All published articles of this journal are available on ScienceDirect.
Caries Removal by Chemomechanical (Carisolv™) vs. Rotary Drill: A Systematic Review
Abstract
Background:Chemomechanical caries removal is an effective alternative to the traditional rotary drilling method. The advantages of chemomechanical techniques in terms of the need for anesthesia, pain perception and patient preference are systematically reviewed and a meta-analysis of the time required for caries removal is reported. Method: Randomized controlled studies of comparison of chemomechanical techniques with conventional rotary drill were selected from a systematic search of standard biomedical databases, including the PubMed and Cochrane clinical trials. Non-repeated search results were screened for relevance and risk of bias assessment, followed by methodology assessment. Statistical models were applied to the outcome parameters - time required, pain perception, need of anesthesia and patient preference - extracted from the studies. Results: Out of the 111 non-repeated search results, 26 studies receiving a low bias score were selected for the review, and 16 randomized clinical trials of rotary and Carisolv techniques were considered for meta-analysis. Meta-analysis by fixed effect as well as random effect models indicate that Carisolv takes more time (3.65 ± 0.05 and 4.09 ± 0.29 min) than rotary drill (8.65 ± 0.09 and 8.97 ± 0.66 min) method. Advantages of reduced pain (14.67 for Carisolv vs. 6.76 for rotary drill), need for anesthesia (1.59% vs. 10.52%) outweigh the longer time requirement and make it the preferred (18.68% vs. 4.69%) method. Conclusion: Chemomechanical techniques stand out as a minimally invasive and preferred method based on the meta-analyses. Evaluation of pain experienced using robust methods is needed to strengthen the evidence for their use.
INTRODUCTION
Dental caries is one of the most prevalent chronic diseases, causing localized dissolution and destruction of the calcified tooth tissue. In certain cases, it may result in infection of the dental pulp [1]. There is a general agreement among clinicians that the key objective of treating carious lesions is to remove the infected layer, leaving the unaffected dentin intact [2]. It is significant to differentiate these layers to prevent the painful and unnecessary removal of sound tooth structure [2, 3].
Restorative dental treatment in children, comprising of removal of caries with conventional drill, is traumatic primarily due to fear and anxiety of children and their parents [4]. The aversion to the noise of rotary instruments and anesthesia are the key factors triggering fear and anxiety [5]. In most cases, these factors delay or avoid the uptake of dental treatment by children, leading to emergency situations. However, in such scenarios, the treatment will be even more complicated with the mandatory use of anesthesia [6]. On the other hand, there is a need for preserving tooth tissue, combined with a patient-friendly approach in every field of dentistry. The ideal strategy in restorative dentistry to ensure maximum life for the natural tooth is to preserve the sound tissue from further damage using minimally invasive techniques [7]. Diverse techniques such as, air abrasion, atraumatic restorative technique, sono-abrasion, laser and chemomechanical methods are in use for caries removal [7-10]. Among these techniques, chemomechanical caries removal is generally considered as an effective alternative to the traditional rotary drilling method.
First chemomechanical agent for removing carious dentin was marketed under the name GK-101 in 1972 [11]. It consisted of a non-specific proteolytic agent, sodium hypochlorite in Sorensen’s buffer. Even after several stages of improvement of the product and FDA approval in 1984 as Caridex, chemomechanical method gained limited acceptance due to major limitations like high cost, complexity, taste of the liquid, short life span, requirement of special equipment and large quantities of the gel, and heating. A new patented system called Carisolv™ was introduced in 1998. In contrast to Caridex, the new system uses three amino acids – lysine, leucine and glutamic acid– to enhance the effect of sodium hypochlorite on denatured collagen, and to decrease the involvement of healthy hard dental tissue, although some of the disadvantages remained [3, 12]. Papacarie™, developed in 2003, has bactericidal, bacteriostatic and anti-inflammatory characteristics due to the presence of papain, chloramines and toluidine blue salts in a thickening medium [12]. Its mechanism of action is through breaking of the partially degraded collagen molecules, thereby contributing to the degradation and elimination of the fibrin mantle formed by the carious process. The key advantages of Papacarie™ are atraumaticity, biocompatibility, antibacterial properties, non-requirement of anesthesia, and better preservation of healthy tissue while removing the compromised tissue [13].
There has been an earlier attempt at meta-analysis by Marquezan and coworkers in 2006, comparing the efficacy of chemomechanical studies with conventional drilling technique for caries removal. An observation by Marquezan et al. was that the studies available then did not have power of evidence generation [14-17]. Considering the various systematic, randomized clinical trials published in recent years, it is highly significant to generate clinical evidence for the use of chemomechanical caries removal methods. The objective of the present systematic review is to compare the performance of chemomechanical CarisolvTM technique with conventional rotary drill method of caries removal, in terms of (i) the pain experienced or perceived by the patients, (ii) the need for anesthesia and (iii) patients’ preference of one method over the other. A secondary objective is to conduct a meta-analysis of the time for complete caries removal by CarisolvTM technique vs. conventional rotary drill method, based on randomized clinical trials published till date.
