Local Anaesthetic Drug Administration in Dentistry Using Computer Assisted Anaesthetic Delivery System: A Systematic Review
Abstract
Background:
Local anaesthetics play a key role in reducing pain and anxiety during dental treatment. However the disadvantage of using syringe and needle technique in the maxilla, proximal to the apices of the teeth is that it is painful and also leads to collateral anaesthesia. Hence this systematic review aims to identify whether computer assisted local anaesthetic delivery system could produce predictable results similar to conventional syringe needle technique and also eliminate the disadvantages.
Method:
Electronic databases were searched for eligible studies. A pre-tested data extraction form was created and following data were extracted from each eligible study: trial site, year, trial methods, participants, interventions and outcomes. A significant heterogeneity was seen in between the eligible studies.
Results:
Six studies met the inclusion criteria and were included in the present review. One was cross-over and one split mouth, while others were parallel. Only one was open label and the rest were single blinded. Three studies were conducted in children while the rest in adults. The outcome measurement was directed to measure psychological attributes using visual analog scale, electric pulp testing and pain behaviour code.
Conclusion:
Unfortunately because of the clinical heterogeneity, meta-analysis could not be performed. Hence it is difficult to conclude that the computer assisted delivery is better than the conventional method, although it was found to perform better. Many high quality studies assessing the efficacy and cost-efficiency of various modes of administration are required to confirm the utility of computer assisted delivery systems.
INTRODUCTION
Pain is the most common cause of fear and anxiety in dental practice. Local anaesthetics play a key role in reducing pain and anxiety and are used with or without epinephrine in specified concentrations for various dental procedures. [1, 2] As regards the maxillary anaesthesia, supraperiosteal injections into the mucobuccal fold, proximal to the apices of the teeth using conventional syringe and needle have been commonly used. However certain instances may warrant multiple needle penetrations for adequate pulpal anaesthesia, which increased the dose and caused collateral anaesthesia [3, 4]. In the mid-1990s, the computer assisted system has been developed which provided predictable pulpal anaesthesia of multiple maxillary teeth from a single injection, minimizing the dose with minimal or reduced risk of collateral anaesthesia. It incorporated computer technology to control the rate of flow of the anaesthetic solution through the needle. This concept was called computer-controlled local anaesthetic delivery (CCLAD) [5, 6]. It has a foot control that automates at precise pressure and volume rates which control the drug being delivered. It could be used for buccal, palatal, intraligamental infiltration and blocks. Some of the commercially available CCLADs are Wand, Wand plus and Compumed. Anterior middle superior alveolar (AMSA) and Palatal anterior superior alveolar (P-ASA) techniques are most frequently used with the computer assisted system. [7-9] Besides the introduction of the technique, a systematic compilation on studies does not exist. Hence this systematic review aims to identify the use of computer-assisted local anaesthetic technique in producing predictable anaesthesia as conventional syringe needle technique, eliminating the disadvantages.
METHOD
Information Sources and Search Strategy
The protocol for this review was registered with International prospective register of systematic reviews (PROSPERO) with the registration number CRD42015032590. The review protocol can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015032590. Literature search was conducted using key words computer controlled anaesthesia [tiab] and was completed on 23 Dec 2015. The primary data base used was Medline (via PubMed), Cochrane central register of clinical trials (CENTRAL) and Database of Abstracts of Reviews of Effects (DARE). This search was further supplemented by hand searching of relevant references from review articles and other eligible studies. No limits were applied to the year of study but only studies published in English language were included.
Eligibility Criteria
Only those studies with randomized controlled design with the following requirements were included in the present study:
- Type of participants - Adults/children requiring infiltration or block local anaesthesia for dental procedures in the maxillary arch
- Types of intervention - Any local anaesthetic drug administration in the maxillary arch using computer assisted delivery system
- Comparison - Any local anaesthetic administration in the maxillary arch using traditional needle technique or using a computer assisted system
- Outcome - Assessment of the efficacy of local anaesthetic using electric pulp testing, assessment of pain using VAS, assessment of behaviour using behaviour codes
Study Procedure
Both the authors independently screened the above mentioned data bases for studies and independently reviewed abstracts for suitability. Full-texts articles were obtained for those found to be eligible to be included and for those that were inconclusive on the abstract screening. A pre-tested data extraction form was created and both the authors independently extracted the following data from each eligible study: trial site, year, trial methods, participants, interventions, and outcomes. Disagreement between the authors was resolved through discussion. A significant heterogeneity was seen in between the eligible studies. The present meta-analysis was conducted and presented in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. [10, 11].
