All published articles of this journal are available on ScienceDirect.
Modified Upper Lip Lift Technique: A Clinical Study to Evaluate Esthetic, Functional, and Scar Quality
Abstract
Introduction
The modified upper lip lift technique has emerged as a promising surgical approach for addressing upper lip elongation and enhancing lip volume, offering improved aesthetic and functional outcomes with minimal scarring. This study aimed to evaluate the efficacy of this technique in increasing lip volume and optimizing upper lip height, tooth exposure, and scar quality.
Materials and Methods
Twenty Arab patients (19 female, 1 male; mean age 32.5 ± 6.4 years) meeting selection criteria for a long upper lip (length ≥ 24 mm for males, ≥ 22 mm for females) underwent a modified upper lip lift. Patients with severe skeletal discrepancies (e.g., severe Class II or III cases, patients with anterior open bite or severe vertical maxillary excess) and excessive exposure of the maxillary anterior teeth gingiva at rest (> 3 mm) were excluded. Upper lip height, vermilion thickness, and anterior tooth exposure were measured preoperatively and at 1 week, 1, 3, and 6 months postoperatively. Scar quality was assessed using the Vancouver Scar Scale (VSS; range 0–13, where 0 = no scar and 13 = worst possible scar).
Results
Statistically significant improvements (p<0.001 for all, paired t-test or Wilcoxon test) were sustained at six months: mean upper lip height decreased from 21.80 ± 1.30 mm to 16.95 ± 0.89 mm, vermilion thickness increased from 2.10 ± 0.79 mm to 5.65 ± 0.75 mm, and tooth exposure improved from 0.25 ± 0.44 mm to 2.00 ± 0.65 mm. Scar quality (VSS) improved significantly (p<0.001, Wilcoxon test), with mean score decreasing from 5.10 ± 0.72 at one week to 2.40 ± 1.05 at three months. No major complications occurred.
Discussion
The modified technique demonstrated significant, stable improvements in lip height, vermilion volume, tooth exposure, and scar quality over six months. The results highlight the precision of the surgical design in balancing aesthetic and functional outcomes. Scar quality benefited from microincisions in natural subnasal creases and reduced-tension closure.
Conclusion
The modified technique effectively enhances lip aesthetics and function, providing stable, long-lasting results with minimal scarring. It represents a reliable alternative to traditional surgical and non-surgical approaches. Future research should prioritize more diverse patient cohorts, include detailed facial skeletal discrepancy assessment, and extended follow-up periods to validate these preliminary findings and establish the technique's long-term efficacy and safety profile.
1. INTRODUCTION
Lips play a pivotal aesthetic and functional role in shaping the overall impression of the face, as they are a key component of the facial “aesthetic triad” alongside the eyes and nose [1, 2]. Aesthetically, harmonious lip appearance is associated with vitality and attractiveness, with full, well-proportioned lips often considered a symbol of youth and freshness across many cultures. Functionally, lips are essential for speech, mastication, and nonverbal communication through facial expressions. However, various factors, such as aging, prior surgical interventions, or congenital deformities, can lead to undesirable changes in lip length, size, or symmetry. These alterations necessitate therapeutic approaches aimed at restoring their natural appearance and enhancing their aesthetic appeal [3-5].
In recent years, the field of lip aesthetics has seen significant advancements, with the development of both surgical and non-surgical techniques to address concerns related to lip length, volume, and positioning. Non-surgical options, such as injectable fillers, offer temporary enhancement with minimal downtime [6, 7]. In contrast, surgical techniques involve incisions and tissue modification to achieve more permanent changes in lip shape [7, 8]. While surgical methods provide long-lasting results, they may also carry risks such as visible scarring or loss of natural lip contours.
Among surgical approaches, the traditional direct lip lift remains a widely used procedure for correcting excessive upper lip length. This technique involves excising a strip of skin just below the nose, thereby elevating the upper lip and increasing visibility of the anterior teeth. Although effective, it can sometimes result in visible scarring or flattening of the vermilion border—particularly if patient selection is not optimal or anatomical considerations are overlooked—potentially compromising the final aesthetic outcome [9, 10].
