All published articles of this journal are available on ScienceDirect.
Iatrogenic Damage to the Periodontium Caused by Endodontic Treatment Procedures: An Overview
Abstract
The tooth, the pulp tissue within it and its supporting structures should be viewed as one biologic unit. The interrelationship of these structures influences each other during health, function and disease. The interrelationship between periodontal and endodontic diseases has aroused much speculation, confusion and controversy. The endodontium and periodontiumare closely related and disease or damage of one tissue may lead to the involvement of the other.
INTRODUCTION
The primary objective of endodontic treatment is to preserve the teeth. The pulpal space biomechanical preparation, root canal sterilization, and obturation are the three important steps of endodontic treatment [1]. During endodontic treatment, numerous endodontic treatment failures occur due to improper treatment and bacterial reinfection. [2].
The most common types of errors that affect the periodontium during the endodontic treatment procedures are [3].
- Main cause of gingival necrosis or periodontitis is insufficient arsenic use,
- A perforation of the posterior tooth during root canal exploration,
- Root canal broken instrument,
- Overextension of filling substance overpassing the apical foramen (overfilling).
One of the most important processes in endodontic treatment is the obturation or filling of the root canal. Over passing of the apical foramen by the filling substance will have its adverse effects on the periodontium.
OVERFILLING CAUSE AND EFFECT
The occurrence of overloading caused by a filling substance with a soft consistency /texture such as paste or cement e.g. paraformaldehyde, AH26, Hydron, Diaket-A and zinc oxide eugenol or a solid consistancy such as guttapercha or silver cones can present bad reactions/effects to patients. Sometimes, the reaction is minor or in light signs such as short-term inflammation, but eventually it can also give damaging effects of overfilling, by unavoidably deforming the adjacent tissue permanently [4].
It is recognized that the success rate of endodontic treatments decreases when overfilling occurs. There are several factors to cause overfilling: too much cement in the root canal, unprecise working length measurement, no X-ray photo prior, during, and after the treatment process, over-instrumentation, excessive pressing to filling substance, resistency disappearance due to insufficient root canal preparation, the use of injection technique to fill the root canal, improper apical seal and operator’s lack of skill [5].
The effect of overfilling is varied (Figs. 1, 2), determined by the filling substance, filling substance’s quantity which passes the apical foramen, and how far the filling substance surpasses the apical foramen. Based on these three factors, the most common effects of overfilling are inflammation reaction of the periapical tissue causing severe pain accompanied by swollen tissue, periodontal ligament breakage, and a periapical lesion [6]. Other effects are necrosis of alveolar bone in the periapical area of the discoloration mucosa membrane covering tooth apex, or even a neurological difficulty such as paraesthesia.
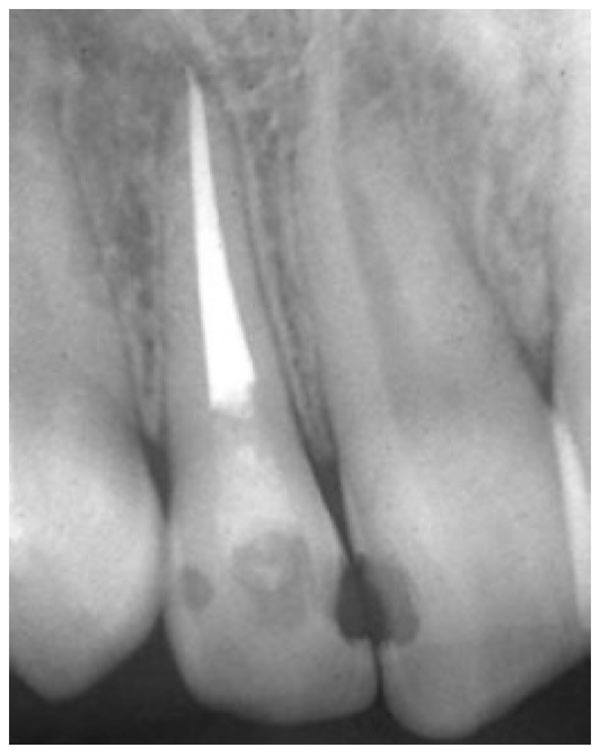
Periapical radiograph shows overfilling: zinc oxide eugenol, inflicting severe pain to patients.
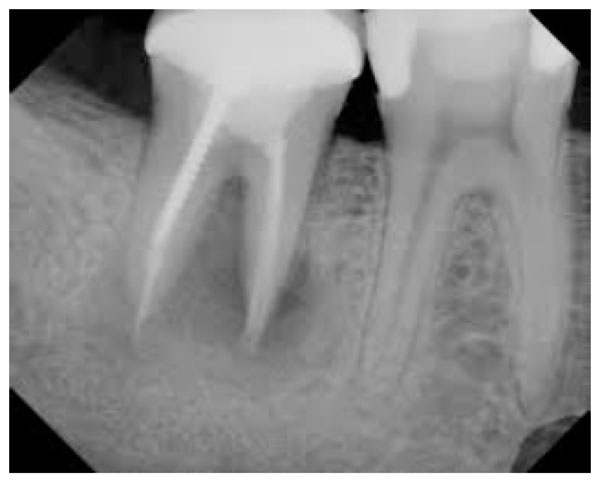
Iopa of second molar of the lower jaw shows overfilling with guttapercha cone causing abscess and paresthesia.

Perforation of the pulp chamber.

Root fractures.