RESULTS
Search Results
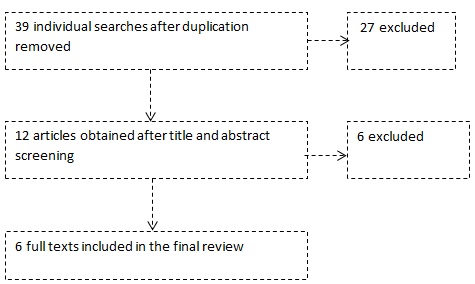
A total of 39 articles were identified, of which 12 was shortlisted on title screening. Of the 12, two assessed the efficacy of different local anaesthetic agents delivered using CCLAD, one was not randomized and three were on healthy patients that assessed pain due to injection technique only. After full text and abstract screening, six studies met the inclusion criteria and were included in the present review. The study flow chart is shown in Fig. (1).
Key Features of Included Studies
Six studies [12-17] were found to be eligible to be included. Of these six studies, one was cross-over [13], one split mouth [14] while all others were parallel group studies. Only one [12] was open label and the rest five [13-17] were single blinded. Three studies [12, 15, 17] were conducted in children while the rest in adults [13, 14, 16, 17]. The outcome measurement was directed to psychological attributes in two studies [12, 15, 17], visual analog scale in four studies [12, 13, 15, 16] and electric pulp testing in Kandiah et al. [16]. Other salient features of the included studies are listed in Table 1. Due to significant clinical heterogeneity between the included studies, meta-analysis was not carried out. But considering all the included studies, the computer assisted technique performed better than the conventional syringe needle technique for administration of local anaesthetic in terms of pain measured using VAS, psychological attributes and predictable anaesthesia achieved which was measured using electric pulp testing. Risk of bias of the included studies was assessed as per Cochrane’s risk of bias tool [10] and is depicted in Fig. (2).
| Study ; Type of Study: |
Participants | Intervention | Control | Outcome | |||
|---|---|---|---|---|---|---|---|
| Outcome measure used | Numerical values | ||||||
| Intervention Group | Control Group | ||||||
| Klein et al. [12] RCT; open label; parallel group |
21 children of 3-5 years of age who required pulp tissue removal and subsequent crown/extraction for at least two teeth in the anterior maxillary segment on opposite sides of the midline | P-ASA with CompuMed- 1.4 ml of 2% lignocaine with 1:100,000 epinephrine | Several buccal infiltrations and an additional palatal injection- Traditional syringe- 2% lignocaine with 1:100,000 epinephrine in 1.8ml cartridge with a 30-gauge needle | Disruptive behaviour using anxious and disruptive behaviour code | 50% disruptive behaviour, 30% crying and 28% body movement were observed |
75% disruptive behaviour, 57% crying and 49% body movement were observed |
|
| Loomer PM et al. [13] RCT, single blind, cross over design |
20 adults with moderate periodontal disease requiring scaling and root planning | AMSA and P-ASA using 2% lignocaine with 1:100,000epinephrine. | PSA,MSA,ASA,GP,NP using 2% lignocaine in 1:100,000 epinephrine | Visual analog scale (VAS) | A mean (SD) difference of 0.19 (0.24) was observed in VAS from baseline | A mean (SD) difference of 0.22 (0.24) was observed in VAS from baseline | |
| Yenisey M [14] RCT, single blinded study using split mouth design |
16 adult patients aged 27 to 64 years, with partially edentulous state in both right and left maxilla to undergo fixed prosthodontics treatment | AMSA using Wand at 1.7 ml articaine hydrochloride with 0.006 mg adrenaline using 27 G needle | 2 ml articaine hydrochloride with 0.006 mg adrenaline with 27 G needle with a plastic syringe | Verbal rating scale (VRS) | Median (range) of VRS was 0 (0-2) | Median (range) of VRS was 2 (0-3) | |
| Tahmassebi et al. [15] RCT; single blinded; parallel group |
38 children of age 39-120 months in need of at least one restoration on either side of maxilla | Wand assisted buccal infiltration and direct palatal injection of 2% lignocaine in 1:80000 adrenaline | Buccal and intra papillary infiltration using 2% lignocaine in 1:80000 adrenaline | The anxiety using Venham scale and modified VAS for pain |
