All published articles of this journal are available on ScienceDirect.
Unconventional Implant Placement IV. Implant Placement through Impacted Teeth to Avoid Invasive Surgery. Long-term Results of 3 Cases
Abstract
This paper presents the long-term data of patients that have been treated with an unconventional implant placement protocol to avoid an invasive surgery when edentulism was caused by an impacted tooth. In 2009, the follow-up of this unconven-tional protocol was 2 to 3.5 years; this article documents now the long-term 5- to 8-year follow-up of 3 patients and 5 im-plants. Over this period of time, implant stability was maintained without complications. This unconventional protocol opens intriguing possibilities; however, more patients with long-term follow-up are warranted before endorsing it in routine appli-cation. Nonetheless, it might suggest that there is still room to revisit one of the leading concepts in dental implantology.
INTRODUCTION
Consider that at the inception of osseointegration, only 2-stage surgeries with titanium ancillary were recommended; post-operative radiographs were commended to be performed only at the end of a 3 to 6-month healing period; occlusal surfaces other than resin like metal or ceramics were barred from use [1]. One can then come to the conclusion that clinical protocols have dramatically changed over time; that paradigms-shifts have been common over the last 35 years. Still, osseointegration is widely ipso facto accepted as ‘implant surface should come into contact only with bone’, at the exclusion of any remnant tooth material [2].
In 2009, the first 2 clinical papers dealing with implants deliberately placed in contact with dental tissues were published. The related procedures were aiming at dodging invasive surgeries while treating ankylosed [3] or impacted teeth [4]. The follow-up of these prosthetically driven implants placed through dental tissues was ranging 12 to 49 months and 2 to 3.5 years, respectively.
Since then, more cases with impacted teeth have been successfully treated [5, 6] and the principle governing these protocols has been extended to inserting implants through residual roots [7, 8] or in contact with radicular dentine while seeking to optimize esthetics [9, 10]. The biological rationale of bringing implants into contact with dental tissues has been extensively addressed elsewhere [3-6]; it was found to get a trustworthy support from available histological data.
It is pointless to say that these innovative protocols need long-term documentation with large numbers of patients before being accepted in routine use by the clinical community. A large number of cases are not at hand because the present indication involves at best a few patients per year in the hands of every practitioner; getting sizable numbers requires time. Before getting the compulsory numbers, the way to start paving a conceivable route for such an unconventional protocol is to provide long-term documentation even on a small numbers of cases; this would help starting evaluating its long-term fate.
The first few cases with impacted teeth that have been treated with this unconventional implant protocol have been reaching now a follow-up of 5 and more years. The aim of the present paper is, therefore, to report on these first long-term data.
MATERIAL & METHODS
Inclusion Criteria and General Requirements
Conduct of the treatment adhered to the tenets of the latest available Declaration of Helsinki released by the World Medical Association. In addition, to undergo this unconventional treatment, the following conditions had to be met:
1) Patients had to be healthy and able to maintain good hygiene.
2) Implant therapy was indicated.
3) The impacted teeth had to be asymptomatic and free of surrounding pathology.
4) When treatment planning was discussed with the patient, it was explained that extraction might be complex and invasive; it would require additional augmentation procedures before implant placement. Also, the cortical table might collapse and require an additional bone augmentation procedure before or during implant placement.
5) The patient had to require an alternative option, less invasive and fostering the delivery of the implant-supported prosthesis;
6) A benefit/risk analysis was presented to the patient. Advantage of the protocole was that the patient could avoid an invasive surgery including a bone grafting procedure with a xenogenic material. He/she would be treated according to a standard implant placement procedure without delay after a standard integration period. Another advantage was that the risk of cortical table collapse was circumvented.
The risk of the present protocol was post-operative pain or implant failure after having encroached the impacted tooth. Would it happen, the implant would be immediately removed and the standard extraction procedure of the impacted tooth would follow. The site would then involve bone grafting and healing before placing an implant. Any complication would delay implant placement.
After explanation of the protocol and its deviation from standard care, the patient had to accept the risk of implant failure. In case of implant failure, the conventional treatment with an augmentation procedure was warranted at no additional cost.
7) An informed consent had to be signed.
All patients received standard antibiotic prophylaxis (Augmentin, 2 x 1g/d for 6 days, GlaxoSmithKline, Marly-le-Roi, France).
Evaluation of the Implants
Implants were evaluated clinically and radiography at the end of the healing period, at 6 months, and then annually. The success criteria according to Cochran et al. [11] were used. Clinical criteria included: 1) absence of clinically detectable mobility, 2) absence of pain or any subjective sensation, 3) absence of peri-implant infection. Radiographic success included: 1) absence of continuous radioluscency around the implant, 2) observation of any abnormal reaction at the bone-implant interface, 3) observation of any specific reaction at the root-implant interface, 4) determination of resorption of the remaining root fragment.
