All published articles of this journal are available on ScienceDirect.
Iatrogenic Damage to the Periodontium Caused by Radiation and Radiotherapy
Abstract
The radio-sensitivity of a tissue or organ is measured by its response to irradiation. Loss of moderate numbers of cells does not affect the function of most organs. However, with loss of large numbers of cells, all affected organisms display a clinical result. The severity of this change depends on the dosage and thus the extent of cell loss. Moderate doses to a localized area may lead to repairable damage. Comparable doses to a whole organism may result in death from damage to the most sensitive systems in the body.
INTRODUCTION
In dentistry, the size of the doses used routinely is relatively small and well below the threshold doses required to produce the somatic deterministic effects. However, the somatic and genetic stochastic effects can develop with any dose of ionizing radiation. Dental radiology does not usually involve irradiating the reproductive organs, thus in dentistry somatic stochastic effects are the damaging effects of most concern.
HOW DO X-RAYS CAUSE DAMAGE
The precise mechanism of how X-rays cause these damaging effects is not yet fully known, but two main mechanisms are thought to be responsible.
• Direct damage to specific targets within the cell
• Indirect damage to the cell as a result of the ionization of water or other molecules within the cell.
Direct Damage
Specific targets within the cell, probably the chromosomal DNA or RNA in the nucleus, take a direct hit from an incoming X-ray photon, or an ejected high-energy electron, which breaks the relatively weak bonds between the nucleic acids. The subsequent chromosomal effects could include.
• Inability to pass on information
• Abnormal replication
• Cell death
• Only temporary damage - the DNA being repaired successfully before further cell division.
If the radiation hits somatic cells, the effects on the DNA (and hence the chromosomes) could result in a radiation-induced malignancy. If the damage is to reproductive stem cells, the result could be a radiation-induced congenital abnormality. What actually happens in the cell depends on several factors, including:
• The type and number of nucleic acid bonds that is broken
• The intensity and type of radiation
• The time between exposures
• The ability of the cell to repair the damage
• The stage of the cell's reproductive cycle when irradiated.
Indirect Damage
As 75% of each cell consists of water, it is the water molecules that are most likely to be ionized by the incoming X-rays. The effects are shown below which illustrates that the damage to the cell results from the free radicals produced by the ionization process (Fig. 1).
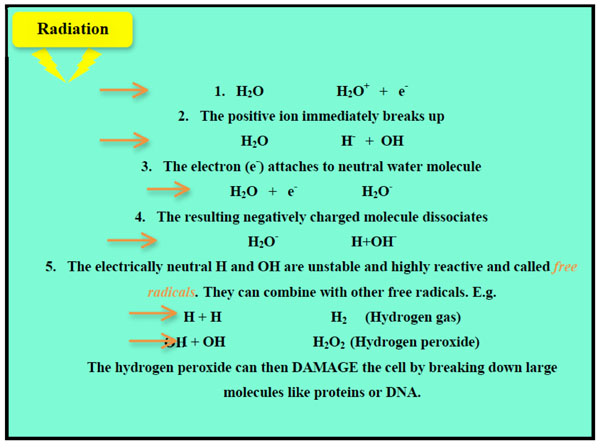
A diagrammatic summary of the sequence of events following ionization of water molecules leading to indirect damage to the cell.

Radiation effects on human submandibular salivary glands. A-Normal gland. B- A gland 6 months after exposure to radiotherapy. Note the loss of acini and presence of chronic inflammatory cells. C-A gland 1 year after exposure to radiotherapy. Note the loss of acini and extensive fibrosis.

Retarded development of the mandibular second premolar crowns with stunting of the mandibular incisor, canine, and premolar roots at 9 years.

Radiation caries. Note the extensive loss of tooth structure in both jaws resulting from radiation-induced xerostomia.
