All published articles of this journal are available on ScienceDirect.
Combined Soft and Hard Tissue Peri-Implant Plastic Surgery Techniques to Enhance Implant Rehabilitation: A Case Report
Abstract
This case report presents an implant-aided prosthetic treatment in which peri-implant plastic surgery techniques were applied in combination to satisfactorily attain functional aesthetic expectations. Peri-implant plastic surgery enables the successful reconstruction and restoration of the balance between soft and hard tissues and allows the option of implant-aided fixed prosthetic rehabilitation.
INTRODUCTION
Dental implants are preferred over removable prostheses because they are convenient, as these prostheses are fixed [1]. For successful implants, soft and hard tissues should have adequate volume and quality and present a balanced unit for implant placement [1-8]. Peri-implant plastic surgery techniques have facilitated the development of healthy peri-implant soft and hard tissue structures, thus providing more satisfactory functional and aesthetic implant results [2-4, 6, 7].
Peri-implant plastic surgery is the adaptation of plastic surgery to implantology [2-4, 6, 7]. These techniques were initially presented as “soft tissue management/augmentation” for the treatment of soft tissue defects [2-4, 6]. Peri-implant plastic surgery has evolved into an expanded role and now includes the treatment of hard tissue defects. Currently, peri-implant plastic surgery for hard tissue defects is considered a “bone enhancement/augmentation technique” [1-3].
Peri-implant soft tissue defects generally occur because of insufficient keratinized mucosa (KM) [3,4]. KM comprises dense, collagen-rich connective tissue, lined by a keratinizing epithelium. Peri-implant plastic surgery enables the creation of KM and the development of interimplant soft tissue height in order to avoid food impaction, interimplant airflow, and speech problems [3].
Peri-implant hard tissue defects occur due to traumatic tooth extraction, advanced periodontal disease, and abscess formation [5]. These defects complicate or prevent ideal placement of an implant and create aesthetic problems [1, 9, 10]. Application of bone augmentation in the defect area before implantation provides aesthetic and functional advantages and enables the optimal placement of implants [1, 9, 10]. Bone augmentation techniques are useful in extraction socket defect grafting, horizontal ridge augmentation, vertical ridge augmentation, and sinus augmentation [1, 9-13]. Furthermore, autogenous bone grafts have been shown to be the most successful grafts because of lower infection rates versus other graft materials and their osteogenic and osteoinductive effects [1, 9-13].
When hard and soft tissue defects exist together, it presents the ideal opportunity to use combined peri-implant plastic surgical approaches [2-4]. In this study, we describe the techniques and clinical results of hard and soft tissue peri-implant plastic surgical procedures used in the before and after the implant period for our patient’s oral rehabilitation.
CASE PRESENTATION
A 45-year-old woman presented to our clinic with missing left maxillary central and lateral teeth with an associated bone defect area. After initial examination, the left canine tooth along with an associated endodontic-periodontal lesion was extracted (Fig. 1). The patient underwent clinical and radiographic (periapical and panoramic radiography and dental computed tomography) measurements. Because the potential implant site had a shallow vestibule due to heavy inflammation and a horizontal bone defect, it was felt that the patient would benefit from peri-implant plastic surgery. Right maxillary central and lateral teeth were extracted because of insufficient periodontal support. Pre-implant and post-implant plastic surgeries were planned.

Patient prior to treatment.

FGG application of the anterior maxillary area, including the augmentation area.

Six months post-implant surgery and bone augmentation.

Implant surgery and the papilla regeneration technique (second surgery). A full-thickness flap was elevated, and simultaneously, an immediate implantation was performed in the right central tooth area. Semilunar bevel incisions were made, recreating a scalloped shape similar to that of tissues around natural teeth (The rotation of the pedicles made it possible to close the space between the abutments).
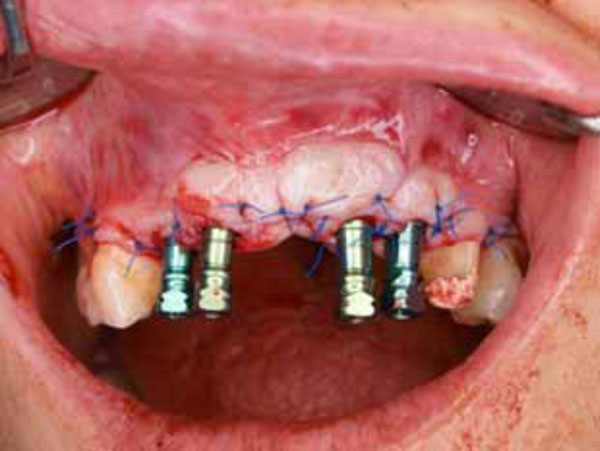
Suturing of the flap.

Provisional restorations with over contouring in the central tooth area.

Papilla formation in edentulous area.

