus can cause sinusitis [5] as well as dentygerous cysts, keratocystic odontogenic tumor, odontomas and bone tumors like ossifying fibromas [2, 6].
There is evidence that maxillary sinusitis of odontogenic origin represents 10% of all maxillary sinusitises [3, 7]. According to Maillet [4], the incidence can raise to 51.8%.
In terms of clinical symptoms, many patients with odontogenic sinusitis do not refer upper teeth pain [1]. The most common symptoms are nasal obstruction, facial pain, headache, snoring, acute sinus perforation and swelling [8]. Also, odontogenic sinusitis can manifest in the form of nasal congestion or discharge, facial pressure, anosmia and cacosmia [1, 9]. The patient may have a dental infection or have undergone previous oral surgery [10].
Diagnosis is based on a combination of clinical symptoms and radiographic findings. When sinusitis is unilateral and non-responsive to treatment, then odontogenic sinusitis should be considered [2, 9].
Panoramic radiographies have an important drawback: there are anatomical superimpositions, and visualizing the topographical relationship between the upper molars and the maxillary sinus may be difficult [7]. Nevertheless, an ectopic molar in the maxillary sinus can be easily diagnosed with a panoramic radiography [5].
Water’s view provides a good visualization of the sinus, but it is useless for detecting an ectopic molar in the maxillary sinus [8].
Three-dimensional imaging systems display multiple sections of the maxillary sinus (bone and soft tissue), whereas computed tomography eliminates the superimposition of structures [1, 4].
Cone Beam computed tomography (CBCT scanning) -a more effective imaging system- shows apical periodontitis and mucosal thickening, as well as dental pathologies related to the maxillary sinus [7, 11, 12]. CBCT scanning is a three-dimensional radiography that produces high-resolution images with low doses of radiation, as compared to conventional computed tomography scanning [3]. Although resolution and radiation dosage are very heterogeneous among different CBCT devices. Whereas, the mucosa in a healthy sinus is less than 2 mm thick, it increases to an average of 7.4 mm in chronic sinusitis [4]. Another characteristic of sinusitis is radiographic opacity due to accumulation of fluid.
A panoramic radiograph can be enough for follow-up examination [8]. Although magnetic resonance imaging provides a better visualization of soft tissue, it is not useful for odontogenic sinusitis.
Odontogenic sinusitis can be resolved by just treating the dental cause (endodontic treatment, cystectomy, etc.) [9]. However, when symptoms are acute, antibiotic treatment with amoxicillin-clavulanic acid or clindamicyn is necessary. Other useful antibiotics are: trimethoprim-sulfamethoxazole or doxycycline, cefuroxime, ceftriaxone, cephalexin, cefoxitin, ceftriaxone and azitromycin [1, 2]. Saline nasal sprays and decongestants may be necessary [2].
Surgery can be carried out endoscopically better than the Cadwell-Luc approach [2].
The infection can progress and cause serious complications such as cerebral abscess [13]. Akhaddar reported an orbital abscess associated with an odontogenic sinusitis [14].
Fibrous dysplasia (FD) is a benign tumor of the bone characterized by replacement of normal bone by fibro-osseous tissue. It is caused by somatic activating mutations in the subunit of the stimulatory G protein [15]. It begins in childhood and it usually stops at puberty, although about a third of patients have progression in adulthood [16].
FD may involve a single bone (monostotic) or multiple bones (polyostotic), and it affects long bones, ribs and cranio-facial bones more frequently. As many as 70% of lesions are monostotic and asymptomatic. Diagnosis is usually incidental finding. The extent of the lesion can be determined by computed tomography imaging, but a presumptive diagnoses must be confirmed by a histopathological study. Radiographic findings include radiolucency, ground-glass appearance, and a smoking cloudy and even radiopaque fingerprint [17, 18].
Between 10% and 25% of FD lesions involve the cranio-facial bones, being the maxilla the most frequently affected bone. Finally, it also can cause obliteration of the paranasal sinuses [16, 19].
Treatment for FD is conservative [19]. Bisphosphonate therapy is indicated for selected patients with pain, fracture risk and dysfunction. Surgery is indicated for biopsy, correction of deformity and painful lesions [20].
FD must be differentially diagnosed from ossifying fibroma, Paget´s disease and giant cell tumor [18, 21]. Regarding the prognosis, fibrous dysplasia commonly has a slow growth. Malignant change to osteosarcoma is very rare [22].