SHORT-TERM EFFECTS OF RADIATION
The short-term effects of radiation ona tissue are determined primarily by the sensitivity of its parenchymal cells. If continuously proliferating tissues (e.g., bone marrow, oral mucous membranes) are irradiated with a moderate dose, cells are lost primarily by mitosis-linked death. The extent of cell loss depends on damage to the stem cell pools and the proliferative rate of the cell population. The effects of irradiation of such tissues become apparent relatively quickly as a reduction in the number of mature cells in the series. Tissues composed of cells that rarely or never divide (e.g., muscle) demonstrate little or no radiation induced hypoplasia over the short term.
Long-term Effects of Radiation
The long term deterministic effects of radiation ontissues and organs depend primarily on the extent of damage to the fine vasculature. The relative radio-sensitivityof capillaries and connective tissue is intermediate between that of differentiating intermitotic cells and reverting postmitotic cells. Irradiation of capillaries causes swelling, degeneration, and necrosis. These changes increase capillary permeability and initiate a slow progressive fibrosis around the vessels. As a result, deposition of fibrous scar tissue is increased around thevessels, leading to premature narrowing and eventual obliteration of vascular lumens. This impairs the transport of oxygen, nutrients, and waste products and results in death of all cell types. The net result is progressive fibro-atrophy of the irradiated tissue. Such progressive atrophic changes lead to a loss of cell function and a reduced resistance of irradiated tissue to infection and trauma. These cellular changes are the basis for long-term radiation-induced atrophy of tissues and organs. Death of parenchymal cells after moderate exposure is thus the result of mitotic linked death of rapidly dividing cells in the short term and the consequences of progressive fibro-atrophyon all cell types over time.
GENERAL GUIDELINES ON PATIENT CARE
• For intraoral radiography the patient should be positioned comfortably in the dental chair, ideally with the occlusal plane horizontal and parallel to the floor. For most projections the head should be supported against the chair to minimize unwanted movement. For intraoral radiography the patient should be seated comfortably in the dental chair, ideally with the occlusal plane horizontal and parallel to the floor. For most projections the head should be supported against the chair to minimize unwanted movement. Some clinicians elect to X-ray their patients in the supine position along with most other dental surgery procedures. All techniques need to be modified accordingly, but it can sometimes be more difficult to assess angulations and achieve accurate alignment of film and tubehead with the patient lying down.
• For extraoral views the patient should be reassured about the large, possibly frightening or unfriendly-looking equipment, before being positioned within the machine. This is of particular importance with children.
• The procedure should be explained to the patients in terms they can understand, including warning them not to move during the investigation.
• Spectacles, dentures or orthodontic appliances should be removed. Jewellery including earrings may also need to be removed for certain projections.
• A protective lead thyroid collar, if deemed appropriate for the investigation being carried out, should be placed on the patient.
• The exposure factors on the control panel should be selected before positioning the intraoral film packet and X-ray tube head, in order to reduce the time of any discomfort associated with the investigation.
• Intraoral film packets should be positioned carefully to avoid trauma to the soft tissues taking particular care where tissues curve, e.g. the anterior hard palate, lingual to the mandibular incisor teeth and distolingual to the mandibular molars.
• The radiographic investigation should be carried out as accurately and as quickly as possible, to avoid having to retake the radiograph and to lessen patient discomfort.
• The patient should always be watched throughout the exposure to check that he/she has obeyed instructions and has not moved.
PERIODONTAL CHANGES IN PATIENTS UNDERGOING RADIOTHERAPY
Cancer is currently the cause of 12% of all deaths worldwide andis animportant global health problem with more than 10 million new cases and 6 million deaths each year worldwide [1].
Among them, head and neck neoplasia (HNN) is a major form of cancer in India, accounting for 23% of all cancers in males and 6% in females; Depending upon the sub-site of origin and the clinical extent of the disease the 5 -year survival varies from 20% to 90% [2].
The three most common modalities used in head and neck cancer treatment are surgical resection, radiotherapy and chemotherapy, either used singly or in combination. While these modalities are effective in eliminating the tumor, they also adverselyaffect the normal head and neck structures surrounding the tumor.
Radiation therapy has cytotoxic effects on both normal cells and malignant cells.