Case Presentation and Surgical Procedures of Implant Placement
Patient # 1
A 31-year old female patient attended to rehabilitate her maxillary right canine site. Her temporary canine was lost recently; the site was edentulous because the deciduous canine was impacted. She was wearing a provisional appliance and wished a fixed solution. Radiographic examination showed that the impacted canine was close to the alveolar ridge (Fig. 1a). For esthetic reasons, the patient vigorously refused to consider the orthodontic path prescribed by previous practitioners. The classical surgical approach was then explained; it consisted in removing the impacted canine, grafting the area and placing an implant after 6 months of healing and again waiting for the same amount of time. She was desperate for a shorter and less invasive solution.

Patient # 1. a) Panoramic radiograph with the unerupted canine. b) Radiograph showing the drilling through the impacted canine. c) Radiograph after removing the drill. Reduction in radio-opacity is related to the removal of dental tissue. d) Implant placement after removing the mobile fragment of the crown on the mesial side. e) Periapical radiograph at the 8-year control. f) Vestibular clinical view at the 8-year control. The papilla length is similar to the adjacent natural teeth.
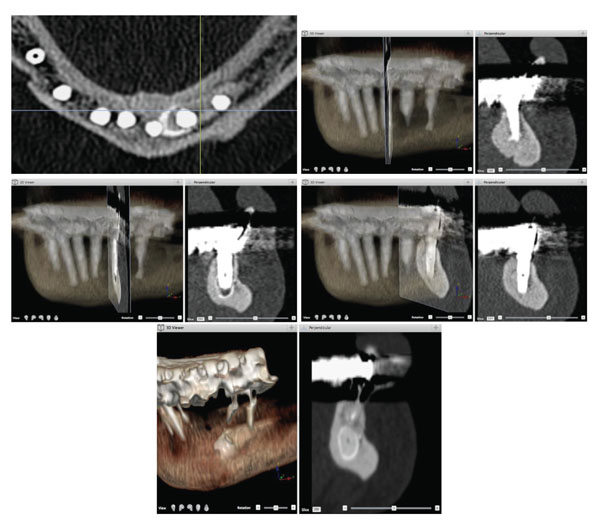
Patient # 2. a) Preoperative tomodensitometric examination displaying a 3D reconstruction and a transverse section at the impacted ectopic horizontal premolar. The impacted tooth is in the middle of the mandible just beneath the root of the failing teeth. b) Localisation of implant WHO # 32 (ADA # 23) and corresponding transverse section of the tomodensitometric examination at the 8-year control. c) Localisation of implant WHO # 33 (ADA # 22) and corresponding transverse section at the 8-year control. d) Localisation of implant WHO # 34 (ADA # 21) and corresponding transverse section at the 8-year control. e) Axial section of the tomodensitometric examination at the 8-year follow-up. Note the distinct position of each implant in contact with the various parts of the impacted premolar, the cuspid of the crown, the crown and the root. No specific deleterious radiographic feature could be observed.
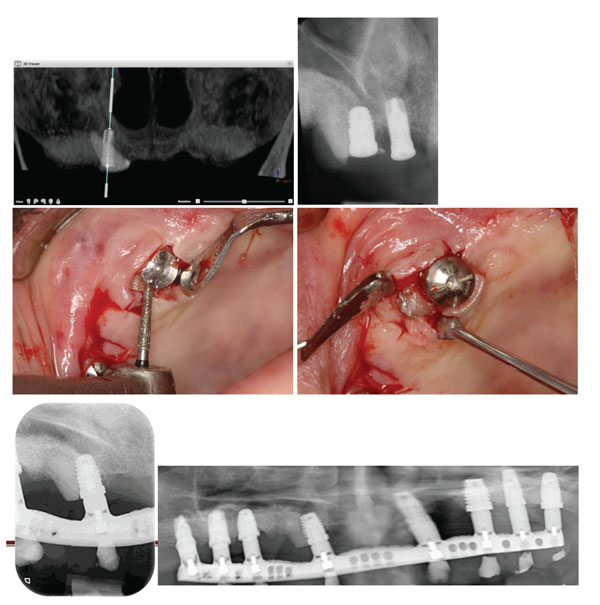
Patient # 3. a) Pre-operative panoramic radiograph with the radicular part of the canine. b) Post-operative radiograph of the implant encroaching the root. c) Flattening the distal part of the root of the impacted canine to accommodate the abutment. d) Flattened distal part of the root before suturing over the abutment. e) Periapical radiograph of the implant incroaching upon the canine at the 5-year control. f) Panoramic radiograph of the implant-supported prosthesis at the 5-year control.