METHODOLOGY
A systematic search of original research articles, reviews and clinical studies on chemomechanical techniques of caries removal was undertaken. Published studies on the topic of comparison of techniques of caries removal were obtained based on a search of the PubMed, the Cochrane Central Register of Controlled Trials (CCTR93), Unbound Medline, Embase and Metapress databases, using the search terms ‘chemomechanical’, ‘caries removal’, ‘Carisolv™’, ‘Papacarie™’ ‘clinical’ and related keywords, and their combinations. The search included reports published in conference proceedings not currently listed in MEDLINE or other bibliographic databases. The search was restricted to articles published till October 2014 in the English language, by setting a language and period limitations during the search process.
All the processes of selection and evaluation of papers were performed by two expert reviewers. The selection of studies for the purpose of systematic review was performed in two stages. During the first stage of selection, as being ‘relevant’ or ‘not relevant’ (NR) to the objectives of the present review, based on the title and abstract sections. To be classified as ‘relevant’ and be eligible for inclusion in the second stage of selection process, a study was required to be an in vivo clinical study or trial of caries removal by mechanical or chemomechanical method, All types of in vitro studies of evaluation of the properties of caries extracted by mechanical or chemomechanical methods or restorations, comparative studies on different compositions of the gel used in chemomechanical methods, and studies in special groups of patients were classified as NR and were excluded from the second stage of selection process.
In the second stage, relevant studies were further evaluated using a Cochrane type quality assessment process based on a study of the full text of the article. Each study was assigned a risk of bias score of ‘Low risk’ (L) or ‘High risk’ (H), indicative of possible bias upon inclusion in the systematic review. Risk score of ‘L’ was assigned to randomized clinical trials (RCT), controlled clinical studies and comparative studies of rotary drill and CarisolvTM methods reporting the performance parameters of time for caries removal, need for anesthesia, pain perception and patient preference. A risk score of ‘H’ was given to non-comparative studies, in vitro studies and those using other caries removal methods and evaluating parameters other than those mentioned above. Additional stringent inclusion-exclusion criteria were applied to further shortlist studies for meta-analysis of time required for the removal of caries by conventional rotary drill vs. Carisolv™ technique.
Data on the type of study, demographic data of subjects in different groups, various performance parameters of the different techniques used for comparison, and their statistical significance were extracted from the included studies. Meta-analysis was performed based on two models: fixed effect and random effect model. Statistical measures of heterogeneity of data, Q and I2 were evaluated for the two techniques. Meta-analysis of the selected data was done using SAS® (SAS Institute Inc., Cary NC USA) and Microsoft Excel (Microsoft, Inc., Redmond WA USA) statistical analysis software.
RESULTS
The search of PubMed database yielded 79 unique studies, published until October 2014. A systematic search of the CCTR93 yielded 28 trials including five ‘Papacarie’ trials. International Association for Dental Research (IADR) Conference proceedings had a study reported in 2005, while Unbound Medline database yielded three studies. Similar search of Metapress, Google Scholar, ClinicalTrials.gov and some journals in dental research did not yield any other unique studies. A schematic flow chart of the literature search strategy is shown in Fig. (1). Search results from these databases were pooled and a significant number of studies were identified as duplicates were excluded.
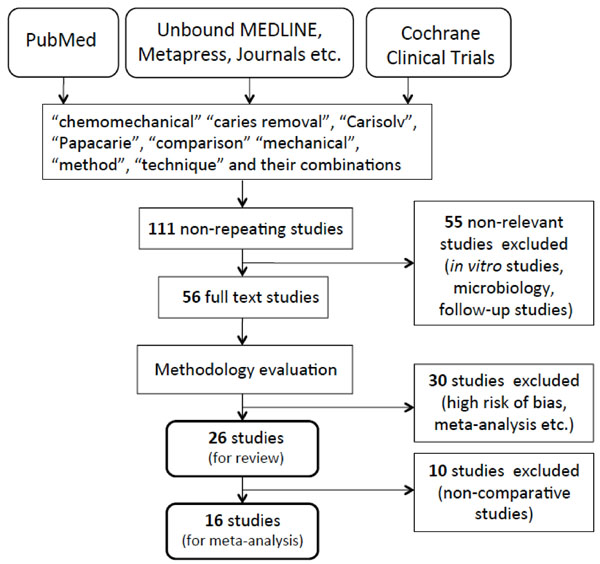
Flow chart of the literature search process.
