All published articles of this journal are available on ScienceDirect.
Clinical Performance of a New Biomimetic Double Network Material
Abstract
Background:
The development of ceramics during the last years was overwhelming. However, the focus was laid on the hardness and the strength of the restorative materials, resulting in high antagonistic tooth wear. This is critical for patients with bruxism.
Objectives:
The purpose of this study was to evaluate the clinical performance of the new double hybrid material for non-invasive treatment approaches.
Material and Methods:
The new approach of the material tested, was to modify ceramics to create a biomimetic material that has similar physical properties like dentin and enamel and is still as strong as conventional ceramics.
Results:
The produced crowns had a thickness ranging from 0.5 to 1.5 mm. To evaluate the clinical performance and durability of the crowns, the patient was examined half a year later. The crowns were still intact and soft tissues appeared healthy and this was achieved without any loss of tooth structure.
Conclusions:
The material can be milled to thin layers, but is still strong enough to prevent cracks which are stopped by the interpenetrating polymer within the network. Depending on the clinical situation, minimally- up to non-invasive restorations can be milled.
Clinical Relevance:
Dentistry aims in preservation of tooth structure. Patients suffering from loss of tooth structure (dental erosion, Amelogenesis imperfecta) or even young patients could benefit from minimally-invasive crowns. Due to a Vickers hardness between dentin and enamel, antagonistic tooth wear is very low. This might be interesting for treating patients with bruxism.
INTRODUCTION
Since there is a great variety of dental ceramics and a large selection of composite resin materials on the market, it is questionable why there is a need for a new material. Table 1 lists important parameters to compare zirconia, feldspar, lithium-disilicate and composite resins with each other. Advantages of ceramics are a high flexural strength and a great color stability, while disadvantages are high antagonistic tooth wear and loss of tooth structure due to a minimum thickness of 1.5 to 2.0 mm. These two parameters are better for composite resins, but the wear of the material itself is higher. The table also lists Youngs modulus and Vickers hardness for dentin and enamel. While ceramics are stiffer and harder than natural tooth structure, composite resins show lower values. These parameters show that there is a need for a material that combines the advantages of ceramics with those of composites with the focus on the prevention of natural tooth structure. Therefore Youngs modulus should come close to dentin, hardness should be between enamel and dentin. A minimum of wear of both the material itself and the antagonistic tooth, would be desirable and the most important requirement for a new material would be a very low minimum thickness to preserve sound tooth structure.
Comparison of Important Parameters of Zirconia, Feldspar, Lithium-disilicate, Composite Materials and ENAMIC. Refer-ences are given in Parentheses
| Unit | Dentin | Enamel | Zirconia | Feldspar | Composites | ENAMIC | |
|---|---|---|---|---|---|---|---|
| Flexural strength | MPa | <207 [6-8] | <180 [9, 10] | <620 [11-13] | <150 [13, 14] | <135 [15-17] | 150 [2] |
| Weibull modulus | / | / | / | 4-14 [18, 19] | 6-23 [13, 20] | <13 [21, 22] | 20 [2] |
| Youngs modulus | GPa | <25 [23-25] | <94 [23, 24] | <400 [26, 27] | >50 [20, 26] | <17 [28] | 30 [2] |
| Vickers hardness | GPa | <1 [23-25] | <6 [24, 25, 29] | 10-12 [12, 27, 30] | >6 [31] | <6 [28, 32] | 2.5 [2] |
| Wear | m | / | / | <1 [33, 34] | <1 [14] | >20 [35, 36] | >1 [37] |
| Antagonistic wear | m | / | / | 84 [34, 38] | 53 [39] | <10 [40, 41] | 28 [37] |
| Color stability | dE | / | / | <1 [42, 43] | <1 [44, 45] | >2 [46, 47] | <1 [37] |
| Min. thickness | mm | / | / | >0.5 [48, 49] | >1.0 [50-52] | No [53, 54] | >0.2 |
The new VITA ENAMIC material combines the properties of ceramic and polymer. It consists of a hybrid structure with two interpenetrating networks of ceramic and polymer, a so-called double network hybrid (DNH). Table 1 also offers all parameters of ENAMIC compared to those of groups of materials available on the market. Due to the fine structure of feldspar ceramic and the acrylate polymer network, this material has a similar abrasion, high flexural strength and an elasticity close to dentin. The Vickers hardness was evaluated with values between those for dentin and enamel. Wear is comparable to common dental ceramic, while antagonistic tooth wear is lower at the same time. For the preservation of tooth structure the material can be milled very thin (0.2-0.5mm; VITA Zahnfabrik). The Weibull modulus, which describes the range of fracture, the reliability and strength of a material, is surprisingly high. Fig. (1) shows a SEM micrograph of a Vickers hardness test on a ceramic on the left side (Mark II, VITA Zahnfabrik). The typical crack line is clearly visible. The same test was performed with the hybrid ceramic on the right side. The crack line is is stopped by the interpenetrating polymer within the hybrid network. According to the manufactorer´s instructions the material can be used for single crowns. The purpose of this study was to evaluate the clinical performance of ENAMIC for a non-invasive treatment approach of severe dental erosions.
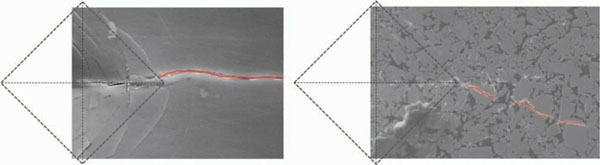
Vickers hardness: SEM micrographs of Vickers hardness tests of ceramics (Mark II) on the left side and ENAMIC on the right side. The ceramic shows a typical crack line, while the crack line of ENAMIC is thinner and hard to find.
MATERIALS AND METHODOLOGY
A 36-year-old female patient came to our department consulting us because of her teeth, that were extensively eroded due to gastroesophageal reflux disease as can been seen at the palatal area in the upper jaw and the buccal area in the lower jaw (Fig. 2).

