All published articles of this journal are available on ScienceDirect.
Benign Oral Masses in a Northern Jordanian Population-a Retrospective Study
Abstract
The aim of this study was to evaluate the relative frequencies, types and distribution of benign oral masses in North Jordanians. The records of the Department of Pathology at Jordan University of Science & Technology were reviewed and analyzed for patients with benign oral soft tissue masses, received during an 11-year period (1991-2001). The main outcome measures were patients’ age and sex, and the mass type and location. A sum of 818 benign oral soft tissue masses (4% neoplastic and 96% non-neoplastic) was analyzed. Common benign neoplasms were salivary pleomorphic adenoma and lipoma. Non-neoplastic lesions consisted of traumatic (43%) inflammatory/ infective (33%), cystic (14%) and developmental (9%) lesions. Common non-neoplastic lesions were fibroepithelial polyp, pyogenic granuloma, mucoceles, hemangioma and squamous papilloma, in a descending order. There were 330 (40%) males and 488 (60%) females with a male to female ratio of 1: 1.5. The mean age was 33 years, with the majority in the 2nd, 3rd and 4th decades. The sites commonly affected by benign neoplasms were the palate, tongue, upper lip and buccal mucosa, in a descending order and the sites commonly affected by non-neoplastic lesions were the gingiva, buccal mucosa, lower lip and tongue in a descending order. It is concluded that some of the features of benign oral masses in north Jordanians published in this paper are similar to those from other countries, and some are different. Further nationwide population-based surveys are needed to further define the epidemiology of benign oral masses among Jordanians.
INTRODUCTION
The appearance of benign oral soft tissue masses can occasionally resemble malignant tumors. It is, therefore, crucial to distinguish benign from malignant masses, and in order to make a proper diagnosis, the clinical characteristics of benign oral soft tissue masses needs to be well known. Most benign oral soft tissue masses have a specific age and sex distribution and preferable locations in the oral cavity.
Benign oral soft tissue masses encompass a wide variety of mass lesions. Characteristically they all share the property of being exuberant with minimal growth into deeper tissues. These lesions can be either neoplasm or non-neoplasms. Non-neoplastic lesions are usually inflammatory or represent a reaction to some kind of irritation or low-grade injury. Neoplasms on the other hand, represent a process characterized with progressive autonomous growth [1]. Although oral neoplasms can be either benign or malignant, the majority of oral masses have a benign nature. Clinical differential diagnosis of oral lesions is often dependent on obvious changes in color, size, consistency, and relation to neighboring structures. Knowledge of the frequency and distribution of such lesions is also essential when establishing a diagnosis and putting forward a proper treatment plan.
Despite a considerable volume of literature written about benign oral soft tissue masses in people from different countries, there is very little documentation of the prevalence of such lesions in Jordanians or any other Arab population. The purpose of this retrospective study was, therefore, to analyze the frequency and distribution of the various types of benign oral soft tissue masses found in biopsy specimens taken from northern Jordanians, during an 11-year period starting 1991 and ending 2001.
MATERIALS AND METHODS
Data included in this retrospective study were collected, by the author, after reviewing all reports from the records of the Department of Pathology at Jordan University of Science & Technology. The Department of Pathology receives all biopsy specimens, including those from the oral and maxillofacial area, from all hospitals in north Jordan, serving approximately 30% of the Jordanian population living in four different governorates. The primary source of tissues was from the 6 main hospitals in North Jordan. Biopsies from the oral and maxillofacial area are usually examined and diagnosed by an oral and maxillofacial pathologist. Tumor cases are routinely discussed in scheduled departmental meetings attended by a panel of 4 general pathologists and 2 maxillofacial pathologists. The records of patients with biopsied benign oral soft tissue masses received during an 11-year period from 1991 to 2001, were retrieved, reviewed and analyzed by the authors. For a case to be included the following parameters had be present in the patient’s record: age and sex, and the tumors’ location and type. Lesions were classified according to Scully and Porter [2] into neoplastic and non-neoplastic, and non-neoplastic lesions were further classified into developmental, inflammatory, traumatic and cystic. Data were placed on prepared Microsoft Excel spreadsheets and were evaluated using this software. Patient confidentiality was maintained during this study.
