All published articles of this journal are available on ScienceDirect.
The Evolution of Dental Materials for Hybrid Prosthesis
Abstract
Since the immemorial, the replacement of missing teeth has been a medical and cosmetic necessity for human kind. Nowadays, middle-aged population groups have experienced improved oral health, as compared to previous generations, and the percentage of edentulous adults can be expected to further decline. However, with the continued increase in the number of older adult population, it is anticipated that the need for some form of full-mouth restoration might increase from 53.8 million in 1991 to 61 million in 2020 [1]. Denture prosthetics has undergone many development stages since the first dentures were fabricated. The introduction of computer-aided design/computer aided manufacturing (CAD/CAM) has resulted in a more accurate manufacturing of prosthetic frameworks, greater accuracy of dental restorations, and in particular, implant supported prosthesis.
HISTORIC PERSPECTIVES
Since the immemorial, the replacement of missing teeth has been a medical and cosmetic necessity for human kind. Denture prosthetics has undergone many development stages since the first still preserved dentures were fabricated. While 3,500 years ago, the ancient Egyptians carved false teeth out of mulberry wood and tied them to the adjacent teeth with gold wire, the Etruscans arrived at considerable skill, producing construction made of gold and bovine teeth, which were already guided by principles used in denture prosthetics today [2].
Dental technology remained virtually undeveloped until the 18th century. Candidate materials for artificial teeth during the 18th century were (1) human teeth, (2) animal teeth carved to the size and shape of human teeth, (3) ivory, and finally (4) “mineral” or porcelain teeth. Other than for costly human teeth that were scarce, the selection of artificial tooth materials was based on their mechanical versatility and biologic stability. Animal teeth were unstable toward the “corrosive agents” in saliva, and elephant ivory and bone contained pores that easily stained. Hippopotamus ivory appears to have been more desirable than other esthetic dental substitutes [3, 4], John Greenwood carved teeth from hippopotamus ivory for at least one of the four sets of complete dentures he fabricated for George Washington [5]. Lower dentures, made of ivory with inset of cadaver teeth, worked reasonable well and managed to stay in place without too much difficulty, especially if weighted with some lead. The difficulties really came to the fore with the upper denture, which refused to stay in place due to both the heavy weight and the poor fit. In order to overcome this problem, upper dentures were fashioned onto the lower dentures by means of springs or hinges. This technique would ensure that the upper denture would always be pushed up against the roof of the mouth [6].
The first porcelain teeth were developed as early as in 1709 after the introduction of porcelain manufacturing secrets by Father d’Entrecolle, a Jesuit priest who had spent many years in China, but their massive production was not undertaken until 1837 [2]. This end the practice of transplanting freshly extracted human teeth and supplanted the use of animal products [5].
In 1774, Alexis Duchateau and Nicholas Dubois de Chemant, made the first successful porcelain dentures at the Guerhard porcelain factory [5, 7].
A new era was marked for dental prosthetics after Charles Goodyear in 1850 invented the vulcanization process. In this process, rubber was hardened in the presence of sulphur to produce a material call vulcanite, this material was not only cheap but was also easy to work with; it could be molded to provide an accurate fit of the denture base to the model and hence to the oral structures. The first sets of dentures based on rubber and porcelain began to appear in 1881 when the patent expired in and less expensive dentures could be made available to the masses of people in need of them [6].
In 1930’s Dr. Walter Bauer introduced polymethyl methacrylate (PMMA), an amorphous polymer, highly transparent and rather brittle, yet highly stable towards aqueous media and UV radiation, tasteless, easy to repair and high shape stability [8], a suitable candidate for vulcanite substitute.
HISTORY OF IMPLANTS
The history of dental implants is as fascinating as it is ancient [9-12]. There do not appear to have been any geographical restraints to the desire of early dental practitioners to provide replacements for missing or diseased teeth. Dental implants and transplant history can be traced to Africa (Egyptians), to the Americas (Mayans, Aztecs and Incas), and to the Middle East. Also in this earliest historical period, tooth transplants can be traced to the Greeks, the Etruscan, and the Romans [13]. The first endosseous implant that present oseointegration is probably from the Mayans (7th century AD) where sea shells were carved as tooth shape and placed in the mandible [14].
Today dental implants have become one of the most exciting and rapidly developing aspects of dental practice. The rapid increase in the acceptability of dental implants as regular treatment in the late 20th and early 21st centuries is largely attributable to Swedish Professor Per-Ingvar Brånemark during the 1950’s, an orthopedic surgeon who turned an accidental discovery into a dental revolution [15] a new form of attachment mechanism; the osseointegration. Osseointegration is a biological concept and refers to the incorporation within living bone of an inanimate (metal) component. Most implants are made out of titanium and placed into the bone of the jaws by surgical means, and protrude through the mucosal tissues to provide attachment anchorage of replacement artificial teeth [16].
HYBRID PROSTHESIS
The fixed-removable prosthesis resembles a flangeless denture that is retained solely by several osseointegrated implants. There is no contact between the prosthesis and the tissues of the alveolar ridge.
The original design of the fixed-removable prosthesis was developed by Swedish investigators using the two-stage endosseous implant system developed by Brånemark. The prosthesis consisted of a gold alloy framework attached to the copings of the implant. Acrylic resin denture teeth were arranged on the framework and secured with acrylic resin [17]. The fixed-removable prosthesis represented a unique aspect of prosthodontics reconstruction for edentulous arches, since implants were situated in the anterior region and the posterior sections of the framework were cantilevered from the anterior portion of the framework (Fig. 1). The length, height, and width of the cantilever are crucial in minimizing the amount of deformation of the prosthesis (Fig. 2). According to Glantz, the mount of deformation of the cantilever is directly proportional to the cube of the length and inversely proportional of the width and the cube of the height of the cantilever [18]. In addition, there is a direct relation between the amount of deformation and the force of the occlusion (loading force) as well as an inverse relation with the modulus of elasticity of the material to be used for the framework. This relationship can be expressed in the following equation:

Conventional design for hybrid prosthesis with long distal cantilevers.

Catastrophic fracture of distal extension due to extensive cantilever.

Excellent maintenance and oral hygiene after 3 years from maxillary hybrid prosthesis delivery.

Intaglio surface of maxillary hybrid has been custom designed in order to improve esthetics and phonetics.

Ideal implant distribution.

Prosthetic system out of distal cantilevers.

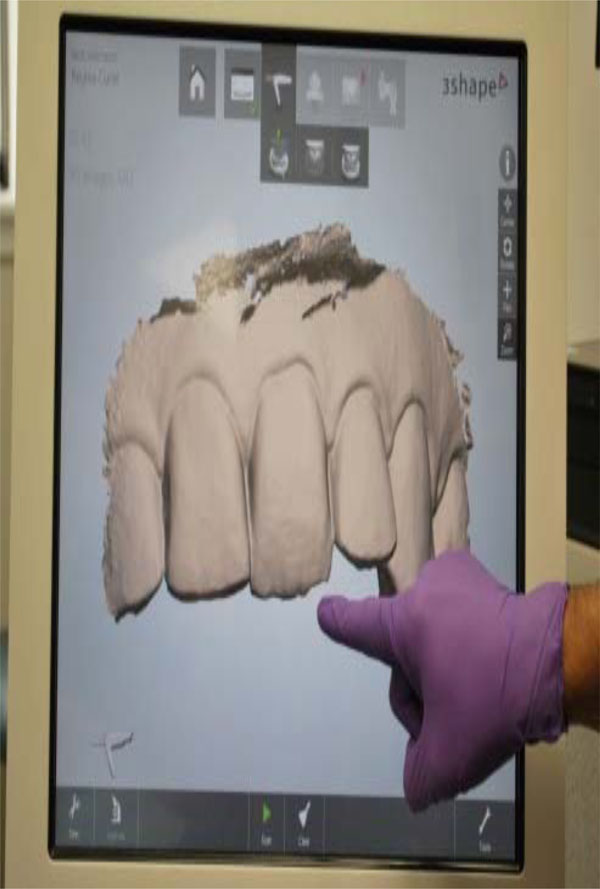
Intraoral scanner apparatus.

