All published articles of this journal are available on ScienceDirect.
Osseointegration of Dental Implants in a Patient with Hajdu-cheney Syndrome
Abstract
Background:
Hajdu-Cheney Syndrome (HCS) is a rare hereditary bone metabolism disorder characterized by acro-osteolysis, short stature, craniofacial changes, periodontitis and premature tooth loss. Extensive search of the current literature revealed no reports of implant placement in patients with HCS.
Case Report:
A 22-year old woman with osteoporosis, generalized advanced chronic periodontitis and premature tooth loss was referred to the Postgraduate Clinic of Periodontology, University of Athens-Greece. The patient was diagnosed in 2001 with HCS. The patient received non-surgical periodontal treatment and several teeth were extracted due to extensive alveolar bone loss.
After careful consideration of the possible implications deriving from the patient’s condition and having taken her young age into account, initially, a dental implant was placed in the upper right first premolar region. Specific protocols such as longer healing periods were implemented, so five years after placement and successful osseointegration of this implant, four additional dental implants were placed in the posterior regions of the maxilla and the mandible. Prosthetic rehabilitation followed 6 months after implant placement. Upon completion of periodontal treatment, the patient was enrolled in a periodontal maintenance program.
Results:
Clinical and radiographic examination of the patient during the periodontal maintenance program after implant placement revealed no abnormalities in the implant region.
Conclusion:
Patients with HCS suffer from periodontitis, bone destruction and premature tooth loss. This case indicates the successful osseointegration of dental implants in patients with HCS. However, further research is required in order to determine the predictability of dental implant placement in those patients.
INTRODUCTION
Hajdu-Cheney syndrome (HCS) or acro-osteolysis is an extremely rare autosomal dominant congenital bone metabolism disorder characterized by excessive abnormalities of the cranial, spinal and facial bone structures, severe progressive resorption (acro-osteolysis) of the distal phalanges and generalized osteoporosis [1, 2]. It was named after Nicholas Hajdu (1908-1987), a Hungarian-English Radiologist working in the UK and Dr. William D. Cheney (1899-1985), a US Physician [3, 4].
HCS is an osteolytic syndrome presenting multiple clinical features such as, osteoporosis, short stature, craniofacial and skull changes, periodontitis and premature tooth loss and it is often referred in the current literature as arthro-dento-osteodysplasia [5], cranio-skeletal dysplasia with acro-osteolysis [6], hereditary osteodysplasia with acro-osteolysis [7] and acro-osteolysis with osteoporosis in skull and mandible [8]. Most patients have a normal mental development, whereas others experience mental retardation [9]. This condition is mostly inherited in an autosomal dominant pattern [4, 7], caused by mutations in the NOTCH2 gene [10, 11], although sporadic presentations have been recorded [6, 9].
As already mentioned, the main facial features of HCS include hypertelorism, micrognathia, low-set ears, short neck, small mouth with dental abnormalities, coarse hair and thick eyebrows, hearing loss and a hoarse voice [1, 7]. Additionally, short stature, joint laxity, scoliosis and kyphosis, renal cysts and cardiovascular anomalies may also be present [1]. Radiographic examination of the skull reveals persistent wide cranial sutures with intra sutural bones, absence of the frontal and maxillary sinuses and enlarged sella turcica [1, 3, 8]. Neurologic abnormalities may present due to progressive basilar invagination often resulting to optic nerve head swelling and mild optic neuropathy [12].
Premature exfolation of teeth [3, 7], tooth impactation and maleruption [7], increased tooth mobility [9] and hypoplastic dental roots [5], as well as atrophic alveolar processes [4, 6] are some of the characteristic manifestations of the syndrome in the oral cavity. Already in 1984, periodontal examination of patients with HCS revealed compromised periodontal health [1]. More detailed, the patients presented with rapidly progressive periodontal disease, insufficient zone of attached gingiva and secondary occlusal trauma, whereas radiographic evaluation showed bone morphology abnormalities and reduced bone density [1, 18].
Despite the premature tooth loss experienced by most of the patients with HCS in their young adulthood, extensive search of the current literature revealed no reports of implant placement in patients with Hajdu-Cheney Syndrome. This report presents for the first time the treatment of a young female patient with HCS with dental implants.