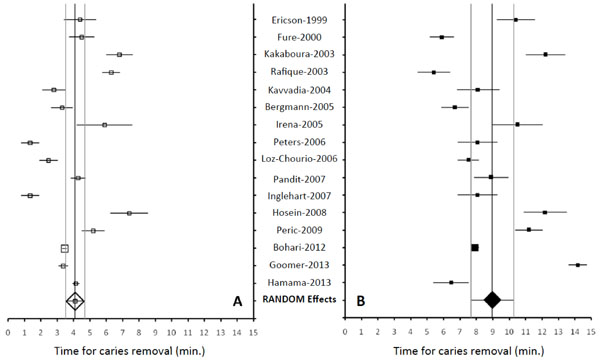
Distribution of time for caries removal by (A) rotary drill technique (open squares, Random effects model estimate (◊, 95% CI) and (B) Carisolv™ technique (filled squares, Random effects model estimate (♦, 95% CI).

Distribution of percentage of patients who perceived ‘No pain’ (A) or ‘some pain’ (B) during caries removal by rotary drill technique (open squares, mean -----, weighted mean ◊) and chemomechanical techniques (filled squares, mean ——, weighted mean ♦).
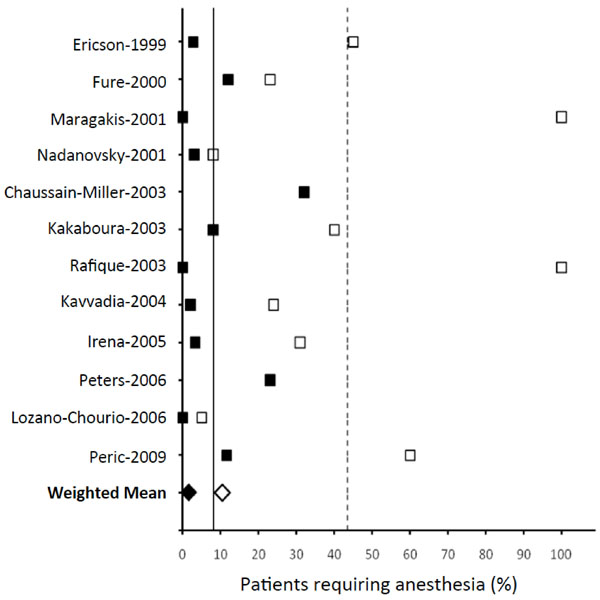
Distribution of percentage of patients who needed anesthesia during rotary drill technique (open squares, mean -----, weighted mean ◊) and chemomechanical techniques (filled squares, mean ——, weighted mean ♦).
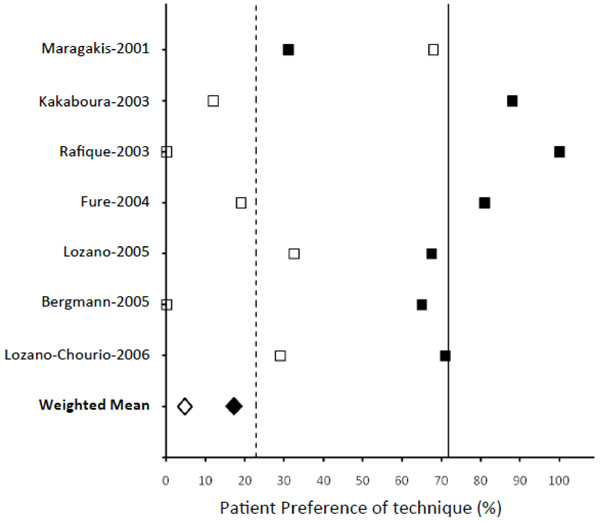
Distribution of patient preference to rotary drill technique (open squares, mean -----, weighted mean ◊) and chemomechanical techniques (filled squares, mean ——, weighted mean ♦).
Studies selected for systematic review, their salient features and extracted data.
| No. | Author-Year | Subjects | Type of Teeth | Rotary or Mechanical method | CarisolvTM | Other Measurements | Reason for non-inclusion in meta-analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Caries (N) | No. of Patients | Age range (y) (Mean ± SD) |
N | Time (m) (Mean ± SD) |
N | Time (m) (Mean ± SD) |
Measure | Technique | Mech. method | CarisolvTM | ||||
| 1 | Zinck-1988a (Caridex) |
114 | 57 | NA | Previously restored with secondary decay | 57 | (-)3.29 ± 0.65 | 57 | 3.03 ± 0.90 | Anesthesia needed | 21/57 (37%) | 12/57 (21%) | Older Caridex method Restored teeth removal Absolute time values not reported |
|
| 2 | * Ericson-1999 | 127 | 137 | 3-85 (35 ± 21) |
Mix of 4 types of teeth | 19 | 4.4 ± 2.2 | 106 | 10.4 ± 6.1 | Anesthesia needed | 9/20 (45%) | 3/107 (2.8%) | - | |
| Degree of pain | Patient survey | 1/11 'No pain' 9/11 ‘some pain’ |
58/104 'No pain' 44/104 ‘some pain |
|||||||||||
| 3 | * Fure-2000 | 60 | 38 | Primary root caries | 26 | 4.5 ± 2.0 | 34 | 5.9 ± 2.2 | Anesthesia needed | 6/26 (23%) | 4/34 (12%) | - | ||
| 4 | Maragakis-2001 | 32 | 16 | 7-9 (7.7 ± 0.7) |
Primary molars | 16 | 0.2 ± 0.05 | 16 | 6.85 ± 2.61 | Anesthesia needed | Patient survey | 16/16 (100%) | 0/16 (0%) | Method of measuring time for removal of caries is different |
| Patient preference | Patient survey | 11/16 (68%) | 5/16 (31%) | |||||||||||
| 5 | Nadanovsky-2001 | 132 | 66 | 6-44 | Permanent teeth | 66 | 8.6 ± 3.8 | 66 | 9.2 ± 3.8 | Anesthesia needed | 5/66 (8%) | 2/66 (3%) | Non-rotary method used, conventional spoon excavator method | |
| Pain perception | Patient survey | 43/66 (65%) ‘some pain’ |
21/66 (32%) ‘some pain’ |
|||||||||||
| 6 | Chaussain-Miller-2003 | 120 | 96 | 10-81 (35.9 ± 17.7) |