The primary clinical indication for performing an upper lip lift is the aesthetic and functional deficit caused by a long upper lip, which results in insufficient display of the upper incisor teeth at rest and during animation [11, 12]. An aesthetically pleasing smile typically reveals 2-4 mm of the upper central incisors. A lip that drapes over the teeth, obscuring them completely, can impart an aged, stern, or less vibrant appearance [11, 13]. While the desire for increased vermilion volume is a significant factor, the fundamental goal of the procedure is to reposition the lip to its more youthful and functional position, thereby restoring the normal exposure of the anterior teeth and creating a harmonious balance between the lip, teeth, and overall facial aesthetics. This study's modified technique was specifically designed to address this insufficiency in tooth display while simultaneously enhancing lip volume and minimizing scar visibility [13, 14].
To address the limitations of traditional approaches, we developed and evaluated a modified upper lip lift technique [12-14]. This modification specifically refers to our emphasis on a deep-plane sub-SMAS dissection and suspension of the advanced lip flap to the stable pyriform ligament, rather than relying on a skin-only excision with high-tension closure [11-14]. This approach is designed to minimize visible scarring, prevent nasal base distortion, and ensure long-term stability of the result. It builds upon, but significantly refines, established techniques such as the “bullhorn” lip lift, which involves a central excision of skin beneath the nose, and the “subnasal” or “Italian” lift, which uses two separate lateral excisions. While these traditional methods effectively shorten the lip, they are often associated with a higher risk of an unnatural, “pulled” appearance or visible scarring if tension is not meticulously managed. Our modification aims to enhance both aesthetic and functional outcomes while minimizing these complications [11-14].
This study aims to evaluate the efficacy and safety of a modified upper lip lift technique by comprehensively assessing its impact on key aesthetic and functional parameters, including the reduction of upper lip height, the augmentation of vermilion thickness, and the improvement in upper anterior tooth exposure during smiling, all of which are measured quantitatively at standardized postoperative intervals over a six-month follow-up period to ensure stability of results. Concurrently, the study seeks to objectively document the evolution and final quality of the surgical scar using the Vancouver Scar Scale, thereby providing a rigorous assessment of the technique’s ability to minimize visible scarring through its design and closure method. Furthermore, the research endeavors to monitor and report any associated intraoperative or postoperative complications to establish a robust safety profile, while also contributing to the field by developing and validating a standardized surgical protocol and a set of objective, measurable criteria for outcome evaluation, ultimately facilitating its reliable adoption and comparison in future clinical practice.
2. METHODS
2.1. Study Design and Ethical Considerations
This prospective clinical study was designed to evaluate the outcomes of a modified upper lip lift technique. The study adhered to the ethical principles for human research outlined in the Declaration of Helsinki. Prior to commencement, the study protocol, including the surgical procedure, data collection methods, and informed consent forms, was submitted for review and approval. Formal approval was granted by the Institutional Ethics Committee of Tishreen University, Latakia, Syria (Ethical Permission No. 127 on September 20, 2022).
2.2. Patient Selection and Recruitment
A total of 20 patients were consecutively recruited from the pool of individuals seeking cosmetic improvement at the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tishreen University, and Tishreen University Hospital between January 2023 and June 2024. All patients were thoroughly evaluated during initial consultations. A detailed explanation of the modified surgical technique, its objectives, potential benefits, inherent risks (including scarring, asymmetry, and altered sensation), and the postoperative follow-up schedule was provided to each candidate.
Written informed consent was obtained from all participants who chose to enroll in the study. They were given ample opportunity to ask questions and were informed of their right to withdraw at any time without penalty. The following assessments were made:
• Documentation of Sagittal skeletal relationship (Class I, II, or III malocclusion) based on clinical assessment and cephalometric analysis.
• Documentation of Vertical skeletal pattern, classified as increased, average, or decreased lower anterior facial height (LAFH%) based on clinical facial proportions and cephalometric norms (LAFH >55% = increased, 50–55% = average, <50% = decreased).
