All published articles of this journal are available on ScienceDirect.
Morphological and Functional Parameters in Patients with Tooth Wear before and after Treatment
Abstract
Advanced tooth wear often results in lost vertical dimension and impacts facial aesthetics. Complex restorative treatment can replace the lost tooth structure and improve functional occlusal and facial skeleton parameters.
Purpose:
The aim of the study is to assess changes in the morphological and functional occlusal parameters of the facial skeleton after prosthetic rehabilitation that increased lost occlusal vertical dimension.
Material and Methodology:
50 patients with advanced tooth wear were clinically examined, to assess the degree of wear. Each subject underwent cephalometric analysis, digital occlusal analysis, and electromyographic analysis, of the anterior temporalis, superficial masetter, anterior digastric, and the sternocleidomastoid muscles. Prosthodontic treatment was performed to restore the occlusal vertical dimension of each subject’s occlusion, which was followed by repeating the pretreatment analyses. Pre and post treatment parameters were statistically compared.
Results:
Pre-treatment cephalometric analysis showed that lost vertical dimension reduced anterior facial height and resulted in small angular skeletal parameters. Post treatment anterior facial height increased from the increased occlusal vertical dimension. The mean value of functional electrical activity during clenching post treatment, increased compared to pretreatment.
Conclusion:
Increasing the vertical dimension of occlusion improved facial aesthetics by positively affecting facial skeletal angles. The restored occlusal surface morphology changed the pre treatment flat broad occlusal contacts into more point contacts. The increased vertical dimension of occlusion after treatment also increased muscle activity levels over the pretreatment levels after three months period of adaptation.
INTRODUCTION
Advanced tooth wear can be a major source of tooth structure loss that often requires an advanced and costly prosthetic rehabilitation to reconstruct the occlusion. Advanced wear becomes even more serious when observed in relatively young patients, who have a full dentition where, exposed dentin and advanced recession is present on some teeth.
When planning a complete prosthetic rehabilitation, it is important to determine the etiology of tooth wear, the amount of hard tissue loss, the change in the occlusal vertical dimension resultant from the wear, the amount of available interocclusal space required to restore the lost vertical dimension, the causative occlusal scheme, the levels of contractile muscle activity, and untoward changes in facial morphology [1]. The morphology of the face, the existing occlusal vertical dimension, and the amount of available interocclusal space, can all be determined with by cephalometric analysis, combined with the Shimbashi measurement of CEJ – CEJ [2, 3]. Shimbashi measurement refers to the skeletal classes of facial morphology whereby the distance between the cementoenamel junction [CEJ] of the central upper and lower incisors for class I should amount to 17-18 mm.
Provisional treatment that reestablishes the lost vertical dimension, can test the patient acceptance of the reestablished vertical dimension. This can also be evaluated with a mid-treatment cephalometric analysis to determine the correctness of the newly proposed occlusal height for possible use in the final reconstruction.
Defining functional occlusal parameters, as well as measuring the masticatory contractile muscle activity, assists in matching a particular rehabilitated occlusal scheme appropriate for each individual patient. Moreover, mid treatment and post treatment measurements, make it possible to assess that the treatment has physiologically improved the pretreatment condition, so as to better improve the adaptation process to the new occlusal design [4, 5]. A desirable treatment goal is to install well-fitting, high quality restorations, that function under favorable (low-muscle activating) occlusal conditions (short disclusion time in excursions) [6], short occlusion time in closure [7], and a high degree of force equality per arch half [7], so as to provide the patient with a reconstruction that can survive for many years [8, 9].
The aim of the study was to assess the morphological and functional parameters of the facial skeleton before and after prosthetic rehabilitation of the masticatory system in patients with severe pathological tooth wear resulting in lost occlusal vertical dimension.
MATERIALS AND METHODOLOGY
Inclusion and Exclusion Criteria
The data was collected in the Department of Prosthetic Dentistry at the Medical University of Białystok, (Bialystok, Poland), while conforming to the criteria of The Helsinki Declaration, ICH Guideline for Good Clinical Practice [10].
50 patients with advanced tooth wear, lost vertical dimension of occlusion (VDO), and visible exposed occlusal dentin, comprised the subject pool. Sixteen women and 34 men with a mean age of 49.5 ± 9 years were included in the study. Tooth wear patients possessed 22 teeth contacting in 9 opposing functional units (5-6 units of front teeth with a mean of 6 units, and 1-8 units of posterior teeth with a mean 3 pairs).