94 | 11.1 ± 9.51 | Anesthesia needed | 30/94 (32%) | Not a comparative study | |||||
| Pain perception | Patient survey | 68.3% ‘No pain’ | ||||||||||||
| 7 | * Kakaboura-2003 | 90 | 45 | 18-55 | 45 | 6.8 ± 2.8 | 45 | 12.2 ± 4.1 | Anesthesia needed | 40% | 8% | - | ||
| Patient preference | Patient survey | 12% | 88% | |||||||||||
| 8 | * Rafique-2003 | 44 | 22 | 13-75 | Contra lateral teeth | 22 | 6.3 ± 1.3 | 22 | 5.4 ± 2.4 | Anesthesia needed | 100% | 0% | - | |
| Patient acceptance | Patient survey | 0% | 100% | |||||||||||
| 9 | * Kavvadia-2004 | 92 | 31 | 2-9 (4.2 ± 1) |
Primary teeth | 27 | 2.8 ± 1.9 | 65 | 8.1 ± 5.3 | Anesthesia needed | Class V patient survey | 4/17 (24%) | 1/43 (2%)11 | - |
| 10 |
Fure-2004 |
202 | 170 | 19-85 | 104 98 | 6.7 ± 4.1 7.6 ± 4.2 |
Patient preference | Patient survey | 19% | 81% | Comparison of two different gels (Carisolv method) | |||
| 11 | * Balciuniene-2005j | 35 | 30 | 2.5-13 | Deciduous & Permanent | 30 | 5.9± 4.75 (1-20) |
30 | 10.5± 4.25 (3-20) |
Anesthesia needed | 9/29 (31%) | 1/30 (3.3%) | - | |
| Pain perception | Patient survey | 8/29 ‘No pain’ 15/29 ‘some pain’ |
14/30 ‘No pain’ 7/30 ‘some pain’ |
|||||||||||
| 12 | *Bergmann-2005 | 92 | 46 | 4-11 (8) |
Maxille /Mandibular molars (deciduous) | 46 | 3.3 ± 2.3 | 46 | 6.7 ± 2.9 | Pain perception | Patient survey | 18/46 ‘No pain’ 17/46 ‘some pain’ |
26/46 ‘No pain’ 17/46 ‘some pain’ |
- |
| Patient preference | Patient interview | 0% | 65% | |||||||||||
| 13 | * Peters-2006 | 50 | 6-11 (8.1) |
24 | 1.34 ± 1.4 | 26 | 8.06 ± 3.13 | Anesthesia needed | 6/26 (23%) | - | ||||
| Pain reported | 28% ‘some pain’ | |||||||||||||
| 14 | * Lozano-Chourio-2006 | 80 | 40 | 7-9 (7.7 ± 0.7) |
Primary Molars | 40 | 2.47 ± 1.83 | 40 | 7.51 ± 2.10 | Anesthesia needed | 2/40 (5%) | 0/40 (0%) | - | |
| Pain Perception | Patient survey | 24/40 ‘No pain’ 16/40 ‘some pain’ |
33/40 ‘No pain’ 7/40 ‘some pain’ |
|||||||||||
| Patient preference | 11/38 (29%) | 27/38 (71%) | ||||||||||||
| 15 | Magalhaes-2006,j | 30 | Molars | 30 | 3.61 ± 1.17 | 30 | 6.42 ± 2.62 | Knoop Hardness (KHN) | Micro-hardness Tester | Lower KHN at all distances | Non-rotary, hand excavation method | |||
| 16 | * Pandit-2007 | 150 | 75 | 6-9 | Deciduous teeth | 50 | 4.28 ± 1.67 | 50 | 8.9 ± 3.78 | Pain (Mean ± SD) | VAS | 4.24 ± 1.25 | 2.18 ± 1.12 | - |
| Pain (Mean ± SD) | VPS | 1.44 ± 0.91 | 0.08 ± 0.27 | |||||||||||
| Efficacy (Mean±SD) | 0.38 ± 0.75 | 0.42 ± 0.76 | ||||||||||||
| 17 | * Inglehart-2007 | 50 | 8.16 | 24 | 1.34 ± 1.4 | 26 | 8.06 ± 3.13 | Perceived pain (0-4) | Operator Survey | 2.42/4 (60.5%) | 2.77/4 (69.25%) | - | ||
| Satisfaction (0-5) | 4.00/5 (80%) | 2.62 (52.4%) | ||||||||||||
| Pain experience (0-100) | Patient Survey | 61.12 (61.12%) | 69.71 (69.71%) | |||||||||||