CASE REPORT
A 38 year-old man presented with a swollen right cheek, pain and rhinorrhea of 15 days of evolution. He had not got any systemic diseases.
The patient reports to have been examined by an otolaryngologist, who prescribed him a treatment with antibiotics. Since no remission was evident, the patient was referred to our clinic to rule out an odontogenic cause.
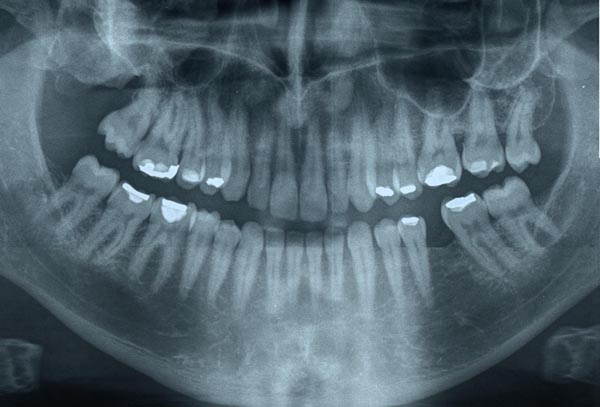
The patient provided an orthopantomography that revealed that the upper third molar was displaced to the maxillary sinus by the pressure of a cyst that went unnoticed by the otolaryngologist (Fig. 1).

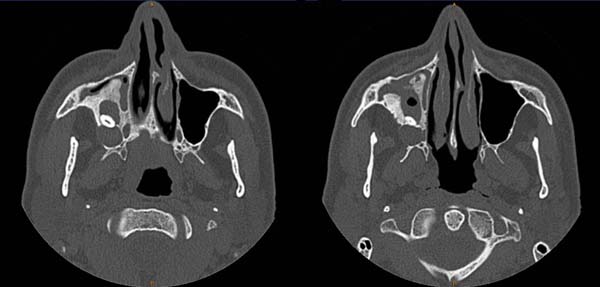
A computed tomography (CT) scan was obtained to improve diagnostic imaging, showing a cystic lesion with involvement of the bone (Fig. 2).
The cyst and the ectopic third molar were dissected under local anesthesia (Articain 40/0,005 mg/ml) (Figs. 3-6). Amoxicillin 875mg/clavulanic acid 125mg, for seven days and ibuprophen 600mg, three times daily for pain control, if needed, were administered postoperatively.

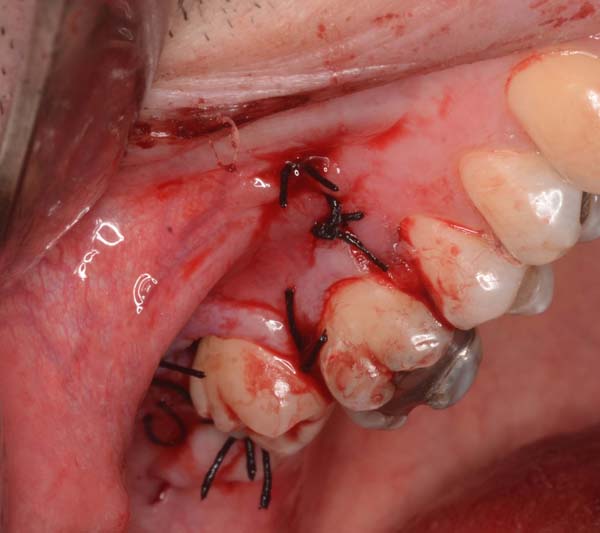


The cystic capsule was sent for histopathological examination; the diagnosis was a dentigerous cyst with signs of inflammation.
Postoperative complications were not observed and the patient remained asymptomatic over a follow-up period of seven months.
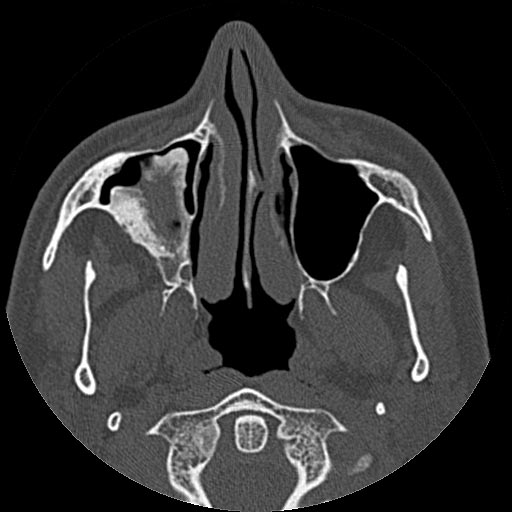
Follow-up orthopantomography imaging was performed at seven months following surgery (Fig. 7). The maxillary sinus was almost completely occupied by bone, so we decided to refer the patient for another scan. The new scan revealed that the maxillary sinus was largely and abnormally occupied by bone, what made us think of a possible fibrous dysplasia (Fig. 8). This was confirmed by a biopsy carried out by a maxillofacial surgeon and by histopathological examination. Conservative treatment was administered with regular follow-up examination.