Direct damage to the oral structures (soft and hard tissue) commonly occurs from radio- and chemotherapy, and indirect damage may also occur from systemic toxicity. These oral complications may arise during and following cancer treatment and are commonly grouped into two broad categories: acute and chronic [3].
The reported acute oral complications are mucositis, xerostomia, dysphagia, dysguisia, and opportunistic infections, and chronic complications such as trismus, irradiation caries, osteoradionecrosis, and changes in periodontal attachment.
The long-termeffects comprise alteration in vascularity of soft tissue and bone, salivary gland damage, reduction in cellularity of connective tissue, and risk of increased collagen synthesis which results in fibrosis [4].
Radiation treatment induces obliterative end- arteritis that results in the soft tissue ischemia and fibrosis while the irradiated bone become hypovascular and hypoxic [5].
The peridontium is sensitive to the effect of radiation at high doses.
Diminished vascularity and cellularity of the periodontal ligament membrane with widening of periodontal space,thickening, rupturing, and disorientation of Sharpey′s fibers have been reported [6].
The direct and indirect effect of high-dose radiotherapy (RT) on the periodontium results in greater risk of periodontal attachment loss and tooth loss and greater risk for the development of osteoradionecrosis [7]. The extensive periodontal destruction may occur in the absence of good oral hygiene. Periodontitis in patients scheduled for head and neck radiotherapy results in acute and chronic complications such as osteoradionecrosis. Maintenance of good oral hygiene in patients undergoing radiotherapy may reduce morbidity of the known oral and periodontal side effects. Patientslated to receive the head and neck radiation therapy need dentalconsultation at the earliest possible time. Pre-irradiation treatment depends on patient prognosis, compliance, and residual dentition, in addition to fields, ports, dose and, immediacy of radiotherapy.
Diseases of teeth and supporting structures are a worrying finding in a patient about to undergo tumoricidal radiotherapy for a malignant condition in the maxillofacial region because oral pain and infection are common and a potentially serious sequence to radiotherapy for head andneck tumors in patients with healthy mouth.
The loss of integrity of the gingival crevicular tissues, as a result of periodontitis and radiotherapy induced thinning of these tissues together with xerostomia, mucositis, altered diet, and poor oral hygiene that often follow high-dose radiotherapy to the jaws, can create oral problems that affect the quality of life, which can cause interruption to cancer therapy [8].
The periodontal blood vessels are affectedby radiation leading towidening of periodontal ligament space and destruction of bony trabeculae which may result in increased risk of periodontal disease and altered healing with diminished capacity for bone remodeling and repair [9].
Llory et al. in 1972 showed a radiation-induced downshift of periopathogens [10]. Markitziu et al. [11] in 1992 and Leung et al. [12] in 1998reported that due to radiation-induced hypo-salivation and a concomitant increase in plaque accumulation and shift in oral micro florathe risk of periodontal infection is also increased Fig. (2). Shwarze et al. in 1999found a greater number of shallow periodontal pockets in radiated patients [13]. The reduced probing pocket depth does notindicate the histologicalpocket depth since the probe generally penetrates coronal level of junctional epitheliumdue to inflammation of underlying connective tissue or may be due to disparity between probing technique, probing force, or angle of insertion of the probe. Studies by Epstein [14] and Yusuf and Bakri [15] showed that direct and indirect effects of high dose of radiotherapy on periodontium resulted in increased attachment loss. Marx et al. in 1987 reported that generally increasing the doses of irradiation above 7000 rads carries the risk and severity of osteoradionecrosis [16].
Marciani et al. in 1992 reported that dosage can indicate potential irradiation injury [17]. Smaller irradiation doses administered at higher dose rates may be more injurious than higher doses dispensed at lower dose rates. Marques et al. in 2004 stated thatradiotherapy canadd to a greater or lesser degree to progression of attachment loss [18]. Oral mucositis is the most distressing of all the complications following head and neck radiotherapy.