| Satisfaction (0-4) | 3.96/4 (99%) | 3.46/4 (86.5%) | ||||||||||||
| 18 | * Hosein-2008 | 60 | 30 | Mandibular molars | 30 | 7.4 ± 3.21 | 30 | 12.19 ± 3.7 | Incomplete removal | Clinical assessment | 0/30 (0%) | 3/30 (10%) | - | |
| 19 | * Peric-2009 | 120 | 120 | 3-17 (8.7 ± 3.0) |
60 | 5.2 ± 2.8 | 60 | 11.2 ± 3.3 | Anesthesia needed | 36/60 (60%) | 7/60 (11.6%) | - | ||
| Pain perception | Patient Survey | 10/24 ‘No pain’ 10/24‘some pain’ |
46/53‘No pain’ 5/53‘some pain’ |
|||||||||||
| Incomplete removal | Clinical assessment | 5/60 (8.3%) | ||||||||||||
| Patient satisfaction | Patient Survey | 28/60 (47%) | 51/60 (85%) | |||||||||||
| 20 | Sanjeet-2011 | 80 | 40 | 4-8 | Primary molars | 40 | 2.08 ± 0.38 | 40 | 5.48 ± 0.75 | Pain perception | Wong Baker Faces Pain Scale | 6.65 ± 1.89 | 1.525 ± 1.36 | Non-Carisolv, Papacarie method |
| Mean reduction in viable bacterialcount | Colony count | 87.94% | 81.12% | |||||||||||
| 21 | Anegundi-2012 | 60 | 30 | 4-9 | Primary molars | 30 | 4.68 | 30 | 17.96 | Pain perception | Patient Survey | 50% ‘No pain’ 46.7% ‘some pain’ |
86.7% ‘No pain’ 10% ‘some pain’ |
Non-Carisolv, Papacarie method |
| Patient preference | Patient Survey | 36.7% | 60% | |||||||||||
| Mean bacterial count | Colony count | 90.33 | 115.5 | |||||||||||
| 22 | * Bohari-2012 | 120 | 5-9 | 30 | 3.45 ± 0.37 | 30 | 7.91 ± 0.72 | Pain perception | FLACC Scale | 2.93 ± 1.74 | 1.13 ± 1.25 | - | ||
| Complete removal (%) | DIAGNODENT pen | 92.9 ± 9.2 | 87.7 ± 6.4 | |||||||||||
| 23 | Matsumoto-2012 | 40 | 20 | 5-8 | Deciduous molars | 20 | 1.73 ± 1.3 | 20 | 2.75 ± 0.8 | Pain perception | 10/20 ‘No pain’ 10 ‘some pain’ | 9/20 ‘No Pain’ 11 ‘some pain’ | Non-Carisolv, Papacarie method | |
| 24 | * Goomer-2013 | 150 | 80 | 6-10 | Primary molars | 50 | 3.37 ± 1.1 | 50 | 14.17 ± 2.03 | Pain (Mean ± SD) | VAS | 77.20 ± 19.8 | 20.40 ± 12.28 | - |
| Pain (Mean ± SD) | VPS | 2.72 ± 0.3 | 0.82 ± 0.83 | |||||||||||
| Efficacy (removal) | Clinical assessment | 0.48 ± 0.3 | 1.2 ± 0.83 | |||||||||||
| 25 | * Hamama-2013 | 32 | Molars | 8 | 4.14 ± 0.32 | 8 | 6.46 ± 1.57 | Vickers Hardness, 75mm | 79.16 ± 5.7 | 19.01 ± 2.5 | - | |||
| 26 | Motta-2013 | 40 | 20 | 4-7 | Primary teeth | 20 | 20 | Pain perception (Face scale) | 13/20 no pain 7 some pain | 18/20 no pain 2 mild pain | Non-Carisolv, Papacarie method | |||
* Studies selected for meta-analysis of time for caries removal by the two methodsNA Not available in the article
a Mean times adjusted for volume (residuals)
d value inferred from the abstract
h comparison of CarisolvTM and PapacarieTM methods
j Mean and/or SD was calculated using the reported median, range and N values
Meta-analysis and estimation of significance levels between methods.