Inclusion in the study required participants to satisfy the following criteria:
- The presence of widespread advanced tooth wear with multiple sites of exposed occlusal dentin (Tooth Wear Index- TWI on occlusal/incisal surface ≥ 2).
- The presence of a considerable decrease in the occlusal vertical dimension (more than 4 mm measured in the anterior region ).
- Their own teeth demonstrated no decay, and no significant periodontal bone loss.
- No prior prosthetic rehabilitation attempting to treat the lost vertical dimension.
- Healthy adults with no chronic medication use that would affect the oral micro flora or the salivary flow rate.
- Subjects were required to be available to be recalled multiple times during and after the duration of the study.
Exclusion Criteria
Subjects were excluded from the study when they demonstrated:
- No presence of tooth wear on occlusal/incisal surface.
- No decrease in the occlusal vertical dimension.
- Their teeth demonstrated decay and/or significant periodontal bone loss.
- Prior prosthetic rehabilitation was present that restored the lost vertical dimension.
- Unhealthy adults presenting with chronic medication use
- Prior preventive professional application of topical fluoride.
- Unavailability to be recalled multiple times during and after the duration of the study.
All the patients complained about difficulties in chewing, the pain when cold foods were taken and esthetic problems (short teeth, bad shape, discoloration). All included subjects underwent a detailed clinical examination that included periodontal probing, exploration of occlusal surface integrity, and observation of the amount of exposed occlusal dentin. In order to determine the degree of tooth wear, the Smith and Knight index was employed (Tooth Wear Index) [11]. This index is a comprehensive system whereby all four visible surfaces (buccal, cervical, lingual and occlusal-incisal) of all teeth present are scored for wear irrespective of how it occurred (from 0 to 4 where 0- no loss of enamel, 4-complete enamel loss-pulp exposure, secondary dentine exposure),. It measures and monitors multifactorial tooth wear. The distance from the cementoenamel junction between the upper and lower central incisors [CEJ-CEJ] was measured to assist in determining the amount of lost occlusal vertical dimension per subject. Additionally, each subject underwent a morphological evaluation that included lateral skull cephalometric radiographic analysis according to Ricketts and McNamara to determine the linear and angular parameters of the facial skeleton (Fig. 1).
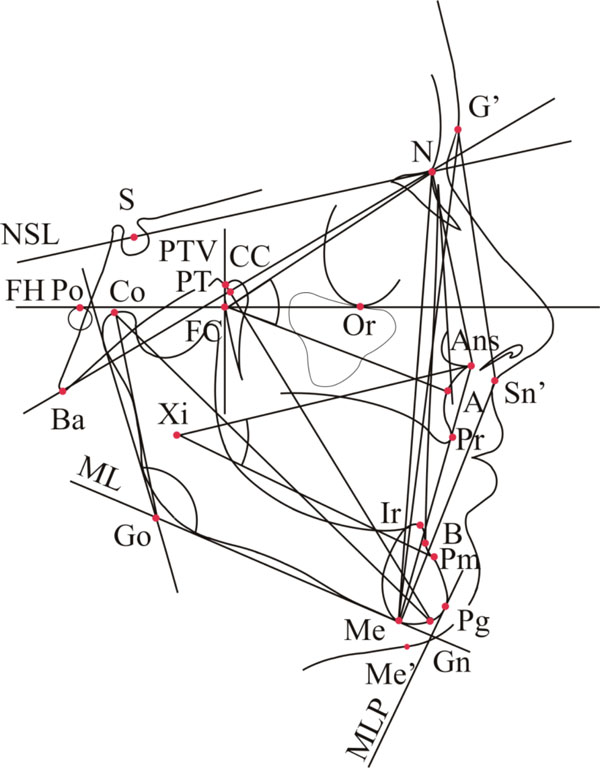
Soft tissue cephalometric landmarks
G’ (Glabella) – the most anterior soft tissue point of the frontal bone, Sn’ – the point at which the nasal septum merges mesially with the upper cutaneous lip in the mid-sagittal plane Me’ (Soft tissue Menton) – the point on the lower contour of the chin opposite to the hard tissue Menton
Skeletal / hard tissue cephalometric landmarks
A (Subspinale) - the deepest point in the midsagittal plane between the anterior nasal spine and prosthion, Pr (Prosthion) - the point of the upper alveolar process that projects most anteriorly in the midline, ANS (Anterior nasal spine) - the anterior point of the nasal floor, B (Sm) (Supramentale) - the deepest point in the midsagittal plane between infradentale and Pg, Ir (Infradentale) - the most anterior point of the alveolar process of the mandible, Co (Condylion) - the most superior posterior point on the outline of the mandibular condyle, Gn (Gnathion) - most anterior and lowest point of the symphysis, Me (Menton) - the lowest point of the contour of the mandibular symphysis, N (Nasion) - most anterior point of nasofrontal suture in the midsagittal plane, Or (Orbitale) - the lowest point on the margin of the orbit, Pm (Suprapogonion) - point where curvature of the anterior contour of the symphysis changes from concave to convex, Po (Porion) - the midpoint on the upper edge of the external auditory meatus, S (Sella) middle point of sella turcica, PT – the junction of the pterygopalatine fossae and foramen rotundum located at the posterosuperior border of the averaged pterygopalatine fossae, Ba (Basion) – the lowest point on the anterior medial margin of the foramen magnum in the mid-sagittal plane, Pg (Pogonion) - the most anterior point on the symphysis of the mandible