DISCUSSION
The presence of ectopic teeth in the maxillary sinus is very rare. In this case, an ectopic third molar caused pain, inflammation and rhinorrhea. Displacement to the maxillary sinus had been caused by the pressure exerted by an odontogenic cyst.
It is very important to diagnose the odontogenic origin of maxillary sinusitises, since only the management of the odontogenic cause can lead to the resolution of the infection and avoid recurrence [7].
Most authors use 3D imaging to find the aethiological cause of maxillary sinusitises [2, 7, 23, 24]. In a survey conducted among otolaryngologists, CT scanning was the preferred imaging technique for the diagnosis of odontogenic maxillary sinusitis [6]. Before any kind of sinus surgery it is very important the sistematic study of radiographic anatomy of maxillary sinus [25]. In this sense, the patient´s CT-scan already showed a bony coating around the cystic lesion, so we should have suspected a bone lesion but it went unnoticed.
The pressure exerted by a dentigerous cyst can displace molars into ectopic positions like -as in this case- the maxillary sinus [8, 26]. Other sites of ectopic third molars are the mandibular condyle, the coronoid process and the mandibular angle [27].
Dentigerous cysts are the second most common type of odontogenic cyst after radicular cyst and they can occur in the maxillary very close to the maxillary sinus [2, 28]. Differential diagnosis must be done with radicular cyst, keratocystic odontogenic tumor, ameloblastoma, even extramedullary plasmacytoma of the maxilla [29].
A dentigerous cyst may remain asymptomatic for several years [19, 23, 30]. Treatment includes the enucleation of the cyst and impacted upper third molar [2]. Histopathological examination is essential. A multidisciplinary therapy administered by a dentist and an otolaryngologist is occasionally recommended; in fact, 54% of patients have been reported to resort to a dentist to treat their maxillary sinusitis [9]. Although the symptoms may initially improve with the administration of antibiotics, if the dental pathology remains untreated, the therapy will eventually fail and the symptoms will return [6, 31].
As regards fibrous dysplasia, surgery is controversial. If the lesion is stable with no growth, annual evaluation should be enough [15]. Remodeling resection should be performed to improve the patient’s quality of life and minimize symptoms like exophthalmia, nasal obstruction, etc. However, remodeling should not be performed until the growth phase is completed, and still there is a risk of recurrence (25%) [32].
Lee [33] treats fibrous dysplasia of the maxillary sinus by decortication through the anterior wall of the maxillary sinus by removing all fibrous tissue until the sinus cavity was clear. According to Lee, internal decortication of fibrous dysplasia is effective in minimizing external spread. On the other hand, Yang [34] proposes subtotal or total resection of the lesions and reconstruction with bone grafts. Remodeling resection can cause complications like recurrent painful ophthalmoparesis due to the involvement of the superior orbital fissure [35].
Sontakke [18] has reported two cases of complete obliteration of the maxillary sinus as a result of a fibrous dysplasia. When it affects the maxillary sinus, FD can displace the orbital floor and then fractures can occur in the bones involved [36]. Also, cases of trigeminal nerve compression have been reported [37].
The dental community is wary of treating patients with fibrous dysplasia but Petrocelli in 2014 performed implant rehabilitation of the mandible in a patient with fibrous dysplasia [38]. According to Bajwa [39] dental implants may be considered if the lesions are quiescent. There aren´t many cases published, maybe there is a higher risk of implant failure even osteomyelitis development. There aren´t any complications after dental restorations, tooth extraction or orthodontic therapy [15].
CONCLUSION
In cases of odontogenic sinusitis, thorough examination is crucial as evidenced by the case reported in this study, where a sinusitis caused by a third ectopic molar associated with a dentigerous cyst was accompanied by a fibrous dysplasia that went initially unnoticed and was eventually diagnosed in follow-up examination some months later.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


