All published articles of this journal are available on ScienceDirect.
Multidisciplinary Treatment Options of Tooth Avulsion Considering Different Therapy Concepts
Abstract
Background:
Avulsion of permanent front teeth is a rare accident, mostly affecting children between seven and nine years of age. Replanted and splinted, these teeth often develop inflammation, severe resorption or ankylosis affecting alveolar bone development and have to be extracted sooner or later.
Objectives:
The purpose of this study was to evaluate different therapy concepts to create a structured concept for the treatment of avulsions.
Results:
Based on existing therapy concepts, a concept for different initial conditions (dry time, age, growth, tooth, hard and soft tissues) was developed and is presented here.
Conclusion:
A great deal of research has been performed during recent years and guidelines for the management of avulsions have been published. With the help of this literature it is possible to identify the best treatment procedure for each tooth.
Clinical Relevance:
The prognosis of avulsed teeth can be improved by considering evidence-based therapy concepts. Resorption, ankylosis and tooth loss could be minimized.
INTRODUCTION
Avulsion is a traumatic displacement of the tooth from its socket. It is an accident, representing 0.5% to 3% of traumatic injuries [1] in permanent dentition, mostly affecting children between seven and nine years of age [2]. An adequate management within the first half hour is most important for the prognosis of the tooth. Different medical storage media have been reported to be effective in maintaining [3] the periodontal ligament (PDL) cells in a viable state after avulsion, but milk remains one of the most commonly used and recommended storage media [4]. Its main advantages are high availability, a physiologically compatible pH and osmolality with the PDL cells. Depending on the injury to the PDL these replanted teeth often develop surrounding inflammation followed by severe resorption ending up in ankylosis [5]. Ankylosis affects alveolar bone development in younger patients [6]. A great resource of help for dentists in decision-making and choosing treatment procedures is the Dental Trauma Guide (www.dentaltraumaguide.org) [7]. Within this tool Andreasen also provides a prognosis for each form of trauma based on the analysis of innumerous cases. Meanwhile, there is some evidence-based literature that makes it favorable to modify some of these procedures regarding preparation of the root surface, timing of root canal treatment and systemic medication. A lot of research has been performed during the last years and guidelines for the management of avulsions have been published [8, 9]. Reviewing this literature it is possible to identify the best treatment procedure for every tooth, but the information is spread over journals and books of different disciplines in dentistry (endodontic, periodontal, orthodontic, pedodontic or surgical publications). For daily practice, it would be helpful to have structured recommendations for treatment protocols under different initial conditions (dry time, age, growth, tooth, hard and soft tissues) relying on existing evidence-based therapy concepts. The first goal of avulsion treatment is to keep the tooth vital or at least functional in place avoiding resorption and ankylosis resulting in normal growth of the alveolar ridge. If this cannot be achieved it is of utmost importance to prevent the alveolar bone from collapsing due to tooth loss. Alveolar bone structure is necessary for the the placement of an implant after completion of alveolar bone development up to the age of 21 or even later.
MATERIALS AND METHODS
Textmining
The complete Medline/PubMed data was screened for articles about dental avulsion. Specific keywords were used to retrieve about 200 articles. Ten additional records were identified through other sources (books, articles not indexed in PubMed). The abstracts of those records were screened and 130 were excluded due to evidence-based criteria. About 80 full-text articles were included in the synthesis and divided into groups: Endodontics, Periodontics, Orthodontics, Surgery, Therapy and Reviews (Fig. 1). Specialists in the different disciplines read the articles and met weekly to find a consensus for each problem.
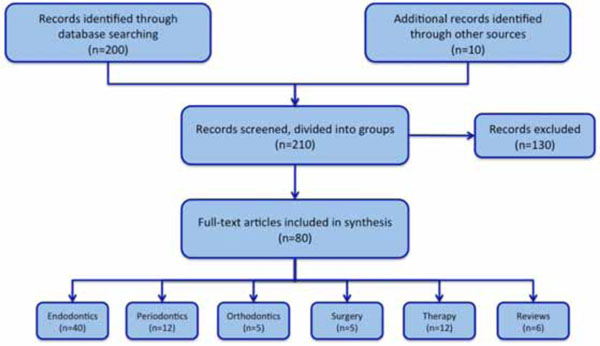
Flowchart of literature synthesis.
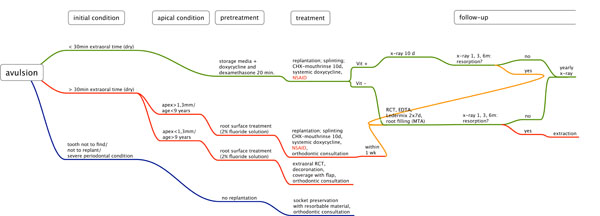
Flow chart for the avulsion of permanent teeth.
With the help of the Flow chart, clinicians obtain a quick overview of evidence-based treatment options for avulsed teeth.

Individualized holder for comparable x-rays.
The holder can easily be individualized with dental impression material (putty silicone).
RESULTS AND DISCUSSION
For easy understanding and fast access a flow chart was developed comprising a synthesis of the evidence-based literature about tooth avulsion. Fig. (2) summarizes the conclusions from the analysis of the literature and offers guidance in determining the optimal treatment concept for any form of tooth avulsion.