Constructional points
Go (Gonion) – formed by the junction of the ramus with the lower border of the mandibular body on its posteroinferior aspect, FC (Facial centre) - intersection of the Frankfort plane and the perpendicular through the posterior side of the pterygomaxillary fissure (PTV), CC (Centre of the cranium) - the point of intersection between the BaN plane and the facial axis (PTGn) plane, Xi (Xilion) - the point placed in the center of the mandibular ascending ramus, determined by the Frankfort plane and pterygomaxillary fissure
Cephalometric planes and lines
PTV (Pterygoid vertical) – used to represent the posterior border of the maxilla. A line perpendicular to FH and tangent to the posterior contour of the PTM (Pterygomaxillary fossa) at the level of the foramen ovale. Anteroposterior extent of the anterior cranial base. Represents the cranial base in the mid-sagittal plane. ML (Mandibular plane) – a line tangent to the most prominent points on the lower border of the mandible, MLP - ML straight line perpendicular to passing through the Pg, NSL (Sella-Nasion plane) – anteroposterior extent of the anterior cranial base. Represents the cranial base in the mid-sagittal plane, FH (Porion-Orbitale plane, horizontal plane, Frankfurt plane) – represents the cranial base.
Standardization Procedure in the Capturing of the Cephalometric Radiographs
Lateral cephalograms were taken from all subjects by a single technician using the same radiographic machine (Orthoceph OC 100 Dental X-ray System; Instrumentarium Corporation Imaging Division, Tuusula, Finland). The recording procedure was standardized as follows: for each subject, the distance between the focus and the mid-sagittal plane was kept constant at 152 cm, while the distance between the film and the mid-sagittal plane was kept constant at 10 cm. Each patient was exposed to 0.15 mSv of radiation. The values measured were not corrected for linear enlargement. The patient was instructed not to swallow during the radiographic exposure.
Functional Analysis was Performed as Follows
Occlusal analysis was performed with a digital occlusal analysis system (T-Scan II for Windows, Tekscan Inc., South Boston, MA, USA). This occlusal technology records dynamic movies of the occlusion that isolates and displays the relative force of each occlusal contact point across elapsed time. Both centric occlusion and lateral excursive movements can be recorded and played back incrementally for clinical observation. The data can be saved on the hard drive to provide visual documentation of the recorded occlusal function.
Electromyographic examination of the muscle activity levels of four pairs of the masticatory muscles was performed. The anterior temporalis, superficial masetter, anterior bellies of the digastrics, and the sternocleidomastoid muscles, were all recorded simultaneously with the BioEMG (BioResearch, Inc., Milwaukee, Wisconsin, USA). The sample rate was 1000 samples/second for each channel. The filtering is to a bandwidth from 30 Hz to 500 Hz. BioEMG was synchronized with the T-Scan II, during maximal clench and mouth opening. The T-Scan II/BioEMG synchronization module allows for simultaneous acquisition of occlusal function and muscle activity resultant from that occlusal function [12]. For each subject, the maximal clench and mouth opening functional T-Scan/BioEMG measurements were recorded three times, with 1 minute of rest between recordings.
Upon completion of the preoperative data gathering (as previously described), all subjects underwent prosthetic rehabilitation to rebuild the lost vertical dimension. Diagnostic casts were obtained and articulated at an open vertical dimension. Diagnostic waxing was accomplished and provisional restorations were created that increased the vertical dimension intraorally. Clinically, the vertical dimension increased on average 4.5 mm ± 1.5.