CASE REPORT
In 2003, the Department of Oral Pathology and Surgery at the School of Dentistry, University of Athens referred a young 22-year-old female with Hajdu-Cheney Syndrome (HCS) to the Postgraduate Clinic of the Department of Periodontology, in order to receive periodontal treatment (Fig. 1). The patient was diagnosed in 2001 with HCS after clinical, radiographic and histological examination (Fig. 2). After gene examination of both parents, none of them was found bearing a mutation in the NOTCH2 gene [13]. Her physical examination showed that her height was 145cm and her weight was 45kg. The patient had thick coarse hair, low-set ears, small face and stature, thin lips, small mouth and short hands with clubbing of the fingertips (Fig. 3). According to her medical history, the patient suffered from emphysema and allergic rhinitis, whereas oral intake of Vitamin D and calcium were prescribed daily for the treatment of osteoporosis [14, 15].



During orthodontic treatment between the ages of 12 and 21 years, all of her first premolars were removed [16]. At the age of 20 years, the patient received non-surgical periodontal treatment (scaling and root surface debridement), as well as limited periodontal surgery in the lower anterior region [17, 18]. Detailed records regarding both orthodontic and periodontal treatment were not available. The patient was a non-smoker, visited her dentist every 6 months, brushed her teeth twice every day (Bass technique) and used dental floss and interdental brushes. At the time of the referral, the patient suffered from generalized advanced chronic periodontitis, increased tooth mobility and premature tooth loss [18]. Clinical and radiographic examination of both parents and her 4 years younger brother showed that the mother and the younger brother had normal dentition, whereas the father was diagnosed with chronic advanced periodontal disease with increased mobility of various teeth.
The patient was treated in collaboration with the Department of Prosthodontics. Clinical and radiographic examination of the patient revealed a number of significant findings. There was generalized horizontal bone loss of ~ 50%. However, alveolar bone loss around various teeth such as #4 (in place of #5), 14 and 24 was extensive (~ 100%). Tooth roots appeared short and cervical, whereas cervical resorption lesions were also evident (teeth #3, 10, 20 (in place of #19), 26) [2, 19]. The patient received non-surgical periodontal treatment in all four quadrants, which included scaling and root surface debridement. During this period, teeth #4, 14 and 24 were extracted due to extensive alveolar bone loss [20]. The maxilla was then rehabilitated with the placement of a provisional fixed partial denture of metal acrylic and the anterior region of the mandible with the placement of a Maryland bridge [21] (Fig. 4). Upon completion of the periodontal treatment, the patient was enrolled in a periodontal maintenance program.
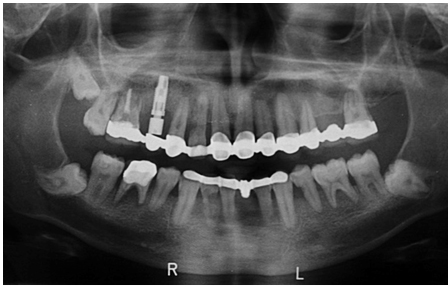
After careful consideration of the possible implications deriving from the patient’s condition (osteoporosis, generalized advanced periodontitis) and having taken her young age into account, we decided to proceed with the placement of dental implants, while implementing specific protocols such as longer healing periods. So, although in the current literature no other case of implant placement in a patient with HCS was described, in February 2005, a dental implant (Nobel Biocare, Replace Select Straight, TiUnite RP 4.3 x 13mm) was placed in the upper right first premolar region [22] (Figs. 4, 5).

During the healing period, in March 2009, further teeth were extracted (#2,3,30). During the extraction of tooth #30, a bovine xenograft (Geistlich Bio-Oss Collagen 250 mg) was placed in the post-extraction site, in order to achieve ridge preservation [23] and the region was rehabilitated with a resin-bonded bridge (Maryland bridge).