Intraoral digital impression.
Design data in the CAD program.

Milling device.

Zirconia framework for hybrid prosthesis.

Hybrid prosthesis with zirconia framework and porcelain veneering material.

Monolithic zirconia framework is custom contoured for a partially sintered system.

Monolithic zirconia framework is custom colored for a partially sintered system.

Special felthpatic porcelain can be added in order to enhance esthetics in specific areas, optional procedure.
D = F x L x constant / E x W x H
Where D is the amount of deformation, F is the force of occlusion, L, W, and H are the length, width, and height of the cantilever, respectively, and E is the modulus of elasticity of the material. Therefore, the length of the cantilever should be minimized while maximizing the height and width of the cantilever. It has been recommended that the cantilever should not exceed 20 mm in length using five or more abutments. If four abutments are used the cantilever should not exceed 15 mm in length [19]. Other studies have shown that the length of the extension should be shorter in the maxillary arch as opposed to the mandibular arch because there is less cortical bone present in the maxilla [20]. The junction of the cantilever and the distal abutments should be provided with added height and width as this area is the primary stress point in relation to the cantilever. There should be about 1 to 2 mm of space between the inferior border of the cantilever and the alveolar ridge to allow for adequate oral hygiene. It is recommended that the metal alloy possess sufficient yield strength (>300 MPa) and modulus of elasticity (>80,000 MPa) to prevent deformation and fracturing of the cantilevers. The literature reports casting the framework in type IV gold or precious metal alloys such as silver-palladium alloy [21]. The use of posterior prosthetic teeth with minimal inclinations is recommended to minimize and lateral forces on the cantilevers during excursive movements. Acrylic resin prosthetic teeth should be used to absorb the shock of occlusal forces [16].
Brånemark has stated that “critical to the maintenance of osseointegration the carefully controlled and prosthetic-induced loading of the implant-tissue interface”. He stressed that a controlled mechanical environment is necessary to assure adequate remodeling stimulus for maintenance of integration [22, 23]. Osseointegrated implants supporting fixed prostheses are exposed to both dynamic and static loading. Dynamic forces on the implants may arise due to chewing and can reach various magnitudes [24]. Static loading on the other hand may be induced by the tension in the bridge locking screws, when securing a misfitting framework to the implants [25]. To help clinicians understand the importance of controlled loading, he stated the precision of the prosthesis fit should be at the 10 µm level.
According to Zarb and Jansson, frameworks in fixed prostheses could be designed in one of the two ways: (1) where metal frameworks comprised the bulk of the prostheses, and artificial teeth and minimal denture bases were the only non-metallic components. (2) Implant fixed prostheses consisting mostly of acrylic resin denture bases (wraparound design) and artificial teeth, with minimally sized metal frameworks [17].
Esthetic demands tend to be more dramatic with maxillary prostheses than mandibular prostheses (Fig. 3). As per Zarb and Schmitt, unlike mandibular implant prostheses were hygienic type designs have proven to be functionally and esthetically acceptable, maxillary implant prostheses demand different sized and shaped labial/buccal flanges that may or may not compensate for optimal esthetics, phonetics, and masticatory function (Fig. 4). Additionally prosthetic gingival tissues are often required due to resorptive patterns of edentulous maxillae. Resorptive patterns in maxillae are dissimilar to mandibular resorption pattern: maxillae resorb superiorly, posteriorly, and medially: mandible resorbs inferiorly, anteriorly, and laterally [26, 27].
ALL ON 4
Implant treatment was based on basic prosthodontics principles that included preliminary and definitive impressions, jaw relation records, wax try-in, metal framework try-in, and insertion of definitive prostheses. Frameworks were fabricated according to the following criteria: bulk for strength, adequate access for oral hygiene procedures, minimal display of metal on the facial and occlusal surfaces, and strategic thinning of implant frameworks to allow for retention of acrylic resin denture teeth and denture basses [28].