The three-month period of observation of the provisional treatment did not reveal any side effects related to the prosthetic treatment e.g. pain, chewing problems, fractures of provisional restorations. In order to evaluate the results of the provisional treatment prior to the final restoration phase, another set of lateral cephalograms were obtained from each subject to observe any facial morphological and skeletal changes resultant from the new vertical dimension of occlusion. The same radiographic standardization was once again utilized, to record dimensionally similar provisional phase cephalograms. Following a three-month period of adaptation to the new occlusal vertical dimension, the provisional appliances were replaced with permanent restorations. Metal framed-porcelain crowns were applied to heavily restored teeth and composite was applied to cover mild and small tooth damage. Lost teeth were replaced using removable dentures or metal-porcelain bridges if it was possible. The treatment was made in both jaws. The new occlusal scheme provided to the patients was group function (canines and first premolars were in contact during lateral movement). On the day of final restoration placement, and 3 months post-insertion, the same functional examinations were all repeated in the same fashion as during the pretreatment examinations.
Ethical Approval
This protocol was approved by the Local Ethical Committee of the Medical University of Bialystok, Poland, with an approval number of R-I-003/6/2006. Informed consent was obtained from each participant at the beginning of the study prior to confirmation of their eligibility for the study. The participants were able to withdraw from the study at any time and for any reason without prejudice.
Statistical Analysis
A statistical analysis of all of the studied attributes was carried out. In the case of quantitative attributes, average and dispersion measures were used, i.e., arithmetic mean and standard deviation. The levels of studied attributes between the groups were compared using the t-test. The strength of relationships between pairs of measurable parameters was determined using Pearson’s correlation coefficient, and its significance was assessed using the t-test for the correlation coefficient. Differences and relationships were considered to be statistically significant at p<0.05.
Results
In total, 1017 teeth from the study group were evaluated for tooth wear, based upon four surfaces for each tooth. The Smith and Knight TWI values of ≤ 1 were determined for the buccal, linqual and cervical surface worn surfaces. The most evident destruction from wear was observed on occlusal and incisal surfaces where the mean value of TWI for these surfaces was 2.27 mm ± 0.52.
A reduced anterior facial height was an observable consequence of tooth wear visible in the pre-treatment cephalometric analyses when compared to post-treatment cephalometric analyses. It was consistently noted that the distance from the lower central incisor to the N –B line was usually too small when compared to normative values. Angular parameters indicated that the ANB angle, the mandibular inclination angle (NSL/ML), N-Go-Me angle, and the basal angle, were also small when compared to their respective normative values. Additionally, the interincisal angle and facial axis angle were observed to be too large when compared to normative values.
Following placement of the provisional restorations, significant differences were noted within both the linear and angular cephalometric parameters, when compared to the pre treatment low vertical dimension condition. Anterior face height increased with the increased occlusal vertical dimension, and there was increase in the angle of the mandibular inclination, the N-Go-Me angle and the base angle, while the facial axis angle decreased.
The increased vertical dimension of occlusion often resulted in a new antero-posterior maxillomandibular relationship, that demonstrated a reduced SNB angle and an increased ANB angle. The restoration of vertical dimension in the anterior region resulted in a considerable increase in the distance from the lower central incisor to the NB line, which also reduced the interincisal angle (Table 1).