Damage to oral mucosa is intenselyassociated with radiation dose, fraction size, volume of irradiated tissue, fraternization scheme, and type of ionizingradiation.
The severe mucosal reaction to radiotherapy is a result of mitotic death of epithelial cells, since the cell cycle time of the basal keratinocytes is about 4 days.
There is an increased gingival recession observed after radiotherapywhich may be due to changes invascularity and cellularity of periodontal ligament and hypovascular, hypocellular, and hypoxic changes in alveolar bone. In the absence of good oral hygiene rampant periodontal destruction may occur.
The gingival recession associated with radiotherapy is mainly due to reduction in gingival blood flow and alteration in immune response. The gingival recession represents loss of attachment, which is an indicator of disease progression.The gingival recession may lead to sensitivity, dental caries, and difficulty in maintenance of oral hygiene.
The inflammatory and degenerative changes of ionizing radiation on the salivary gland parenchyma, especially the serous a cinar cells leads toxerostomia.
Xerostomia has the potential to affect mastication, speech, and patients′ overall quality of life [19].
Difficulty in swallowing is encountered because the reduction in salivary flow diminishes lubrication and liquefaction of food, and irritation of mucosa makes chewing painful. Irradiation also causes fibrosis and atrophy of muscles in the pharynx.
EFFECTS OF IRRADIATION ON TEETH
Irradiation of teeth with therapeutic doses during their development severely retards their growth. Such irradiation may be for local disease (e.g., eosinophilic granuloma) or a generalized condition (leukemia being treated with whole-body irradiation followed by bone marrow transplantation). If it occurs before calcification, irradiation may destroy the tooth bud. Irradiation after calcification has begun may inhibit cellular differentiation, causing malformations and arresting general growth.
Children undergoing radiation therapy to the jawsmay show deficiencies in the permanent dentition such as retarded root development, dwarfed teeth, or failure to form one or more teeth (Fig. 3). Teeth irradiated during development may complete calcification and erupt prematurely. In general, the severity of thedamage is dose-dependent.
Irradiation of teethmay retard or abort root formation, but the eruptive mechanism of teeth is relatively radiation- resistant. Irradiated teeth with altered root formation still erupt.
Adult teeth are very resistant to the direct effects of radiation exposure.
Pulpal tissue, which consists primarily of reverting and fixed post mitotic cells, demonstrates long-term fibroatrophy after irradiation. Radiation has no discernible effect on the crystalline structure of enamel, dentin, orcementum, and radiation does not increase their solubility.
The increased rate of caries may be due to the indirect effect of radiation produced by reduced salivary flow rate and its associated consequences (Fig. 4).
The pain in temporomandibular joint (TMJ) may be due to edema, cell destruction, and fibrosis resulting from radiation. Limited mouth opening complicates oral hygiene procedures and provision of dental care [19].
Anxiety or lack of physical and emotionalmotivation, as well as decreased salivary flow, trismus, and other important factors make oral hygiene more difficult and accelerate loss of attachment.
The occurrence of microorganisms associated with these dental diseases increases the possibility of compromised bones being infected. Plaque control in irradiated patients is necessary to prevent colonization of microorganisms in the gingival crevice. Altered nature of microorganisms and reduced host defense mechanism toward plaque caused by radiotherapy may lead to attachment loss.
CONCLUSION
For a patient about to undergo tumoricidal radiotherapy for malignancy in the maxillofacial region, diseases of teeth and supporting structures are a worrisome finding because oral pain and infections are common and possibly severe sequelae to radiotherapy for head and neck tumors in patients with healthy mouth. Oral hygiene maintenance measures can give better outcome in maintenance of periodontal health during and after radiotherapy. Furthermore, dental treatment should be aimed at improving the oral hygiene status of patients through professional dental care. Patients should be constantly motivated toward maintaining a meticulous oral hygiene status before, during and after radiotherapy to prevent and control the oral and periodontal sequelae. The periodontist is an important member in the oncological team as increased oral hygiene maintenance can lead to reduction in post-radiation complications of peridontium.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