Traditionally, and according to the original concept of the Brånemark system, implants are placed in a fairly upright position in the anterior edentulous mandible. Therefore, it is often necessary to fabricate a bilateral cantilever, which is sometimes up to 20 mm long, to provide the patient with good chewing capacity in the molar region. Clinical studies have demonstrated that the distal tilting of implants may be advantageous, with reduction of cantilever length about 6.5 mm in the mandible and 9.3 mm in the maxilla [29, 30].
The introduction of osseointegration to North America in the early 1980’s has created new challenges and opportunities for dental technicians. Totally new concepts of prosthesis design continue to evolve. Structural engineering principles are combined with artistic skills to build an accurately fitting, durable and esthetic prosthesis [31].
Introduced by Malo´ et al. in 2003, the All on 4 concept involves the use of 4 implants, including 2 distally tilted ones in areas where bone height; nerve proximity; or the proximity of the sinus, inferior alveolar canal, and/or mental foramen have precluded the placement of axially oriented implants. In addition to preserving the relevant anatomic structures, the distal tilting allows for placement of longer implants with good cortical anchorage in optimal positions for prosthetic support. It also increases the inter-implant spaces, reduces cantilever length, and reduces the need for bone augmentation (Figs. 5and 6). Published studies on the All on 4 concept have shown cumulative survival rates to range between 92.2% and 100% [32].
DIGITAL IMPRESSIONS
A well-accepted principle of restorative dentistry is that the final restoration can be only as accurate and well adapted as the final impression. The clinical challenge is to provide an accurate final impression of the intraoral condition to the laboratory if the impression materials are prone to dimensional changes due to on-going chemical reactions [33] and stone will show expansion due to secondary reactions whilst setting [34]. The misfit of fixed partial dentures on natural teeth will result in forces on the underlying teeth. Natural teeth however can move 25-100 µm in axial direction and 56-108 µm in lateral direction [35, 36] and adapt to a slightly different position in the bone due to the periodontal ligament should there be a slight misfit of the prosthetic work. Implants on the other hand will only show a range of motion of 3-5 µm in axial direction and 10-50 µm in lateral direction after osseointegration due to compression of the bone [36]. Ill-fitting frameworks will generate stress on the implants which may have a biological effect on the bone-implant interface [37, 38]. It has been also shown that stresses introduced by misfit were comparable with that related to occlusal forces [39]. Prosthetic complications as screw loosening or fracture may be also related to ill-fitting framework fit [40]. The aforementioned factors have resulted in the paradigm that passive fit of the framework is one of the key factors for long-term success in implant dentistry [41, 42] stressing the importance of a reliable and precise impression procedure. Several strategies have been developed to ascertain passive fit [35, 43]. An intraoral scanner could overcome some of the errors associated with traditional impression taking [44] and cast production [45], since digital output data can be fed directly into a digital workflow.
In general, all of the current systems follow the basic workflow of computer-assisted design/computer-assisted machining (CAD/CAM) to create a restoration. There are three main sequences to this workflow. The first sequence is to capture or record the intraoral condition to the computer (Fig. 7). This involves the use of a scanner or intraoral camera (Fig. 8). Once the data has been recorded to the computer, a software program (CAD) is used to complete the custom design of the desired restoration (Fig. 9). This may involve a full-contour design of the restoration or just the internal coping or substructure of the final restoration. The final sequence requires a milling device to fabricate the actual restoration from the design data in the CAD program (Fig. 10) [46].
ZIRCONIA