Clinical appearance after prosthetic rehabilitation was completed.
KM Width Increase Via FGG
To increase pre-implant KM width (KMW), we used the free gingival graft (FGG) technique (Fig. 2). The FGG was also used to cover the block bone graft completely to enhance healing. The block bone augmentation recipient site was prepared by making a horizontal incision from the mucogingival junction. The FGG was obtained from the hard palate. After three weeks, FGG vestibular depth was adequate and KM had formed.
Monocortical Block Bone Augmentation
Block bone augmentation was performed under local anesthesia three months after the FGG application (Fig. 3). Initially, a sulcular incision was made at the defect site. The exposed resorption site was measured in millimeters, and the dimensions of the block bone graft were determined according to these measurements. A horizontal incision was made from distal to the mandibular third molar, which was chosen as the donor site, to the ramus. The graft dimensions were marked with round burs, and the block graft was obtained using an osteotome. Subsequently, the graft was fixed to the defect site with a titanium screw. The flap was sutured to the graft site without tension. Postoperatively, the patient was prescribed amoxicillin/clavulanic acid 875 mg/125 mg BID, an analgesic, and chlorhexidine mouthwash for 5 days.
Implant Surgeries
Implant therapy was performed in two stages. The first implant surgery was performed six months after the initial augmentation. The screw at the augmentation site was removed, and two dental implants (Tapered Screw-Vent, diameter: 4.1, and length: 10 mm; Zimmer Dental, Carlsbad, CA, USA), were placed at the site. The central tooth in the right maxillary area was extracted because of insufficient periodontal support and the possible risk of prosthetic failure, even in the short term. The area surrounding the implant was supported with a bone graft and a collagen membrane. A second implant surgery was performed four months after the first implant surgery, during which time the patient had used fixed provisional bridges.
Papilla Regeneration Technique
At the time of the second implant surgery, the provisional bridge was removed, and the initial implants were exposed. The maxillary right lateral tooth was extracted, and papilla
regeneration was performed. A full-thickness flap was elevated and reflected labially. The healing abutments held the flap in place. Semilunar bevel incisions were made, recreating a scalloped shape similar to that of tissues around natural teeth. The tissue was rotated towards the palate to create a papilla between the implant and the tooth. The flap pedicles filled the interimplant space. Sutures (5.0-trofilen monofilament; polyvinylidene fluoride) were used to secure the tissues. This technique was done not only around implants placed four months previously, but also immediately after for the additional implants placed that day (Fig. 4, 5).
Prosthetic Restorations
Temporary prosthetic restorations were performed 2 months after the papilla regeneration technique; subsequently, there was no observable pathological tissue reaction at the socket site. The alveolar ridge was nearly flat. For an aesthetic view, the provisional bridge was modified on the maxillary left central tooth area to form papilla on both sides of the tooth. The pontic area on the left central tooth was carved on the cast, and provisional restoration was formed with over contouring. To prevent infection, the pontic was polished carefully, and restoration was temporarily luted (Fig. 6). Follow-up visits were continued until we were satisfied with the appearance of the papilla and alveolar ridge at the end of the fourth month (Fig. 7). At that time, definitive bridges were fabricated using metal-ceramic restorations. At the 24-month follow-up, the patient had no functional, psychological, aesthetic, or phonetic problems (Fig. 8).
DISCUSSION
The functional and aesthetic success of dental implant procedures depends on the balance between soft and hard tissue structures [2-4]. Therefore, soft and hard tissues are best prepared for ideal implant positioning by the use of peri-implant plastic surgery techniques [2-4]. Because there is no consensus on the ideal peri-implant plastic surgery approach, the decision regarding which techniques to apply depends primarily on the clinician’s choice [4].
The patient presented in our report had a severe horizontal defect and a shallow vestibular depth resulting from previous infection at the anterior maxillary site. This made implant-aided fixed prosthetic treatment challenging. Implant surgery was performed in several stages, and aesthetic. expectations were managed using fixed temporary bridges.
Peri-implant plastic surgery was performed in two stages: pre-implantation and post-implantation. The aim of the pre-implant procedures was to create sufficient bone and KM in preparation for the implants. Initially, KMW increased via the FGG. A FGG was also used to cover the block bone graft completely and to enhance healing. Thus, the implant site was prepared for augmentation by application of the FGG graft. This method is an alternative to the “controlled tissue expansion” technique [14]. Increasing the KMW benefited peri-implant tissue health.
During the second stage of pre-implant plastic surgery, monocortical block bone augmentation was used to obtain bone of sufficient volume and quality. In defects in which horizontal ridge formation is too severe, implant placement may be impossible [1, 9, 10, 15]. Several methods have been used to maintain horizontal ridge augmentation [1, 9, 10, 15]. A bone block graft is the preferred method for many types of augmentation procedures because it secures a source of osteogenic cells and provides a rigid structure for mechanical support [1, 9, 15, 16].Recent studies have shown that block bone grafts from the mandibular ramus site lead to successful bone reconstruction in the maxillary alveolar ridge [1, 16]. However, the slow revascularization and remodeling processes of mandibular bone blocks requires waiting at least four months after graft healing before implant insertion [17, 18]. We detected no necrosis in our case after the augmentation, during the six month wait before performing the implant.
There is no consensus regarding the timing of peri-implant plastic surgery. Soft tissue enhancements have been performed before, during, or after implantation surgery for the prevention or treatment of peri-implantitis [2, 4, 6, 19, 20].In our case, soft tissue augmentation using the FGG was performed several months before the first implantation procedure, and papilla regeneration was performed immediately after the second implantation.
Using this technique, papilla regeneration and tight fibrous tissue attachments were achieved simultaneously. Two months after the papilla regeneration procedure, temporary prosthetic restorations were fashioned, and permanent restorations were made after 4 months.
In conclusion, we present a case of an implant-aided prosthetic treatment in which peri-implant plastic surgery techniques were applied in combination to satisfactorily attain functional aesthetic expectations. Peri-implant plastic surgery enables the successful reconstruction and restoration of the balance between soft and hard tissues and allows the option of implant-aided fixed prosthetic rehabilitation. Moreover, in cases that require longterm treatment planning, as in our case, a multidisciplinary approach is most desirable.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