The Comparison of Linear and Angular Parameters Describing Morphological Features of the Facial Skeleton before and after Treatment. Mean Values ± SD were given
| Feature | Before Treatment n=50 | After Treatment n=50 | P< |
|---|---|---|---|
| Linear Measurements (mm), | |||
| Length of anterior base | 73.3 ± 3.9 | 73.4±3.9 | |
| Length of maxilla | 57.5 ± 3.4 | 57.7± 3.6 | |
| Length of mandible | 79.5 ± 5.2 | 79.5± 4.9 | |
| Distance +1 from NA | 3.5 ± 3.5 | 3.9±3.6 | |
| Distance -1 from NB | 3.0 ± 1.9 | 3.5±2.8 | 0.05 |
| The anterior vertical dimension of the face | 118.7 ± 9.0 | 121.5± 10.2 | 0.001 |
| The posterior vertical dimension of the face | 76.9 ± 8.5 | 76.2 ± 8.6 | |
| Angular Measurements ( 0 ) | |||
| SNA angle | 82.3 ± 4.4 | 82.4 ± 4.2 | |
| SNB angle | 80.9 ± 4.8 | 80.4 ± 4.4 | |
| ANB angle | 1.5 ± 2.0 | 2.6 ± 2.9 | 0.002 |
| N-Ba-S angle | 127.7 ± 5.7 | 127.4 ± 5.8 | |
| NSL/NL( maxillary inclination) | 7.0 ± 2.9 | 7.1 ± 3.2 | |
| NSL/ML( mandible inclination) | 23.6 ± 6.8 | 27.5 ± 6.1 | 0.001 |
| Inclination of upper incisors | 72.3 ± 11.4 | 72.6 ± 10.8 | |
| Inclination of lower incisors | 87.1 ± 8.1 | 86.4 ± 7.8 | |
| Inter-incisor angle | 141.1 ± 9.1 | 138.7 ± 13.3 | 0.002 |
| Ar-Go-N angle | 50.9 ± 3.6 | 49.5±3.7 | |
| N-Go-Me angle | 68.7 ± 4.9 | 71.3±4.5 | 0,001 |
| Basal angle | 18.8 ± 6.8 | 25.6±5.7 | 0.001 |
| Facial axis angle | 92.3 ± 4.7 | 89.7±9 | 0.001 |
P< statistically significant difference between the result before and after the treatment
Analysis of the masticatory muscle activity levels showed that, on the prosthesis insertion day, the mean value of the electrical activity during clenching within the temporal muscles, the masseter muscles, and the digastric muscles, had decreased, while electrical levels increased within the sternocleidomastoid muscle. After a 3 month period of adaptation the electrical activity of the temporalis and masetter muscles had increased compared to pretreatment levels. The mandibular opening electrical activity level differences were not statistically significant from pre treatment to provisional VDO thru to the final VDO, an increase in the activity of masetter and digastric levels was observed (Table 2).
The Comparison of Mean Value Activities (µV) of Masticatory Muscles During Maximal Teeth Clench and Mouth Opening before and after the Treatment. Mean Values ± SD were Given
| Before Treatment | The1st Day after Treatment | Three Months Later | |
|---|---|---|---|
| Clench | |||
| M.T. (µV) | 70.9 ± 29.3 | 56.6 ± 28.8 | 80.0 ± 34.4 # |
| M. M. (µV) | 84.9 ± 31.8 | 74.7 ± 21.8 | 102.8 ± 34.8 *, # |
| M. D. (µV) | 14.5 ± 6.2 | 12.9 ± 5.2 | 15.6 ± 6.4 |
| M. SCM. (µV) | 11.9 ± 5.8 | 20.1 ± 6.3 | 10.5 ± 4.7 |
| Opening | |||
| M. T. (µV) | 9.2 ± 3.9 | 11.3 ± 4.9 * | 9.4 ± 3.1 |
| M. M. (µV) | 8.5 ± 3.9 | 12.0 ± 4.7 * | 13.9 ± 2.5 * |
| M. D. (µV) | 19.7 ± 8.9 | 18.1 ± 8.4 | 21.4 ± 9.8 # |
| M. SCM. (µV) | 7.8 ± 2.9 | 7.2 ± 3.6 | 7.3 ± 3.0 |
M.T.- temporal muscles, M.M.- masseters, M.D.- digastric muscles, M.SCM- sternocleidomastoides
* p< 0,05 in relation to the result before treatment
# p<0,05 between the 1st day after treatment and 3 months later
The results of the occlusal measurements made with the T-Scan II system are presented in Table 3. Changes from prosthetic treatment statistically shortened the occlusion time (the elapsed time from first occlusal contact to static intercuspation) when compared to pre treatment durations, where post treatment approached ideal (≤ 0.2 sec.). The occlusion time was observed to remain stable for three months after the prostheses were inserted. The post treatment disclusion time [6] did not deviate from the reported norm (≤ 0.4 sec. per excursion) and was not significantly different from pretreatment levels.
The Comparison of Occlusal Parameters before the Treatment, on the First day after the Treatment and after Three Months after the Treatment. Mean Values ± SD were Given
TO- the time of occlusion , i.e. the time from the first tooth contact to the maximal intercuspation, TDR- the time of disclusion right, the time from the maximal intercuspation to complete disclusion during the right Lateran movement, TDL- the time of disclusion left, the time from the maximal intercuspation to complete disclusion during the left lateral movement
* p<0,05 in relation to the result before treatment.
DISCUSSION
Patients with advanced tooth wear have been shown to demonstrate a reduction of the vertical dimension of the face, a smaller angle of mandibular inclination, a smaller basal angle, a small mandibular angle, and more obtuse interincisal angle [2, 13, 14]. The study patients did present with these morphological facial skeleton attributes.