| Study | Time required (Mean ± SD) (min) | P-Value | |
|---|---|---|---|
| Rotary or | Carisolv™ | ||
| Ericson-1999 | 4.4 ± 0.5 | 10.4 ± 0.59 | < 0.0001 |
| Fure-2000 | 4.5 ± 0.39 | 5.9 ± 0.38 | 0.0138 |
| Kakaboura-2003 | 6.8 ± 0.42 | 12.2 ± 0.61 | < 0.0001 |
| Rafique-2003 | 6.3 ± 0.28 | 5.4 ± 0.51 | 0.1295 |
| Kavvadia-2004 | 2.8 ± 0.37 | 8.1 ± 0.66 | < 0.0001 |
| Irena-2005 | 5.9 ± 0.87 | 10.5 ± 0.78 | < 0.0001 |
| Bergmann-2005 | 3.3 ± 0.34 | 6.7 ± 0.43 | < 0.0001 |
| Peters-2006 | 1.34 ± 0.29 | 8.06 ± 0.61 | < 0.0001 |
| Lozano-Chourio-2006 | 2.47 ± 0.29 | 7.51 ± 0.33 | < 0.0001 |
| Pandit-2007 | 4.28 ± 0.24 | 8.9 ± 0.53 | < 0.0001 |
| Inglehart-2007 | 1.34 ± 0.29 | 8.06 ± 0.61 | < 0.0001 |
| Hosein-2008 | 7.4 ± 0.59 | 12.19 ± 0.68 | < 0.0001 |
| Peric-2009 | 5.2 ± 0.36 | 11.2 ± 0.43 | < 0.0001 |
| Bohari-2012 | 3.45 ± 0.07 | 7.91 ± 0.13 | < 0.0001 |
| Goomer-2013 | 3.37 ± 0.16 | 14.17 ± 0.29 | < 0.0001 |
| Hamama-2013 | 4.14 ± 0.11 | 6.46 ± 0.56 | 0.0011 |
| Meta Analysis | |||
| Fixed Effect Model | 3.65 ± 0.05 | 8.65 ± 0.09 | < 0.0001 |
| I2 = 96.37 % | I2 = 97.72 % | ||
| Random Effect Model | 4.09 ± 0.29 | 8.97 ± 0.66 | < 0.0001 |
| I2 = 56.71 % | I2 = - 9.36 % | ||
A total of 111 non-repeating studies were evaluated on the basis of methodology and relevance to the objective of the present study, to select 56 studies during the first stage of selection. A total of 55 NR studies including in vitro microbiological, morphological, behavioral, radiographic, physiological, follow-up and micro-hardness studies were excluded from the present study. Among the NR studies were studies of restoration, residual caries and surface damage.
During the second stage of selection, risk of bias score was assigned to the 56 relevant studies. Twenty four studies received ‘H’ score for higher risk of bias while 32 studies were assigned as ‘L’ score. Out of the 32 low risk studies, six studies including two conference abstracts published later, and a previous meta-analysis were not selected. The final selection consisted of 26 papers and the data extracted from them are shown in Table 1.
Studies reporting the time required for the removal of caries by conventional rotary drill vs. Carisolv™ technique were shortlisted for meta-analysis. Non-randomized studies, studies with methods other than rotary and Carisolv™, and those with inadequate design (Galuscan et al. have not measured time and Kumar et al. have not used rotary method) were excluded from meta-analysis [18-21]. In addition, one study was excluded because of extreme heterogeneity of the data, probably due to difference in the method of measurement; two studies were excluded due to inadequate reporting of data (Mean and SD were not available) [22-24]. Seven other studies were excluded as non-relevant: one study for the use of hand tools for excavation, one using new gel for Carisolv™ technique, one study of Caridex system, one evaluated radiographically, and three studies for the use of Papacarie™ technique [25-31]. Studies by Irena et al. and Magalhaes et al. did not report the mean time and SD for removal of caries and these two parameters were calculated using the reported median and range, following the method of Hozo et al., before inclusion in the meta-analysis [32-34]. Subsequent to application of the inclusion-exclusion criteria, 16 studies were selected for meta-analysis.
A summary of the studies selected for meta-analysis and their salient characteristics are shown in Table 1. Twenty six studies tabulated were diverse in terms of age groups of subjects, type of teeth caries removed etc. Table 1 shows the data on characteristic performance parameters of the mechanical (rotary standard technique in most of the studies) and chemomechanical (Carisolv™ in all of the selected studies, except for five studies of Papacarie™) methods of caries removal. A comparison of these parameters will be useful to determine the merits of chemomechanical method over the conventional rotary method.
Time Required for Caries Removal
Twenty two of the 26 studies tabulated, report a difference in the time for caries removal by the two methods, which is statistically significant. Based on the inclusion-exclusion criteria mentioned above, 16 studies were included for meta-analysis with respect to time for caries removal. Fig. (2A and 2B) shows the Forest plots for time taken reported by these studies for the two techniques. The data are very heterogeneous as indicated by the very high values of the I2 statistic (fixed effects model) for the rotary drill (96.37%) as well as Carisolv™ (97.72%) techniques. The use of random effects model, appropriate for heterogeneous datasets, yields moderate I2 values of 56.71% for the rotary drill technique, and-9.36% for the Carisolv™ technique. The effect size (or mean time for removal of caries) for the rotary and Carisolv™ techniques, determined by the random effects model are 4.10 ± 0.29 (3.52-4.67 for 95% CI) and8.97 ± 0.66 min (7.67-10.27 for 95% CI), as indicated by the open and filled diamond symbols respectively. Similar to the observations of individual studies, these values are statistically significant (P <0.0001), to confirm that Carisolv™ technique takes longer time for caries removal. Complete details of the meta-analysis by the two models are given in Table 2.