As with any therapeutic modality, complications may arise during endodontic treatment. Tschamer, Kaufman and Rosenberg [7] found that the effect of overfilling the root canal with paraformaldehyde will damage the periodontal ligament. Whereas Heling et al. and Tal et al. Kaufman and Rosenberg reported several cases in which overfilling with sealer containing paraformaldehyde resulted in alveolar bone necrosis [8].
Two significant mechanisms have been described by some authors for the damage to the nerve fibers after an overfilling of the root canal causing paresthesia. The first mechanism is due to chemical effect as a result of overfilling of either one or more components leading to neurotoxic damage to the nerve and its fibers. The second mechanism is due to a mechanical effect which occurs when filling substance is excessively pressed or pushed damaging the nerve and its fibers [9]. It was reported that permanent nerve damage would occur if contact occurs between phenol (or its derivatives) and the nerve for several weeks period [10]. And it would take a longer period of time even if healing occurs later [11]. Besides, the healing process could take place only if the regeneration process of the nerves is not obstructed by the scarred tissue [12]. In dentistry, eugenol is a phenol derivate which is in use since a longer period of time. It has a local anesthetic effect and is able to penetrate tissues resulting in protein coagulation. Eugenol’s ability to coagulate the protein can produce permanent nerve damage if the contact happens with enough concentration for several weeks [13]. Yet, it was reported that a spontaneous nerve healing process occured in 4-12 months in several cases of overfilling with eugenol contained filling substance [14].
SOME OF IATROGENIC NATURES ARE
Perforations of the floor of the pulp chamber or root during access (Fig. 3), canal instrumentation or preparation for a post.
These accidents may result in periodontal defects and treatment should be given as soon as the perforation occurs. The healing of the periodontal lesion depends on whether the bacterial infection can be excluded from the wound by obturation of the site of perforation. If a perforation occurs in the cervical portion of the tooth, a surgical flap approach provides enough access to expose perforation and allow a successful seal. But a guarded prognosis is given for such tooth as the lateral perforation is difficult to seal. Additional problems are root resorption and vertical root fracture.
Resorption may be internal or external. External resorption may follow impact injuries such as luxation or tooth avulsion and is most commonly seen after re-implantation. Vertical root fractures are oriented more frequently longitudinal towards the apex of the tooth. Cause and prevalence of such fracture is not established. However, such fractures can occur curing canal obturation, pin or post placement, or cementation of intra coronal restorations. In same cases they appear to occur spontaneously. They occur most commonly in endodontically treated teeth than non-treated teeth, as endodontically treated teeth become more brittle and less resistant to forces of mastication. These may occur years after treatment and may not be visible in the radiographs unless the fragments are separated.
It has been suggested that thin, halo like apical radiolucency is an indication of vertical root fracture (Pitts DL et al. 1983). Fracture is often inferred from symptoms of pain or tenderness on mastication or the development of a localized periodontal defect or sinus tract that cannot be explained by other clinical findings. Vertical fractures have a hopeless prognosis for the affected root.
ROOT FRACTURES
Root Fractures (Fig. 4) caused by traumatic forces or restorative endodontic procedures may lead to periodontal involvement through an apical migration of plaque along the fracture when the fracture originates coronal to the clinical attachment and is exposed to the oral environment.
Cervical Root Resorption and cemental tears: Cervical root resorption and cemental tears may lead to periodontal destruction when the lesion communicates with the oral cavity and allows bacteria to migrate subgingivally.
CEMENTAL TEARS
Structural and functional integrity of root surfaces is an essential prerequisite for the long-term preservation of periodontal health [15]. In this context, local anatomic root surface alterations may have a intense effect on gingival health, as they are considered to be plaque retentive niches. However, it is widely accepted that a susceptible host and site are also required before periodontal disease progression can occur in the presence of pathogenic bacteria [16]. Unexpected periodontal disease progression may therefore be dependent on the simultaneous existence of a number of primary and secondary factors.
Among the latter, enamel projections or pearls, root grooves/concavities, root fractures, and cervical root resorptions represent major tooth related factors, which may contribute to or predispose to the development of localized periodontal tissue breakdown. Cemental fractures represent a rare root surface alteration, which also fall into this group of developmental or acquired deformities and conditions and are referred to as cemental tears in the literature. A recent multicenter study examined 71 teeth with cemental tears that were confirmed by direct inspection or histological examination [17]. The study showed that 56.3% of the cases were detectable on preoperative radiographs and that these teeth were indeed more likely to have periodontal bone destruction (85.9%).
The diagnosis of a cemental tear is always difficult. The periodontal problems, which arise suddenly after successful endodontic re-treatment could be related to the radiographically distinguishable disintegration of the root surface, resulting in a cemental tear. According to Lin and co-workers the clinical signs such as tissue swelling, narrow deep pocket formation, the presence of a radiopaque fragment on the root surface and the related periodontal/periapical bone destruction are major features of teeth with cemental tears. The removal of the detached fragment and/or the mechanical root surface modification to achieve a smooth and unaltered root surface is a prerequisite for any surgical treatment.
CONCLUSION
Clinicians should bear in mind the consequences of reckless and unplanned treatment because in the process of eliminating one problem, there may be an occurrence of another with greater consequences in terms of tooth loss. Therefore, a thorough understanding of the local factors that a tooth is subjected to in the oral environment and their early correction can aid in preventing a number of cases that would become hopeless at a later stage.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