Mean (SD) of anxiety score - 1.7 (2.5) and 32.1 (30.8) for VAS | Mean (SD) of anxiety score - 1.5 (1.9) and 29.4 (22.4) for VAS |
|
| Kandiah et al. [16] RCT; single blinded; parallel group |
30 individuals of 8-16 years with minimal caries requiring restoration of upper first permanent molar tooth | Wand assisted infiltration using 1.8 ml of 2% lignocaine in 1:80000 adrenaline | Traditional syringe assisted infiltration of 1.8 ml of 2% lignocaine in 1:80000 adrenaline | Onset of anaesthesia measured by Electric pulp testing; Pain measured by modified visual analog scale |
Mean (SD) of onset of anaesthesia was 6.8 (3.1) and 14/15 had no pain |
Mean (SD) of onset of anaesthesia was 6.1 (2.7) and 12/14 had no pain | |
| Allen et al. [17] RCT; single blinded; parallel group |
40 patients 2-5 years of age needing operative dentistry in maxilla | Wand assisted AMSA or P-ASA of 1.4 ml 2% lignocaine with 1:100000 epinephrine using 30 G needle | Traditional 1 ml buccal infiltration and 0.18 ml palatal injection of 2% lignocaine with 1:100000 epinephrine using 30 G needle | Any disruptive behaviour; Crying; Body movement and restraint | 50% had disruptive behaviour; 30% had crying spells; 28% had body movement and 3% restraint | 71% had disruptive behaviour; 57% had crying spells; 49% had body movement and 34% restraint | |

DISCUSSION
Anxiety and fear form the mainstay of deferral in patients undergoing dental treatment, especially involving the injection of local anaesthetics. Recent advances in the field of dental local anaesthesia has come up with the computer controlled anaesthetic delivery vehicle which acts by regulating the rate of flow and delivery of the anaesthetic agent, thereby decreasing the amount of discomfort produced. Additionally the undesired extra oral soft tissue anaesthesia can be eliminated. For the local anaesthetic to provide the required depth of anaesthesia, they must be injected. The main problem lies in the needle and not the cartridge or the syringe. Dental needles are usually 25, 27 or 30 gauges, however the perception remains indistinguishable [18]. Unfortunately this ability to provide painless injection is considered one important factor by patients in selecting their dentist [19]. The Computer -controlled local anaesthetic delivery (CCLAD) was introduced in the mid-1990. A light weight handpiece in a pen like grasp delivers the drug with a foot-activated control. The flow rate of the drug is controlled by the computer, which provides consistent injection from one to other [20]. Commercially available systems include Wand/CompuDent™ system, Comfort Control Syringe™, QuickSleeper™ and Anaeject™.
The maxillary palatal injections are considered to be the most painful because of the mucosal binding to the underlying periosteum and its abundant nerve supply. The pain caused is mainly as a result of displacement of the mucoperiosteum rather than the needle penetration [21]. The introduction of computer assisted system would definitely be of much value in reducing significant discomfort caused due to traditional needle injection technique theoretically. Many individual randomized controlled studies of high quality, which are included in this review, have tested the newer method of delivery of LA (CCLAD) and identified it to be more effective than conventional [12-17]. Unfortunately because of the clinical heterogeneity amongst the studies, a synthetic meta-analysis could not be performed. Hence, at the moment it is difficult to conclude that use of computer assisted delivery is superior to the conventional method, although it was found to perform better from individual studies. More such high quality studies assessing the efficacy and cost-efficiency of various modes of administration are required to confirm the utility of computer assisted delivery systems.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