The introduction of computer-aided design/computer-aided manufacturing (CAD/CAM) has facilitated the use of new dental ceramic materials. Zirconium oxide, known as zirconia is currently used as a core material for fabrication of frameworks for tooth and implant-supported fixed partial dentures (Fig. 11). Esthetics is optimized with zirconia restorations due to the natural shade of the substrate, thus eliminating the problem of the gray effect, especially at the cervical area, of implant prostheses with metal alloy substructures (Fig. 12) [47]. Zirconia stabilized with yttrium oxide possesses good chemical and physical properties such as low corrosion potential, low thermal conductivity, high flexural strength (900-1200 MPa), and hardness (1200 Vickers) [48, 49]. In addition, zirconia is considered more biocompatible than other ceramics, titanium, and metal alloys, which may facilitate soft tissue response in terms of heath [50].
However, several authors [51-53] have expressed concern about the long term degradation, or aging, associated with the spontaneous transformation of the metastable tetragonal phase to the monoclinic phase. It has been shown that the spontaneous tetragonal to monoclinic transformation can drastically decrease the mechanical properties of the zirconia by surface roughening, grain pull out, and micro-cracking [54]. In vivo, these micro-cracks offer a pathway for water to diffuse further into the bulk of the ceramic. This transformation occurs when the tetragonal phase is exposed to elevated temperatures, those approaching 250°C and/or aqueous environments. It is not well understood how the combination of stresses, temperature, acids, humidity, and saliva in the oral environment affects the rate of this transformation [52]. Several studies have shown that the strength of zirconia test specimens has not been significantly affected by aging according to the ISO standard 13356 (steam autoclave: 5 hours at 0.2 MPa and 134 °C) [55]. Molin et al. followed zirconia restorations for at least 5 years concluding that the fracture of zirconia is rare [56-58].
COPY-MILLED ZIRCONIA SYSTEMS
There is a growing array of digital technology and computerized systems for restorative dental treatment. Most zirconia-based restorative systems use computer-aided design/
computer-aided manufacturing (CAD/CAM) technology for the design and subtractive rapid prototyping technology for the fabrication of the zirconia frameworks. Once the design of the framework is completed, the data is transferred to a milling unit for fabricating the framework. The frameworks can be fabricated from fully sintered zirconium oxide or partially sintered zirconium-oxide blanks. The proponents of partially sintered frameworks claim that micro cracks may be introduced to the framework during the milling procedure of a fully sintered blank, whereas the proponents of milling of a fully sintered blank claim that because no shrinkage is involved in the process the marginal fit is superior [59, 60]. Probably the partially sintered zirconium technique presents several appealing advantages; the fully customization of framework into monolithic shape (Fig. 13) and intrinsic colorization (Fig. 14). Such ability to control the framework contours and colors provides the ceramist and the clinician additional flexibility, while providing the patient with robust and esthetic restorations (Fig. 15).
CONCLUSION
This article presented a review of current and past literature regarding the evolution of different materials used for construction of hybrid prostheses. Several advantages can be drawn including CAD/CAM technology, 3D scanning, and monolithic zirconia as framework substrate material. Complications associated with the relative inaccuracy of casting have been significantly improved with the introduction of CAD/CAM technology in implant dentistry. Errors associated with traditional impressions can be solved utilizing 3D scanning since digital output data is fed directly into a digital workflow. Partially sintered monolithic zirconia as an implant-supported prosthetic material, reduces chipping of the veneering porcelain and may requires less prosthetic space compared to a conventional hybrid prosthesis due to its monolithic nature. Improved aesthetics can be achieved due to intrinsic staining capabilities. Such advantages are revolutionizing industries by enabling the merger of mass production and individual customization into fast, cost-efficient workflows that assist in the increasing demand for treatment of the edentulous patient.
CONFLICT OF INTEREST
The author confirms that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.