RESULTS
Types of Swellings
There were 823 cases of benign oral soft tissue masses, 5 were excluded due to incomplete information and the remaining 818 benign oral soft tissue masses were analyzed. Among these, 36 (4%) were neoplastic, and 782 (96%) were non-neoplastic. The tissue of origin of neoplasms was epithelial in 18 (50%) cases and mesenchymal in 18 (50%) cases. Common benign neoplasms were salivary pleomorphic adenoma and lipoma (Table 1).
Tissue Origin and Type of Benign Oral Soft Tissue Masses and their Gender Distribution
| Tissue Origin | Lesion | No (%) | Male (%) | Female (%) | % All1 | ||||
|---|---|---|---|---|---|---|---|---|---|
| NEOPLASMS | |||||||||
| Epithelial | Myoepithelioma | 5 | (14) | 0 | 0 | 5 | (24) | 1 | |
| Pleomorphic adenoma | 13 | (36) | 8 | (53) | 5 | (24) | 2 | ||
| total | 18 | (50) | 8 | (53) | 10 | (48) | 2 | ||
| Mesenchymal | Angiokeratoma | 1 | (3) | 1 | (7) | 0 | 0 | 0.1 | |
| Angioleiomyoma | 1 | (3) | 1 | (7) | 0 | 0 | 0.1 | ||
| Granular cell tumor | 2 | (6) | 0 | 0 | 2 | (10) | 0.2 | ||
| Lipoma | 6 | (17) | 2 | (13) | 4 | (19) | 1 | ||
| Neurofibroma | 5 | (14) | 3 | (20) | 2 | (10) | 1 | ||
| Schwanoma | 3 | (8) | 0 | 0 | 3 | (14) | 0.4 | ||
| total | 18 | (50) | 7 | (47) | 11 | (52) | 2 | ||
| Total | 36 | (100) | 15 | (100) | 21 | (100) | 4 | ||
| NON-NEOPLASMS | |||||||||
| Developmental | Hemangioma | 72 | (9) | 35 | (11) | 37 | (8) | 9 | |
| Lymphangioma | 1 | (0.1) | 1 | (0.3) | 0 | (0) | 0.1 | ||
| total | 73 | (9) | 36 | (12) | 37 | (8) | 9 | ||
| Cysts | Dermoid | 6 | (1) | 1 | (0.3) | 5 | (1) | 1 | |
| Epidermoid | 4 | (1) | 2 | (1) | 2 | (0.4) | 0.5 | ||
| Gingival | 3 | (0.4) | 1 | (0) | 2 | (0.4) | 0.4 | ||
| Mucocele | 88 | (11) | 49 | (16) | 39 | (8) | 11 | ||
| Ranula | 9 | (1) | 1 | (0.3) | 8 | (2) | 1 | ||
| total | 110 | (14) | 54 | (17) | 56 | (12) | 13 | ||
| Traumatic | Denture induce hyperplasia | 26 | (3) | 10 | (3) | 16 | (3) | 3 | |
| Fibroepithelial polyp | 228 | (29) | 78 | (25) | 150 | (32) | 28 | ||
| Fibrous epulis | 51 | (7) | 21 | (7) | 30 | (6) | 6 | ||
| Focal gingivitis | 28 | (4) | 9 | (3) | 19 | (4) | 3 | ||
| Neuroma | 3 | (0.4) | 0 | (0) | 3 | (1) | 0.4 | ||
| total | 336 | (43) | 118 | (38) | 218 | (46) | 41 | ||
| Inflammatory/infective | Abscess | 12 | (2) | 4 | (1) | 8 | (2) | 1 | |
| Peripheral giant cell granuloma | 47 | (6) | 15 | (5) | 32 | (7) | 6 | ||
| Pyogenic granuloma | 148 | (19) | 56 | (18) | 92 | (20) | 18 | ||
| Squamous papilloma | 50 | (6) | 28 | (9) | 22 | (5) | 6 | ||
| total | 257 | (33) | 103 | (33) | 154 | (33) | 31 | ||
| Others | 6 | (1) | 1 | (0) | 5 | (1) | 1 | ||
| Total | 782 | (100) | 312 | (100) | 470 | (100) | 96 | ||
| Total | 818 | 327 | 491 | 100 | |||||
1 Percentage out of all benign oral soft tissue mass.
Non-neoplastic lesions consisted of 336 (43%) traumatic lesions, 257 (33%) inflammatory/ infective lesions, 110 (14%) cystic lesions and 73 (9%) developmental lesions. Common non-neoplastic lesions were fibroepithelial polyp, pyogenic granuloma, mucoceles, hemangioma and squamous papilloma, in a descending order (Table 1).