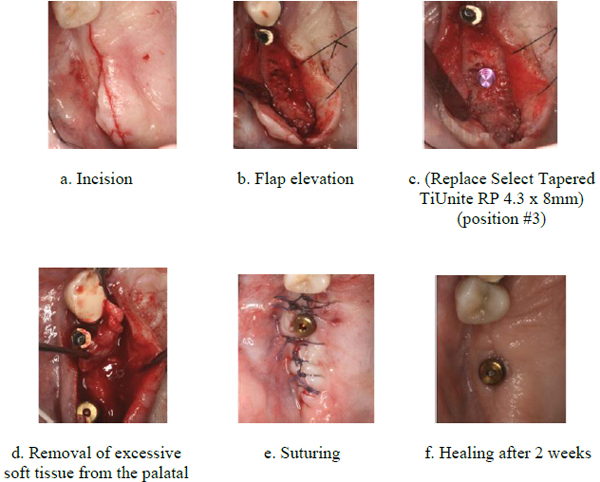
Five years after placement and successful osseointegration of the dental implant in position #5, an additional implant (Nobel Biocare, Replace Select Tapered TiUnite Regular Platform (RP) 4.3 x 8mm) was placed in the upper right first molar region (Fig. 6a-f). Bone mineral density appeared physiological (Bone Type III) (Fig. 7).

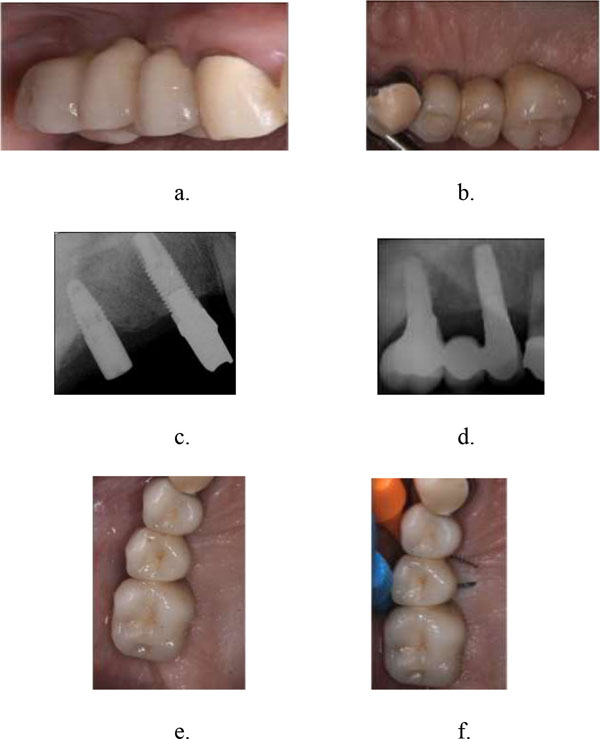
Six months after implant placement, a porcelain fused to metal, three unit implant supported fixed partial denture 3 (4) 5 was placed in the upper right region (Fig. 8a-f). During this period of time, teeth # 18, 19 were extracted due to excessive bone loss.
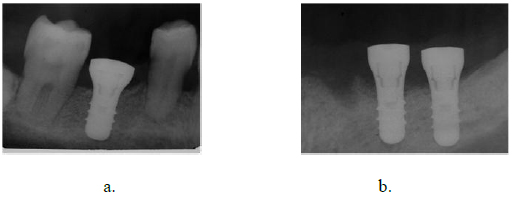
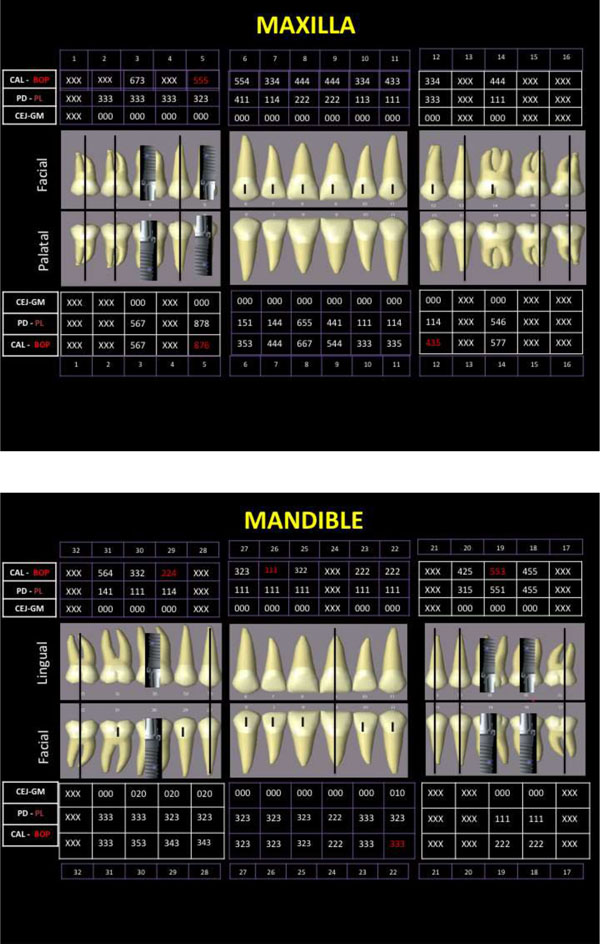
Clinical and radiographic examination of the patient during the periodontal maintenance program in three months interval after implant placement revealed no abnormalities in the implant region. After successful oral rehabilitation of the posterior upper right region, 2 additional dental implants were placed in the posterior left region (during surgery tooth #20 - in place of #21- was extracted) and 1 in the posterior right region of the mandible (Straumann Standard Platform (SP) Tissue Level) (Figs. 9-11).