2.3. Inclusion and Exclusion Criteria
2.3.1. Inclusion Criteria
• Age ≥ 18 years.
• Long upper lip (length ≥ 24 mm for males, ≥ 22 mm for females).
• Thin upper lip with a marked lack of projection and fullness.
• Absence of systemic diseases that might negatively affect the healing process.
• No previous history of cosmetic surgery in the lip area.
2.3.2. Exclusion Criteria
• Uncontrolled systemic diseases (such as diabetes or autoimmune diseases).
• Smoking more than 10 cigarettes per day.
• Previous allergies to surgical materials.
• Short upper lip (length < 20 mm(.
• Excessive exposure of the maxillary anterior teeth's gingiva at rest (> 34 mm) prior to surgery.
• Patients with severe skeletal discrepancies (e.g., severe Class II or III cases [15], patients with anterior open bite or severe vertical maxillary excess)
2.4. Surgical Procedure
The surgical procedure began with thorough preparation, including cleansing the facial area with an antibacterial solution, sterilizing surgical instruments, and using sterile gloves.
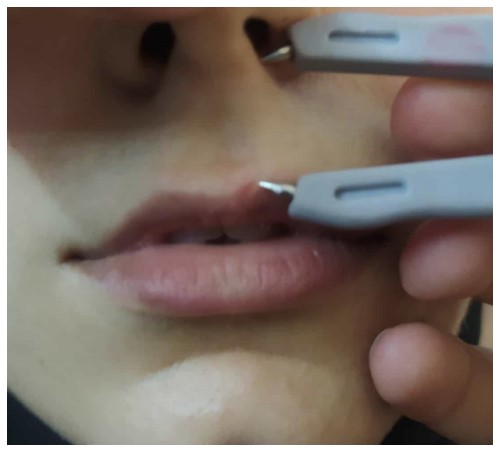
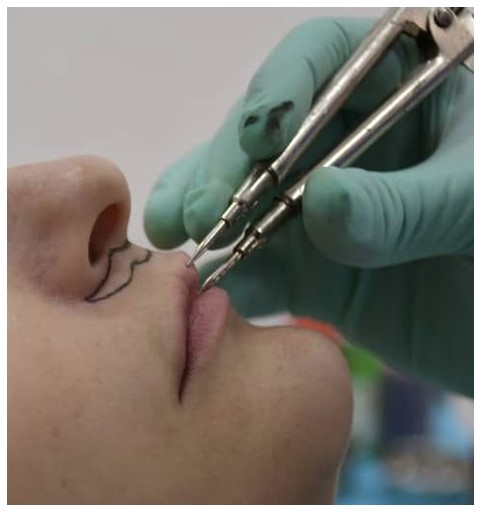
Local anesthesia was administered using a 1:100,000 solution of lidocaine with epinephrine to minimize bleeding and ensure effective numbing (Fig. 1). Once adequate anesthesia was achieved, the surgeon carefully marked the incision line using a sterile surgical pen. A modified bullhorn design was employed, which allows for better distribution of tensile forces and helps conceal the scar within the natural creases beneath the nose (Fig. 2).
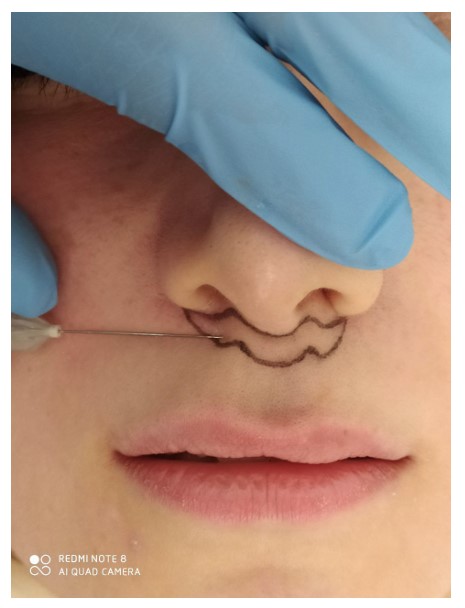
Local anesthesia using a 1:100,000 solution of lidocaine with epinephrine.