Gender and Age
Benign oral soft tissue masses included in this series were biopsied from 330 (40%) males and 488 (60%) females with a male to female ratio of 1: 1.5. Age ranged from 1 to 93 years (mean of 33 years, standard deviation 19 years). The majority of patients (59%) were in their second, third and fourth decades. Fig. (1) shows the distribution of each age group as related to gender. Pleomorphic adenoma was the most common benign neoplasms in all age groups (Table 2). Mucocele was the most common non-neoplastic lesion in the first decade. From the second decade onwards, fibroepithelial polyp was the most common non-neoplastic lesion (Table 2).
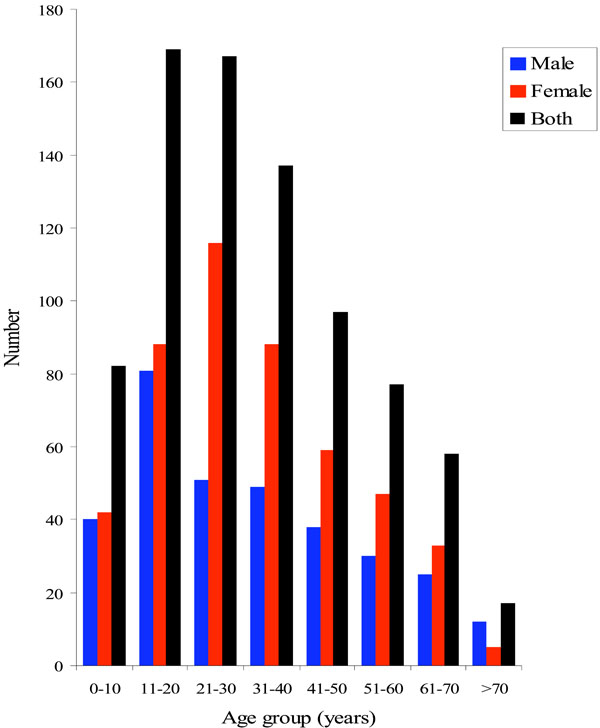
Age and gender distribution of benign oral masses in Jordanians (n=818).
Age Distribution of Benign Oral Soft Tissue Masses
| Lesion | Age Group (Years) | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 0-10 | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | >70 | ||
| NEOPLASMS | |||||||||
| Angiokeratoma | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Angioleiomyoma | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Granular cell tumor | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| Lipoma | 0 | 1 | 2 | 3 | 0 | 0 | 0 | 0 | 6 |
| Myoepithelioma | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 5 |
| Neurofibroma | 1 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 5 |
| Pleomorphic adenoma | 0 | 4 | 6 | 1 | 1 | 1 | 0 | 0 | 13 |
| Schwanoma | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 3 |
| Total | 1 | 11 | 13 | 5 | 2 | 2 | 0 | 2 | 36 |
| NON-NEOPLASMS | |||||||||
| Abscess | 1 | 2 | 1 | 6 | 2 | 0 | 0 | 0 | 12 |
| Denture induced hyperplasia | 0 | 0 | 3 | 2 | 3 | 6 | 11 | 1 | 26 |
| Dermoid cyst | 4 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 6 |
| Epidermoid cyst | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 4 |
| Fibroepithelial polyp | 9 | 31 | 43 | 47 | 45 | 32 | 17 | 4 | 228 |
| Fibrous epulis | 1 | 15 | 14 | 9 | 7 | 5 | 0 | 0 | 51 |
| Focal hyperplastic gingivitis | 2 | 4 | 6 | 9 | 4 | 2 | 1 | 0 | 28 |
| Gingival | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 3 |
| Hemangioma | 11 | 18 | 12 | 10 | 2 | 9 | 10 | 0 | 72 |
| Lymphangioma | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Mucocele | 24 | 31 | 18 | 8 | 4 | 1 | 2 | 0 | 88 |
| Neuroma | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 3 |
| Others | 0 | 1 | 1 | 2 | 1 | 1 | 0 | 0 | 6 |
| Peripheral giant cell granuloma | 11 | 7 | 7 | 7 | 5 | 5 | 2 | 3 | 47 |
| Pyogenic granuloma | 9 | 33 | 37 | 28 | 15 | 10 | 9 | 7 | 148 |
| Ranula | 5 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 9 |
| Squamous papilloma | 4 | 12 | 11 | 7 | 8 | 3 | 4 | 1 | 50 |
| Total | 82 | 160 | 155 | 138 | 97 | 75 | 58 | 17 | 782 |
| Total | 83 | 171 | 168 | 143 | 99 | 77 | 58 | 19 | 818 |
Site
The oral sites commonly affected by benign neoplasms were the palate, tongue, upper lip and buccal mucosa, in a descending order (Table 3). Detailed site distribution of benign neoplasms is shown in Table 3. The sites commonly affected by non-neoplastic lesions were the gingiva, buccal mucosa, lower lip and tongue in a descending order (Table 3). Detailed site distribution of non-neoplastic lesions is shown in Table 3.