To meet the needs of the patient, an alternative non-invasive protocol was then proposed; it was relying on a previous case that has been successful during 6 months until the canines were removed [4, 5]. It was stressed that would this treatment fail, she would go for the conventional way at no additional cost. The patient accepted to cope with the risk.
A large diameter tapered implant was planned (NT Osseotite, Ø 5 x 15 mm, 3i, Palm Beach Gardens, FL, USA). The impacted site was drilled following the manufacturer recommended drilling sequence, i.e. with the Ø 3.25 drill (Fig. 1b, c), the Ø 4 mm and Ø 5 mm. The Ø 6 mm drill was also used over the coronal half of the osteotomy; the aim was to hope keeping away the dental implant from direct contact with the root of the impacted canine. The coronal portion of the crown was totally removed and the implant was placed (Fig. 1d). Primary stability was achieved at implant seating but the palatal side was left with a bone defect; it was then filled with Bio-Oss® (Geistlich AG, Switzerland), a bone substitute of bovine origin. The gingiva was sutured over the implant.
Patient # 2
A 80-year old men attended with a failing mandibular tooth-supported prosthesis. The panoramic radiograph showed that all teeth needed extraction; in addition an impacted premolar was found (Fig. 2a). The impacted premolar was horizontal and the level of impaction was classified as level C [12], i.e. the crown of the impacted tooth was beneath the root apices of the adjacent teeth. Impaction was not associated with a pathological image on the CT scan sections. The patient was seeking a global prosthetic solution in the mandible.
Implant simulation showed that there was no way for the implants to avoid encroaching upon the impacted premolar. It was explained to the patient that the conventional treatment would require extraction of all the remaining teeth, removing invasively the globulous impacted premolar and grafting the created major bone defect. Implants would be placed after a healing period of 6 months. In addition, wearing a temporary prosthesis was strongly dissented for at least 8 weeks in order to protect the grafted sites. The patient asked for a shorter and less invasive alternative.
A non-invasive 2-step solution was therefore discussed. It was proposed to extract all teeth but the canines and place 5 implants; 2 of them would be encroaching upon the impacted premolar in sites WHO # 32 (ADA # 23) and # 34 (ADA # 21). During the 3 months required to achieve implant stability, the canines would support a provisional bridge. At the 2nd-stage surgery, the canines would be extracted and 2 more implants would be placed in the extraction sites. The provisional bridge would be then further prepared to rely on the 5 integrated implants and the 2 newly placed ones.
Eventually, 3 out of the 7 implants did encroach upon the impacted premolar; all achieved primary stability. Implant at site WHO # 34 (ADA # 21), crossed the premolar root (Fig. 2b), its apical extremity was in contact with bone. At site WHO # 33 (ADA # 22), the implant apex was kept within the impacted crown without contacting bone (Fig. 2c). Implant at site WHO # 32 (ADA # 23) had its distal side in contact with the cuspidal edge of the crown (Fig. 2d). Implants were Osseotite Certain Ø 4/5 x 13 mm, full Osseotite NT Ø 5 x 11.5 mm and Ø 4 x 13 mm, respectively.
Patient # 3
A 85-year old women attended to rehabilitate her atrophic edentulous maxilla. The root of an ankylosed impacted canine was found outcropping the crest on the right side. Bone grafting has been previously performed to receive implants (Fig. 3a). The angulated root canine was occupying a position of strategic importance for implant placement. It was decided to maintain it in order to host an encroaching implant with sufficient primary stability. Implant simulation showed that at least 50 % of the implant surface would be in contact with bone. Nine implants were placed in position WHO # 11, 12, 13, 14, 16, 17, 21, 25, 26 (ADA # 2, 3, 5, 6, 7, 8, 9, 13, 14) and left to heal in a submerged way for 6 months (Fig. 3b).
RESULTS
Patient # 1
No post-operative pain was reported by the patient. The 6-month submerged healing period was uneventful. After checking for implant stability the prosthetic steps were carried out and a single ceramo-metallic crown was delivered. The patient was happy that the edentulous site could be treated in a single non-invasive session, in contrast to the treatment offered by various other practitioners.
At the 8-year control, the implant was clinically stable devoid of any subjective symptoms. Bone has filled the original post-operative defect; platform-shifting has been successful in retaining the crestal bone at its pristine level (Fig. 1e). Radiographically, no abnormal reaction could be observed either at the bone-implant or at the root-implant interface. The remaining root fragment was present.
The pink and white score [13] was 14;. it was reflecting the gingival and bone response to the procedure (Fig. 1f).
Patient # 2
Both implant healing procedures were uneventful, no post-operative pain was reported by the patient. The provisional prosthesis was replaced by a final ceramo-metallic bridge.