Initial treatment
For the initial treatment it is important to get information about the dry time of the avulsed tooth, because cells of the periodontal ligament (PDL) are irreversibly damaged after 30-60 minutes [8, 10, 11]. Damaged PDL cells lead to fast inflammatory resorption accompanied by ankylosis and a negative influence on alveolar bone growth [6].
Dry time < 30min
If the tooth’ dry time was under 30 minutes, it is likely that PDL cells have survived and will regenerate [8, 10, 11]. To minimize the risk of inflammatory or replacement resorption an anti-resorption therapy should be performed. This procedure aims onto defending against inflammation caused by bacterial contamination and/or necrotic cells and tissues. Different regimen have been described using antibiotics The anti-resorptive therapy consists of soaking the tooth into a storage media enriched with 800 µg doxycyline (50 µm/ml) and 640 µg dexamethasone (40 µm/ml) for 20 minutes [12, 13]. That time can be used to inspect and clean the alveolus with 0.9% physiologic saline solution. Afterwards, the tooth is replanted and splinted with a semi-rigid device for instance with a titanium trauma splint (TTS) for 10 days. Additionally the patient is prescribed doxycycline for 5 days. Children under 50 kg receive 100 mg as an initial dose on the first day and 50 mg on the following days [12]. Intolerances are rare, but if present, amoxicillin is a good alternative. Doxycycline leads to no or little tooth discolorations [14].
After removal of the splint, the mobility of the tooth is tested and a vitality test is performed. The assessment of the vitality of traumatized teeth in younger patients is very challenging, due to the lack of reliability on the reaction of the children. Moreover, ice spray or solid CO2 snow are poorly reproducible during the first weeks after trauma, while electric pulp testing or pulse oximetry are more reliable over longer periods [15-17].
Positive Vitality Test
A radiograph should be taken with an individualized holder (Fig. 3) which helps to obtain comparable x-rays from the same angle in subsequent follow-ups. After one, three and six months a new x-ray is taken for early recognition of any signs of resorption. If there is no resorption, a recall examination including x-ray should be performed every year. If there are signs of resorption, a root canal treatment (RCT) might stop the inflammatory process [18]. Further treatment follows the procedure for the negative vitality test.
Negative Vitality Test
If the vitality test is negative after 10 days, there is no chance for revascularisation and RCT has to be performed. To prevent resorption it is important to facilitate diffusion through the dentine by removing the smear layer in the root canal with EDTA irrigation and to put in Ledermix as an intermediate dressing twice for 7 days each time [19, 20]. The root filling should be performed with a dental microscope to insert the MTA apically [21-23]. The backfill of the remaining root canal can be done with gutta-percha. Radiographs should be performed with an individualized holder. After one, three and six months a new x-ray is taken to recognize signs of resorption.
Dry Time > 30min
For extraoral dry times over 30 minutes, it is certain that most PDL cells on the root surface are necrotic and resorptions are to be expected [24]. If possible, an orthodontist should be consulted regarding the expected alveolar bone growth, because there are inter-individual differences in age and growth with the poorest prognosis in children with mature teeth before pubertal spurt [6, 25]. These results suggest that replanting these teeth should be regarded as a temporary solution to preserve bone to gain time for a later prosthetic rehabilitation.
Apical Foramen > 1.3mm
For younger patients (<9 years) with wide apical openings (>1.3mm) an attempt should be made to preserve the tooth. To slow down the resorption process, the root surface is treated with 2% sodium fluoride for twenty minutes after mechanical cleaning [26]. The procedure according to teeth with dry time < 30 minutes and negative vitality test follows. The root canal treatment should be performed within one week after replantation with Ledermix as intermediate dressing, as it was found to result in significant less loss in root mass due to resorption [27, 28].
Apical Foramen < 1.3mm
A tooth with a dry time over 30 minutes and a closed apex has a very poor prognosis, mainly resulting in ankylosis and infra-position due to ongoing skeletal growth. Therefore these teeth cannot be expected to be preserved. The root canal preparation is performed extraorally with Gates-Glidden burs 5-6 (ISO 130-150) and the root surface is treated with 2% sodium fluoride for five minutes to retard resorption. A decoronation is followed by coverage of the remnant root with a flap [29, 30].
Tooth not Found/ not to Replant/ Severe Periodontal Conditions
If the tooth is lost or not to replant due to complicated fracture or if there are poor periodontal conditions, the focus is laid on socket preservation with collagen and/or a biphasic alloplastic slow resorbable bone substitute and a collagen membrane for alveolar ridge preservation [31]. Implant therapy in children and adolescents may influence maxillary and mandibular skeletal and dental growth [32] and should be postponed until the completion of alveolar bone growth. An orthodontist should be consulted to assess the alveolar bone growth and discuss treatment options [33, 34]. Autotransplantation of premolars is also described as a successful treatment option after tooth loss [35].
CONCLUSION
With the help of the flow chart, clinicians can choose evidence-based treatment procedures quickly and easily. Antiresorptive therapy methods are essential for therapy of the avulsed tooth to avoid/minimize growth retardation of the alveolar ridge. The clinician has a structured directory and pathway by which to validate the chances of success using the considered treatment regimen.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Anna-Katharina Gieren, Charité – Universitätsmedizin Berlin, for discussing about periodontal aspects after tooth avulsion.