A relationship between neuromuscular activity and linear parameters of the facial skeleton is known to exist [15]. However, why muscle activity levels improved from a change in the anterior-posterior maxillomandibular relationship remains unclear [16, 17]. Physiological occlusion exists when there is functional balance between all the elements of the stomatognathic system, with the morphology of the mandible and the maxillomandibular relationship [18]. The activity and the movements of the mandible are affected by many different factors. Sensory receptors of periodontium, periosteum, temporomandibular joint, tongue and other soft tissues of oral cavity, deliver information through the central nervous system that is subject to constant analysis by the jaw muscles. Pain stimuli can be avoided involuntarily, while the movements of all the mobile structures during function can proceed with minimal risk to the many structures of the stomatognathic system [19].
It has been shown during mastication that the largest number of occlusal contacts tends to occur in the intercuspal position [4]. In this position, the mandibular adductors are able to generate maximal masticatory force. The study subjects presented with advanced tooth wear had totally flat occlusal surfaces. It is quite possible that teeth with a flat occlusal surface resulted in a greater number of intercuspal occlusal contacts. But, it was not possible to determine if the subjects could generate weaker or stronger occlusal forces as a result of the changes in configuration of occlusal surface. Nevertheless, the study subjects demonstrated lower mean electrical activity within the adductor muscles during clench, than in the post treatment condition.
It has also been shown that the facial skeleton is less affected by occlusal force levels, than from prolonged durations of muscle activity [15, 20]. Kiliaridis noted a significant correlation between pathological tooth wear, muscle function, and the patho-morphological pattern of the facial skeleton [21]. After registering the electrical activity of masseter and temporal muscles for a period of three hours per day, Ueda reported a positive correlation between the duration of temporal muscle activity, and changes within the morphological features of the facial skeleton. However, other authors have shown that a negative correlation exists between masseter muscle activity, and changes within the morphological features of the facial skeleton [22, 23].
The intercuspal position provides a stable point during a mandibular clench, because the occlusal forces are placed upon the teeth in the most advantageous location (center of the teeth). This is where the applied load can be best dispersed to protect the teeth and temporomandibular joints from overloading [24].
Prosthetic treatment of the advanced tooth wear improved the aesthetics of the face. The cephalometric analyses pre and post treatment, showed statistically significant changes in a number of facial angle proportions (Table I). The increased vertical dimension resultant from the prosthetic treatment, improved the cephalometric analysis to approximately known reference values [25].
A change in the pattern of occlusal contacts was also observed. Pre treatment the subjects all demonstrated completely flat occlusal contacts resultant from longstanding occlusal wear. Post treatment, the flat surface contacts were replaced with multipoint contacts and increased cuspal morphology. During the three-month period of observation, the T-scan confirmed stability of the occlusal conditions. The occlusion and disclusion times maintained similar duration from the end of the prosthetic rehabilitation to the end of the 3 month period of adaptation.
The prosthetic rehabilitation resulted in the creation of adequate occlusal-articulatory conditions, which led to an improved muscle response. It was initially observed immediately after placement of the new prosthetic appliances that the clench muscle activity levels decreased within the temporal and masseter muscles. However, after 3 months of adaptation to new occlusal vertical dimension, the muscle activity levels of these same mandibular muscles increased significantly, to higher values as compared to pretreatment (see Table 2). This type of positive muscle response to increasing the vertical dimension of occlusion, was reported by Ferarrio [17, 21]. Lastly, it has been shown that the electrical activity levels of the masseter muscles are positively influenced by the presence of point contacts, as compared to flatter contacts [23]. The results of this study corroborate the findings of these previous studies by indicating that point contacts increased masseter electrical activity.
CONCLUSION
- Cephalometric analysis showed that increasing the vertical dimension of occlusion positively affected many of the linear and angular morphological facial skeleton parameters.
- Creating point contacts with the restorations also increased muscle activity levels over the pretreatment levels after three months period of adaptation comparing to pretreatment situation obtained with flat occlusal surface contacts.
- The occlusion time improved significantly when the vertical dimension of occlusion was restored, but the disclusion time was not appreciably changed.
- TMJ disorders did not occur after treatment in the group of patient being treated.
CONFLICT OF INTEREST
The research was carried out within the research project of Ministry of Science and Higher Education no. N 403 051 32/2525.
ACKNOWLEDGEMENT
Special thanks to Dr. Robert Kerstein for his guidance in the preparation of this manuscript.