At the 8-year control, the bridge was clinically stable and implants were successfully fulfilling their function. Attempt to perform a periapical radiograph was unsuccessful because of a pronounced vomiting reflex. Tomodensitometry radiographic examination displayed artefacts at the immediate implants surroundings; however, no specific deleterious feature could be observed (Fig. 2b-e). The crestal bone levels were maintained high, about to reach the level of the neck.
Patient # 3
No post-operative pain was reported by the patient. The 6-month healing period was uneventful but perforation of the mucosa by the underneath radicular portion of the canine was recorded at the 2nd stage surgery. The coronal part was flattened with a bur to accommodate the abutment (Fig. 3c, d) and the mesial portion of the root was removed. After another month, the prosthetic steps were undertaken and the final prosthesis was delivered.
At the 5-year control, the prosthesis was stable; the implant placed through the canine did not show any worrying radiographic feature related to the dentine-implant interface (Fig. 3e, f). On the distal side, the dental tissue of the canine retained the level of the most coronal part of the alveolar crest close to its pristine situation (Fig. 3e,f). On the mesial side, bone was close to the level of the neck (Fig. 3e).
DISCUSSION
This is the first paper reporting on long-term data of implants deliberately placed in contact with dental tissues other than bone with the aim of avoiding an invasive surgery. The reason that led to the developpement of this protocol have been previously explained [3-6]
In all 3 patients, healing was uneventful and post-operative pain was not reported. Implants have been clinically stable and successfully functioning for 5 to 8 years. Five out of six implants have been placed in elderly patients. It is highly probable that the pulp of their impacted teeth was calcified; this might then explain the absence of post-operative pain. However, the same lack of pain at the 31-year old patient of this series of cases and other younger patients reported elsewhere [5, 6] suggest that absence of pain is the rule rather than the exception. The same absence of pain has been reported when coronoectomy of wisdom teeth close to the alveolar nerve was applied in order to avoid injuring it or to move the impacted tooth away from the nerve [14, 15].
This unconventional protocol allowed implementation of implant placement following a conventional surgical procedure. Dodging it would had led the patients to a surgical track of more than one surgery until reaching the standard conditions of implant placement. The treatment would had been then delayed by at least 6 months, probably more.
Several authors reported that orthodontic canine alignment is not as predictable in adults as in teenagers [16-18]. Becker & Chaushu [19] even stressed that this handling failed in all patients over 30 years. Therefore, in case this unconventional procedure gains recognition by the dental community, it might turn into one of the accepted care options on top of the invasive surgical procedure of tooth removal and further implant placement [20-22].
New interfaces have been created with the implants encroaching upon an impacted tooth; they are the following; 1) an implant-periodontal ligament interface, 2) an implant-cement interface, 3) an implant-dentine interface, 4) an implant-pulp interface, 5) an implant-enamel interface.
Some histological data exist to address all these new generated interfaces [2, 9, 23-27] except for the implant enamel interface. Two implants out of the 3 placed in patient # 2 were encroaching the crown; one of them was only in contact with the cuspid of the crown (Fig. 2e). This means that the enamel-implant interface did not jeopardize implant prognosis. Although these long-term data involve only a limited number of patients and implants, they might serve as a starting substrate to envision positively any new protocol that would require placing implants in contact with dental tissues.
At the beginning, a clinical relevance has been related to 3 distinct indications. Their common goal was to avoid invasive surgeries; they were: placing implants through impacted teeth [4, 7], ankylosed teeth [3, 7] and residual roots [7, 8]. But other authors found it applicable to address esthetic issues in order to maintain an optimal support to the marginal gingiva [9] or the papilla [10].
Noteworthy, the present data do not suggest that it should be feasible without consequences to encroach upon a neighbouring vital root in order to place an implant in a narrow space. Because this might lead to either root-canal treatment of the injured dental entity or implant failure [28-31].
Epidemiologic studies have reported that the frequency of impaction of the maxillary canine is low, in the 1-3 % range [32]; indeed, such cases occur once or twice a year in most dental settings. But, then this makes large numbers of patients, in the range of several tens of thousands over the world, and it is worth to work on offering them a possibly relevant patient-friendly surgical protocol.
CONCLUSION
Placing implants through impacted teeth and generating interfaces other than the implant-bone interface led to uneventful healing; it did not interfere the clinical stability of these implants in the long-term, up to 8 years. More implants are warranted before this protocol can be advocated for routine use but it might open intruiging treatment perspectives. Moreover, it might suggest that there is still room to reevaluate well-anchored paradigms in dental implantology as published elsewhere [5, 6].
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors are thankful to the efficient help and skills of Aurélie, Vanessa, Alexandra, Vida and Sabrina.