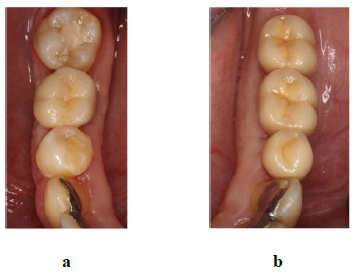
Six months after implant placement, a porcelain fused to metal, three unit implant supported fixed partial denture [20] 19 18 was placed in the left region of the mandible, whereas a porcelain fused to metal implant supported crown was placed in the right region of the mandible (Fig. 12a-b).
Five years after implant placement, clinical and radiographic examination of the patient during the periodontal maintenance program (in three months interval) revealed no abnormalities (Figs. 13-15).


For the reader’s better understanding, Table 1 presents the patient’s detailed dental treatment chronologically.
| Age in years (Year) | Treatment |
|---|---|
| 12-21 (1991-2000) | Orthodontic treatment |
| 13 (1992) | Extraction of all first premolars |
| 20 (2001) | Diagnosis of HCS |
| 20 (2000) | Periodontal treatment (OH instructions, scaling, root surface debridement) and limited periodontal surgery |
| 22 (September 2003) | Referral to the Department of Oral Pathology and Surgery, School of Dentistry, University of Athens, Greece |
| 22 (November 2003) | Referral to the Postgraduate Clinic of the Department of Periodontology, School of Dentistry, University of Athens, Greece |
| 23 (2004) | Non-surgical PT, extraction of #4, 14, 24, placement of a Maryland bridge in the anterior region of the mandible |
| 24 (February 2005) | Placement of a dental implant in the upper right first premolar region, placement of a provisional fixed partial denture of metal acrylic in the maxilla |
| 24-28 (2005-2009) | Periodontal maintenance program |
| 28 (March 2009) | Extraction of #2, 3 and #30 (with bovine xenograft placement), placement of a Maryland bridge 29 (30) 31 |
| 29 (April 2010) | Placement of a dental implant in #3 |
| 29 (October 2010) | Extraction of #18, 19, placement of a porcelain fused to metal three unit supported fixed partial denture 3 (4) 5 |
| 30 (January 2011) | Extraction of #20, placement of 3 dental implants in the lower jaw (in positions #19, 20 and 30) |
| 30 (July 2011) | Placement of a porcelain fused to metal, three unit implant supported fixed partial denture (20) 19 18 and a porcelain fused to metal implant supported crown 30 |
| 30 - present (2011- present) | Periodontal maintenance program |
DISCUSSION
Hajdu-Cheney syndrome (HCS) is an inheritable, rare, bone metabolism disorder, characterized by excessive abnormalities of the cranial, spinal and facial bone structures, severe progressive resorption (acro-osteolysis) of the distal phalanges and generalized osteoporosis. According to the oral and dental findings of various clinical studies (mostly case reports or series), patients with HCS suffer of periodontitis with rapid bone destruction, increased tooth mobility and premature tooth loss [2, 18, 19].