Site Distribution of Benign Oral Soft Tissue Masses
| Lesion | Alveolus | BM | FOM | Gingiva | LL | Palate | Tongue | UL | Uvula | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| NEOPLASMS | ||||||||||
| Angiokeratoma | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Angioleiomyoma | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Granular cell tumor | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 |
| Lipoma | 0 | 3 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 6 |
| Myoepithelioma | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 5 |
| Neurofibroma | 0 | 1 | 0 | 1 | 1 | 0 | 2 | 0 | 0 | 5 |
| Pleomorphic adenoma | 0 | 1 | 0 | 0 | 1 | 8 | 0 | 3 | 0 | 13 |
| Schwanoma | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 0 | 3 |
| Total | 0 | 5 | 0 | 1 | 3 | 14 | 7 | 6 | 0 | 36 |
| NON-NEOPLASMS | ||||||||||
| Abscess | 1 | 3 | 1 | 5 | 2 | 0 | 0 | 0 | 0 | 12 |
| Denture induced granuloma | 23 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 26 | |
| Dermoid cyst | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 3 | 0 | 6 |
| Epidermal cyst | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 4 |
| Fibroepithelial polyp | 2 | 101 | 4 | 11 | 25 | 12 | 63 | 10 | 0 | 228 |
| Fibrous epulis | 0 | 0 | 0 | 51 | 0 | 0 | 0 | 0 | 0 | 51 |
| Gingival cyst | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 3 |
| Hemangioma | 0 | 7 | 1 | 5 | 25 | 0 | 17 | 17 | 0 | 72 |
| Hyperplastic gingivitis | 0 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 28 |
| Lymphangioma | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Mucocele | 3 | 10 | 4 | 0 | 59 | 2 | 10 | 0 | 0 | 88 |
| Neuroma | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 3 |
| Others | 0 | 2 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 6 |
| Peripheral giant cell granuloma | 9 | 0 | 0 | 38 | 0 | 0 | 0 | 0 | 0 | 47 |
| Pyogenic granuloma | 4 | 10 | 0 | 60 | 38 | 5 | 25 | 6 | 0 | 148 |
| Ranula | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 9 |
| Squamous papilloma | 1 | 8 | 0 | 0 | 6 | 14 | 12 | 3 | 6 | 50 |
| Total | 43 | 169 | 21 | 176 | 159 | 36 | 130 | 42 | 6 | 782 |
| TOTAL | 43 | 174 | 21 | 177 | 162 | 50 | 137 | 48 | 6 | 818 |
BM: Buccal Mucosa, FOM: Floor of Mouth, LL: lower Lip, UP: upper Lip.
DISCUSSION
Most previous investigations concentrate on studying a single type of benign oral soft tissue masses or a group of closely related ones. This study investigates all benign oral soft tissue masses in a group of Jordanians. The first English-language published review of benign oral soft tissue masses was by Bloodgood [3]. More comprehensive reviews were subsequently published [4-10]. Most of these studies, like the current study, are derived from surgical pathology reports. Such studies admittedly suffer from referral and case selection biases. Nevertheless, information gleaned from these studies is of value for clinicians facing benign oral soft tissue masses on a daily basis. Furthermore, such studies may constitute a base line for future larger-scale investigations. Population-based nationwide investigations among Jordanians are needed to truly describe benign oral soft tissue masses as they occur naturally in life.