Initial situation: Upper (left) and lower jaw (right) at the initial situation. Severe loss of tooth structure due to anorexia nervosa.
She suffered from dental sensitivity and poor esthetics. There was a loss of occlusal vertical dimension of about 3 mm. Splints were used to increase the vertical dimension from 1.5 to 3 mm requiring six months. Without any preparation, impressions of the upper and lower jaws were taken using Dimension Penta H (3M Espe, Neuss, Germany) and Honigum Light (DMG, Hamburg, Germany). Interocclusal as well as laterotrusion and mediotrusion records were obtained. The models were scanned by a Cerec 3D camera to obtain an optical impression based on the stone model. From the virtual model and using Sirona In-Lab, V 3.10, dental database design mode, full coverage restorations were designed and milled from VITA ENAMIC blocks (VITA Zahnfabrik, Bad Säckingen, Germany). The produced crowns had a thickness ranging from 0.5 to 1.5 mm. At the try-in, marginal fit and interproximal contact points were checked carefully before insertion. The operation field was isolated using OptraGate (Ivoclar Vivadent), cotton rolls and high-velocity suction. Two crowns in both upper quadrants (one on the first premolar and one on the molar) were cemented simultaneously in order to guarantee a balance of occlusal contacts. The surfaces intended for bonding were sandblasted with 50 µm aluminum oxide powder (Microetcher Danville, 2 bars) and then cleaned with 37% phosphoric acid for 20 seconds. A two-component adhesive: OptiBond FL (Kerr Dental, Rastatt, Germany) was used on both tooth and restoration surfaces. Following air thinning, the adhesive on the teeth was light-cured. A thin layer of Variolink II A2 (Ivoclar Vivadent) was brushed into the crowns that were subsequently seated immediately intraorally. The restorations were light-cured for 60 s from each side. Margins were finished with a micropreparation diamond (Komet/Brasseler, Lemgo, Germany) and polishing disks. Occlusal contacts were checked carefully with occlusal adjustment foil. The crowns for the second premolar and molar were inserted similarly paying special attention to the interproximal contact points. The same procedure was repeated for the lower jaw and anterior teeth were adapted to the new situation using composite resin (Tetric Ceram A3, Ivoclar Vivadent). The patient was examined two weeks later (Fig. 3). All crowns were intact, soft tissues appeared healthy, no discolorations to observe so far and this was achieved with no loss of tooth structure. The patient was satisfied with the treatment.

Final situation: Upper (left) and lower jaw (right) at the first recall after insertion of ENAMIC crowns
RESULTS
To evaluate the clinical performance and durability of the crowns, the patient was examined half a year later (Fig. 4 and 5) and one year later. The crowns were still intact and soft tissues appeared healthy. The photos were taken prior to cleaning the teeth. No discolorations were evaluated but plaque accumulation at the cervical margins was visible.

Recall situation: Upper (left) and lower jaw (right) at the second recall after insertion.

Recall situation: Right and left side at the second recall after insertion.
DISCUSSION
Esthetic and functional rehabilitation are always associated with ceramic restorations. Therefore it is necessary to remove healthy tooth structure to achieve a shoulder/chamfer and a circular minimum thickness of 1.5mm. In some cases composite materials can be used, but it takes a lot of valuable chair-time and porosities are likely to appear [1]. To overcome these problems, new CAD/CAM materials have been developed in the last years and there are several polymer-infiltrated-ceramic-network materials (PICN) on the market now [2]. PICN materials have mechanical properties that imitate natural teeth, which is a new approach in restorative dentistry. Youngs modulus is close to dentin, Vickers hardness lies between enamel and dentin. These materials can be milled to thin layers, but are still strong enough to prevent cracks which are stopped by the interpenetrating polymer within the network. Depending on the clinical situation, minimally- up to non-invasive restorations can be milled. Therefore, PICN materials might be interesting for treating younger patients [3], patients suffering from hereditary diseases, such as Amelogenesis imperfecta [4] or patients with bruxism or dental erosions [5].
Since these materials are new on the market, long-term in-vivo studies are still in progress. The shade range is limited and there is no information on the durability regarding cervical areas or discolorations. Nevertheless, novel PICN materials are promising and further research should be performed.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
The authors would like to thank Schilles/Hütten dental laboratory for their excellent work.