Evaluation of Pain
Clinical measures of pain perceived, need for anesthesia and patient preference have been analyzed on the basis of weighted average of the data from selected studies. Fifteen studies have reported measure of degree of pain experienced by the patient during the procedure of caries removal. These results are consistent with the fact that rotary drilling method is more painful compared to the chemomechanical method. Pain experienced during the procedure is expressed in the patient surveys by the two options: ‘no pain’ or ‘some pain’ experienced by the patient. Although other options were also employed in some studies, majority of the subjects have used these options and the difference between the techniques is most pronounced with these options. These two patient responses have been analyzed separately, as shown in Fig. (3A and 3B). The simple mean of percentage of ‘no pain’ and ‘some pain’ responses for the rotary drill technique is shown by dotted lines and those for Carisolv™ are shown by solid lines in Fig. (3A and 3B). The weighted average for these responses in each case are represented by the open diamonds and filled diamonds for rotary and Carisolv™ techniques respectively. The case of ‘no pain’ responses, simple average value is very high for Carisolv™ (30.44% for rotary compared to 64.32% for the chemomechanical method), implying that more subjects did not experience pain with Carisolv™ technique. However, the weighted average for rotary technique is only slightly smaller (16.28) than that for Carisolv™ technique (17.12), indicating that there is no significant difference between the techniques. The difference between the techniques in terms of pain perceived is unequivocally demonstrated by considering the positive choice of ‘some pain’ experienced by the patient. A reverse of the earlier trend is true for ‘some pain’ responses – higher weighted average value for rotary technique (14.67) reflects that many subjects experienced pain with rotary drill and only a smaller number (6.76) experienced pain during Carisolv™ extraction.
Need for Anesthesia
Requirement of anesthesia during caries removal by the patients has been reported in 12 out of 27 selected studies. Majority of subjects assigned to rotary method opted for anesthesia as indicated by their percentage ranging from 23 to 60%, and occasionally to 100% of them have been treated under anesthesia [22, 35]. On the other hand, in most of the Carisolv™ studies, 0 to 12% of subjects opted for anesthesia and only in two studies, their proportion reached 20 to 30% [19, 36]. Distribution of subjects opting for anesthesia in various studies is shown in Fig. (4). The weighted mean of subjects for rotary technique is clearly higher (10.52%) than those opting for anesthesia during chemomechanical caries removal (1.59%). Less than 10% of the group population needed anesthesia in most of the chemomechanical studies, while >30% subjects are treated under anesthesia for the rotary technique.
Patient Preference
Patient surveys in the form of written questionnaire or interview by clinicians have been conducted after the caries removal process. Survey has been useful to quantify many subjective experiences about the process the patients have just undergone. Patients’ preference to one of these methods over the other may sum up these experiences. Patient preferences recorded in seven studies have been plotted as shown in Fig. (5), and analyzed using the weighted average of the percentage of subjects preferring each technique. In all studies, except one, more than 50% subjects preferred Carisolv™ technique to rotary and in two studies, none of the subjects preferred the rotary drill technique [22, 35, 37]. The weighted average of 18.68% for Carisolv™, which is higher than that for rotary drill (4.69%), confirms the trend.
DISCUSSION
The present meta-analysis of the comparative clinical studies of the mechanical and chemomechanical techniques of caries removal has shown that the time required for both methods was significantly different. Time for removal has been taken as the key parameter for meta-analysis, since there is significant heterogeneity in the reporting of other treatment parameters. Measures of pain perception, requirement of anesthesia and patient preference have been evaluated in fewer studies and by different scales and techniques, and hence, are not amenable for meta-analysis. The time required for complete caries removal is significantly more than that for conventional rotary drill, but the other advantages in terms of reduced pain and need for anesthesia outweigh the longer duration.
Although the time required for complete removal of caries by mechanical rotary drill as well as the chemomechanical Carisolv™ or Papacarie™ methods has been reported in 22 studies (Table 1), all these studies could not be included in the meta-analysis due to various reasons, explained above. It is clear from the meta-analysis that chemomechanical Carisolv™ technique takes longer duration for caries removal. Apart from the Carisolv™ studies considered for meta-analysis, few studies have compared the other chemomechanical Papacarie™ with rotary and / or Carisolv™ techniques. In a study by Kumar et al., Papacarie™ technique took a marginally less mean time of 10.48 ± 2.96 min. for caries removal compared to 11.67 ± 3.25 min. (P>0.05) for Carisolv™ technique [21]. Similar results have been obtained by Kotb et al. [29] and Kochhar et al. [38]. Matsumoto et al. did not find significant difference between the time taken by Papacarie™ Duo and low speed bur techniques [31].
