All published articles of this journal are available on ScienceDirect.
Iatrogenic Damage to the Periodontium Caused by Implants and Implant Treatment Procedures
Abstract
A dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor.Well planned, comprehensive treatment plans lead to successful implant treatment and patient satisfaction, which are the eventual long-term objectives. Probability of implant success can be put at jeopardy by absolute and relative risk factors.
INTRODUCTION
An alternate treatment for replacing a missing tooth is a dental implant. An implant is a titanium screw that is placed in the area of the missing tooth.
The implant stabilizes and becomes a prosthetic root as the bone around the implant heals and “integrates” into the threads of the screw. Three months afterthe placement of the new root, a series of molds are created of the implant. A crown is then made and cemented to the new root, restoring full esthetics and function to the area. Majority of implant cases are successful leading to the most expected result in dentistry today.
During implant placement surgical complications are very common. According to a retrospective study by McDermott et al. 677 patients (2379 implants) were examined, and an overall frequency of complications was 13.9% [1]. Inflammatory and prosthetic complications were 10.2% and 2.7%, respectively whereas operative complications made up a mere 1%. Complications are anticipated and can lead to poor treatment outcomes.
PERI-IMPLANT MUCOSITIS
The clinical features of peri-implant mucositis (Figs. 1, 2) are in many respects similar to those of in gingivitis at teeth and include classical symptoms of inflammation, such as swelling and redness. Bleeding on probing (BoP) is a good discriminating indicator of peri- implant mucositis. The prevalenceof this disease remains difficult to estimate since data on BoP at implants are infrequently reported [2]. In a study on 25 subjects treatedwith implant-supported fixed prosthesis, Lekholm et al. reported that bleeding on probingoccurred at 80% of theimplants [3]. Roos-Jansaker et al. examined 987 implants in 216 patients and reported that more than 73% of all implants exhibitedbleeding on probing [4]. Higher frequenciesof bleeding on probing at implants were presented by Fransson et al. in a study on 82 subjects. It was reported that bleeding on probingoccurred in more than 90% ofimplant sites [5].
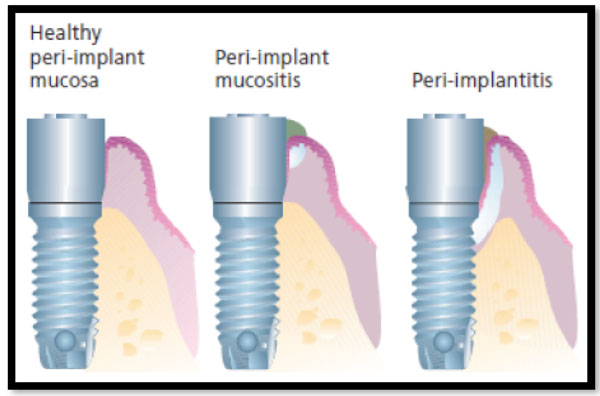
Schematic drawing illustrating healthy peri-implant mucosa, peri-implant mucositis, and peri-implantitis.
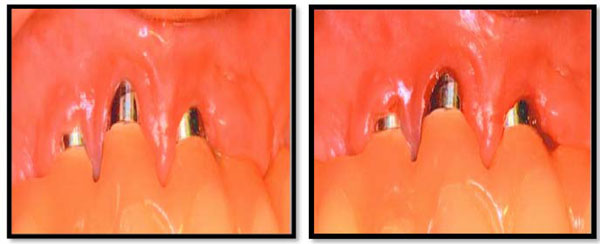
Clinical symptoms of peri-implant mucositis including varying signs of redness and swelling. (b) Probing resulted in bleeding from the margin of the mucosa.
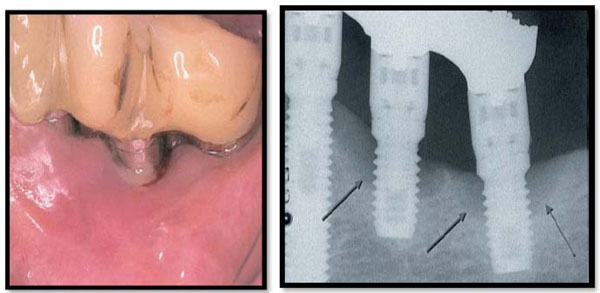
Clinical (a) and radiographic (b) characteristics of two implant sites with peri- implantitis in the left side of the mandible. Note the presence of swelling and suppuration in the peri-implant mucosa (a) and the crater-formed bone destruction around the implants in the radiograph (arrows) (b). Peri-implantitis lesions are poorly encapsulated, extend to the marginal bone tissue and may, if they are allowed to progress, lead to the loss of the implant.
Zitzmannetal [6] studied the response toplaque formation in the soft tissues at implant andtooth sites in humans. Twelve subjects with healthy periodontal and peri-implant conditions were asked to refrain from tooth/implant cleaning for a period of 3 weeks. Clinical examinations were performed and soft tissue biopsies were harvested prior to andat the completion of the plaque accumulation period. Thetissues were examined using histologic techniques.
It was established that plaque buildup was related with clinical signs of soft tissue inflammation.
Furthermore, the initially minutelesions in the gingiva and in the peri-implant mucosa markedly increased in size after 3 weeks of plaque build-up: from 0.03 mm2 at baseline to 0.3 mm2 (gingiva) and 0.2 mm2 (peri-implant mucosa). In addition, the proportion of B cells and neutrophils increased more in the lesion in the gingiva than in its counterpart in the peri-implant mucosa.
PERI-IMPLANTITIS
Peri-implantitis represents a clinical condition that includes the presence of an inflammatory lesion in the peri-implant mucosa and loss of peri-implant bone. The assessment of the diagnosis peri-implantitis must consequently require detection of both bleeding on probing (BoP) as well as bone loss in radiographs. Peri-implantitis initially affects the marginal part of the peri-implant tissues and the implant may remain stable and in function for varyingperiods of time. Implant mobility is therefore not an essential symptom for peri-implantitis but may occur in a final stage of disease progression and indicates complete loss of integration. Symptoms of peri-implantitis relate to the infectious inflammatory nature of the lesion. Thus, there is radiographic evidence of bone loss and the bone loss often has the shape of a crater. Swelling and redness of the mucosa as well as bleeding on gentle probing occur. Suppuration is also a frequent finding. The implant may remain stable over long periods.If left untreated, however, peri-implantitis may progress and lead to implant loss. Symptoms of peri-implantitis (Fig. 3) relate to the infectious inflammatory nature of the lesion. Thus, there is radiographic evidence of bone loss and the bone loss often has the shape of a crater. Swelling and redness of the mucosa as well as bleeding on gentle probing occur. Suppuration is also a frequent finding. The implant may remain stable over long periods.
The large numbers of neutrophils in the peri-implantitis lesion and the absence of an epithelial lining between the lesion and the biofilm, indicate that the peri-implantitis lesions have features that are different from those of periodontitis lesions. Progression of peri-implantitis is more pronounced at implants with rough surfaces than smooth surfaces.
CONCLUSION
Most of the factors that lead to implant failure can be controlled by the dentist by means of proper treatment planning.Surgical implant complications are common and should be managed immediately. Surgical implant complications may be iatrogenic, due to poor treatment techniques, or lack of understanding between dental disciplines. Adequate treatment plan must be accomplished in the implant “planning” stages, such as tracing preoperative radiographs, measuring models, taking CT scans and making proper surgical guides. Basic anatomy must not be forgotten and should be reviewed by the surgeon in every case.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