We found that the tissue origins of benign oral soft tissue masses were traumatic, inflammatory/ infective, cystic and developmental in descending order. These findings agree with those from other countries [10-12]. Neoplasms constituted 4% of all benign oral soft tissue masses; this is in general agreement with previous series [6, 10, 11].
Squamous papilloma was a common benign oral soft tissue masses, its peak incidence was in the 11-30 years age group. This contrasts with the general agreement of its peak of occurrence at 40-60 years of age [13]. We found a slight predilection to male gender which is in agreement with a previous series [14]. The most common location for squamous papilloma was the palate and tongue this also in general agreement with a previous series [14].
The pathogenesis of vascular anomalies is a subject of debate. While some authorities consider them developmental malformations, others consider them as hamartomas of blood vessels. In the present series, one of the most common benign oral soft tissue masses was hemangioma; this is in agreement with previous work [15, 16]. We also found that the majority of haemangiomas occurred in children and relatively young adults. This finding supports that haemangiomas are developmental in aetiology.
Nearly one tenth of benign oral soft tissue masses reported in this work are of neural origin. Neural origin benign oral soft tissue masses may arise in both soft and hard tissue of the oral cavity. Those occurring in soft tissue appear as smooth sub-mucosal swellings clinically indistinguishable from other benign oral soft tissue masses. One study investigated such a lesion in oral and perioral soft tissues, it was concluded that they are more frequent than previously reported and should be included in the differential diagnosis of the more frequently encountered benign oral soft tissue masses [17].
Fibroepithelial polyp is believed to be a nonspecific focal hyperplastic reaction of the lamina propria of oral mucosa in response to chronic mechanical stimulation. We found that fibroepithelial polyp was the most common benign oral soft tissue masses. This is in agreement with previous findings [4]. Common sites were the buccal mucosa and tongue which also agrees with published literature [4]. Fibroepithelial polyp was almost twice more common in females than males, a finding in agreement previous studies [18], but contrasts with others [4].
Cystic lesions (notably mucoceles) were among the most common non-neoplastic lesions in this series. This agrees with previous series form other countries [7, 19], but conflicts with some others [18]. Mucoceles are common oral lesions since their tissue of origin i.e. salivary glands is widely distributed throughout the oral cavity. We found that the peak incidence is in the first and second decades with lower lip being the most common site. These findings are in agreement with previous work [4, 5]. Mucoceles were more common among females than males. This agrees with one study [4], but contrasts with another [5].
In our study there was a high degree of occurrence of pyogenic granuloma of the oral cavity in the second, third and fourth decades of life. This age distribution is in accordance with age distribution reported in previous series [20-22]. The predominance of pyogenic granuloma among females reported in this series is also in accordance with previous work [20-22]. We found that the principal oral site affected by pyogenic granuloma was the gingiva. These findings are consistent with those of others [21, 22].
Benign oral soft tissue masses were more frequent among females, this agrees with others [18], but contrasts with some others [8, 19]. This could reflect differences in the genetic pools between different courtiers. Alternatively, it could reflect different degrees of concern and compliance in females toward dental care between different countries. It has been reported after a longitudinal study of oral hygiene [23] that boys have poorer oral hygiene than girls, and that women, especially the educated, were more frequent dental floss users with a better compliance towards dental advice.
Age at presentation is an important clinical parameter when differential diagnosis of a lesion is being formulated. The majority of our patients were in their second, third and fourth decades of life. This differs from findings of others who reported a peak incidence from third to sixth decades [10]. This might reflect the high percentage of young people among the Jordanian population. According to the most recent data of the Department of Statistics of Government of Jordan, approximately 60% of Jordanians are less than 21-years of age.
We found that the oral sites commonly affected by benign neoplasms were the palate, tongue, upper lip and buccal mucosa, in a descending order. This is in general agreement with findings of other investigators [8, 10]. The sites commonly affected by non-neoplastic lesions were the gingiva, buccal mucosa, lower lip and tongue in a descending order. This is in general agreement with findings of some investigators [12] but contrasts with findings of others [4, 8]. These differences are probably related to different methods of categorization of the various benign oral soft tissue masses.
It is concluded that some of our results are in harmony with those of published literature. On the other hand, some of our results are different from published literature. Comparing the overall prevalence rates of the various oral benign oral soft tissue masses between the various published studies is admittedly complicated due to different ways of categorization, and methodology. Further nationwide population-based surveys are needed to further define the epidemiology of benign oral soft tissue masses among Jordanians.