Among the patient surveys of pain perception, only two of the most frequent options selected by the patients are used in the present study for further analysis. Responses for the complete absence of pain indicated by ‘no pain’, and presence of some tolerable pain indicated by ‘some pain’ have been consistently used by significantly higher number of patients for chemomechanical methods than for the rotary method. For rotary technique, the number of ‘no pain’ responses is usually below 30%, but in two studies, these responses were as high as 40-60%. [37, 39]. In the case of chemomechanical technique, ‘no pain’ responses were consistently above 50% and in two cases, as high as 75-85% [39, 40]. When the second option of ‘some pain’ is considered, the trend becomes clear in that responses for the Rotary range from 40-65% while those for Carisolv™ method ranges from 15-30%.
Inglehart et al. have used both operator and patient surveys for the evaluation of pain experienced during caries removal by the two methods [41]. The operator perceived pain was scored on a scale of 0-4, whereas patients rated their pain experience on scale of 0-100. In their study, average pain experienced during the rotary technique was only slightly less (60%) than the chemomechanical method (69%). Interestingly, both the operator and patients arrive at similar values for the pain experienced by the two methods, in spite of the difference in evaluation methods.
Evaluation of pain using structured pain scales by trained clinicians is expected to yield a better estimate of pain experience, instead of patient surveys, as individual tolerance to pain may influence patient response to the survey. Pain evaluation has been carried out using Visual Analog Scale (VAS) and Verbal Pain Scale (VPS) by Pandit et al. and Goomer et al., using Wong Baker Faces Pain Scale by Sanjeet et al., and using the FLACC (Face, Leg, Activity, Cry, Consolability) scale by Bohari et al. [30, 42-44]. Once again, pain experienced during Carisolv™ method ranks consistently lower than rotary drill method, irrespective of the scale used. However, when mean values of pain by VAS scale across studies are compared, Goomer et al. report a very high 77.20 ± 19.8 compared to 4.24 ± 1.25 reported by Pandit et al. [42-45]. Overall, pain experience by the rotary drill method is clearly higher than the Carisolv™ method.
Thirteen of the selected studies have determined the number (or percentage) of patient who were given or opted for anesthesia during caries removal by the two techniques. Of these, Chousian-Miller et al. [19] did not report a value for the rotary drill method as it is a non- comparative study of Carisolv™ method alone. The extent of pain experienced and/or the fear of patients, especially children, for the rotary drill method is indicated by the percentage of them opting for anesthesia for the procedure. Out of the 11 studies reporting this measure, in nine studies >25% of the patients needed anesthesia and in two of the studies, 100% of the patients were treated under anesthesia. On the other hand, requirement of anesthesia for the chemomechanical method is much lower, as indicated in Table 1. In twelve studies (out of the 13) where Carisolv™ was used,<2 5% of the subjects needed anesthesia and in the remaining study also, the number was a moderate 32%. None of the subjects required anesthesia in studies by Maragakis et al., Rafique et al. and Lozano-Chourio et al., while<5% were given anesthesia in studies by Ericson et al., Nadanovsky et al., Kavvadia et al. and Irena et al. [22, 25, 32, 35, 39, 46-49]. All of these observations go a long way to establish Carisolv™ as a mild and non-traumatic technique for caries removal, especially in children.
In eight of the selected studies, subjects answered a questionnaire or were interviewed after the treatment, about their experience with the two techniques and their preference to one technique over the other. Patient ‘preference’ has been differentiated from ‘patient acceptance’ reported by Rafique et al. and ‘patient satisfaction’ reported in two other studies. [35, 40, 41] In the present analysis, only patient preference measured as a percentage of that specific group population was included. The distribution of patient preferences for the chemomechanical over the rotary drill technique is indicated in Fig. (5). Chemomechanical method clearly stands out as the most preferred, based on the higher weighted average value compared to that for rotary drill technique.
CONCLUSION
In summary, the present systematic review and meta-analysis have established that Carisolv technique has relatively superior performance in terms of the need for anesthesia, pain experience by the patients and preference over other methods, in spite of taking longer time for caries removal. Many randomized controlled studies of chemomechanical techniques have been published over the last decade. Time for removal is the only parameter that could be compared by the current meta-analysis. Comparison of other important clinical parameters of pain perception or pain experienced by robust methods is essential to strengthen the evidence for the use of chemomechanical techniques [50]. In comparison to the studies considered for meta-analysis by Marquezan et al., the quality of studies has improved in recent times, but sample sizes are very small in many studies (especially Hamama et al.). [17, 45] In spite of these limitations, chemomechanical technique stands out as a minimally invasive and preferred method compared to conventional rotary drill, based on the analyses done here. Chemomechanical caries removal techniques, being non-traumatic and least-injurious to healthy tooth structure, hold excellent promise for future dental practice [51].
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