A 22-year old woman with osteoporosis, generalized advanced chronic periodontitis, increased tooth mobility and premature tooth loss was referred to the Postgraduate Clinic of Periodotology initially in 2003. The patient was diagnosed 2 years ago with HCS after clinical, radiographic and histological examination [1-4]. Reason for the referral was the need for periodontal treatment and oral rehabilitation of the edentulous regions.
For the treatment of osteoporosis, the patient received per os Vitamin D and Calcium in a daily basis. According to the results of recent studies, osteoporosis is not a causal factor in the development of moderate to severe chronic periodontitis [24], whereas some researchers suggest that oral intake of Vitamin D adjunctive to periodontal treatment may positively affect its outcome in patients also diagnosed with osteopenia/osteoporosis [25]. Initially, the patient received non-surgical periodontal treatment, which included oral hygiene instructions, scaling and root surface debridement and was enrolled in a 3-month-intervall periodontal maintenance program. However, the periodontal management of such patients can be a challenge for the clinician. The combination of the disease’s pathology and the compromised regeneration’s ability of such patients may contribute to further deterioration of the periodontal condition of the patient [1]. Although, studies have shown, that further periodontal disease progression and subsequent premature tooth loss may be effectively prevented by treatment of juvenile or early adulthood periodontitis [17], the patient underwent extractions of several teeth due to extensive alveolar bone loss.
The decision to proceed with the placement of dental implants, although in the current literature no other case of dental implant placement in a patient with HCS was described, was taken after careful consideration. The periodontal condition and the young age of the patient as well as osteoporosis formed our major concerns. Most studies agree, that patients with dental implants replacing teeth lost due to periodontal disease demonstrated lower survival rates and more biological complications and therefore, specific criteria should be met [22]. Furthermore, clinical studies showed, that osteoporotic subjects presented higher rates of implant loss, however, there are not adequate evidence to support the hypothesis that osteoporosis may negatively effect the bone healing [26]. Therefore, specific protocols and longer healing periods are recommended when treating osteoporotic patients with dental implants [27].
Five years after placement and successful osseointegration of a dental implant placed in the upper right first premolar region, four additional implants were placed in the upper and lower posterior regions. Prosthetic rehabilitation followed 6 months after implant placement with the placement of fixed partial dentures. Finally, the patient was enrolled in a strict 3-months- interval periodontal maintenance protocol, in order to maintain periodontal and peri-implant tissue health on a long-term basis. 5 years after implant placement, clinical and radiographic examination of the patient during the periodontal maintenance program revealed no abnormalities in the implant region.
CONCLUSION
Patients with Hajdu-Cheney syndrome suffer of severe periodontitis with rapid bone destruction and increased tooth mobility. Despite the fact that premature tooth loss is often observed in those patients at a rather young age, there is no record or publication of any clinical study regarding dental implant placement in such patients. The fact that HCS is an extremely rare hereditary bone metabolism disorder characterized by excessive abnormalities of multiple bone structures and generalized osteoporosis may further complicate the oral rehabilitation treatment plan.
This case implies the osseointegration of dental implants in patients with Hajdu-Cheney Syndrome. However, further research is required in order to examine the predictability of oral rehabilitation of those patients with placement of dental implants, although a larger patient population is difficult to obtain.
LIST OF ABBREVIATIONS
| BOP | = Bleeding on Probing |
| CAL | = Clinical Attachment Level |
| CEJ | = Cemento-Enamel-Junction |
| GM | = Gingival margin location, recorded at six sites per tooth mesio-buccal, mid-buccal, disto-buccal, mesio-palatal/mesio-lingual, mid-palatal/mid-lingual, and disto-palatal/disto-lingual |
| HCS | = Hajdu-Cheney Syndrome |
| OH | = Oral Hygiene |
| PDP | = Probing Depth |
| PL | = Plaque Index |
| PT | = Periodontal Treatment |
| RN | = Regular Neck |
| RP | = Regular Platform |
| SP | = Standard Platform |
| WN | = Wide Neck |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to thank Meropi Armaou, DDS, Postgraduate Student, Department of Prosthodontics, School of Dentistry, University of Athens and Nefeli Tsagkari, DDS, Postgraduate Student, Department of Prosthodontics, School of Dentistry, University of Athens for the prosthetic rehabilitation of the patient.