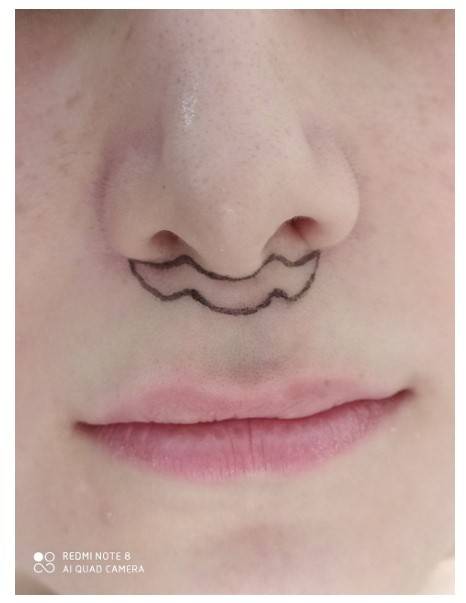
The incision line Marking.
The incision was then made along the pre-drawn line using a No. 15 surgical blade in a single, steady motion, deepened through the full thickness of the skin while avoiding damage to the underlying muscle. The skin flap was carefully elevated using microsurgical scissors and a periosteal elevator, with preservation of the SMAS layer to protect the superficial vascular network supplying the flap. Once the desired depth was reached, the orbicularis oris muscle was gently released from its adhesions, ensuring that its function remained intact and that no excessive tension was placed on the surrounding tissues, which could affect lip mobility. After completion of the incision, the excess skin flap was removed while carefully preserving the integrity of the underlying orbicularis oris muscle—crucial for achieving optimal functional and aesthetic outcomes (Fig. 3).
The outer skin layer was closed using 6/0 nylon sutures using an interrupted suturing technique to ensure precise apposition and minimal scarring (Fig. 4). Particular attention was paid to the mid-arch intersection during suturing, as accuracy in this area is essential for maintaining lip symmetry. At the conclusion of the procedure, a light dressing and antibiotic ointment were applied directly over the incision site.

Making incisions and removing skin.

The closure using the interrupted suturing technique and 6/0 nylon sutures.
Patients received detailed postoperative instructions, including gentle cleansing of the area and avoidance of direct sunlight or extreme heat during the early healing phase. A custom-designed compression bandage was also applied to maintain the lip in an optimal position without compromising blood flow. The bandage was designed to leave most of the lip exposed, allowing continuous monitoring of color and temperature as indicators of proper perfusion.
2.5. Clinical Analysis
The results were evaluated using a combination of objective measures and clinical assessments covering several key variables:
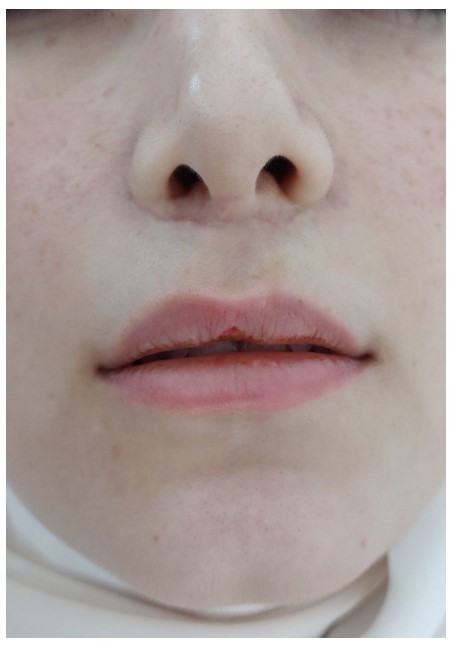
Scar: The Vancouver Scar Scale was used to measure scar grade based on color, texture, height, and elasticity. Results were graded from 0 (excellent scar) to 12 (poor scar) (Figs. 5-7).
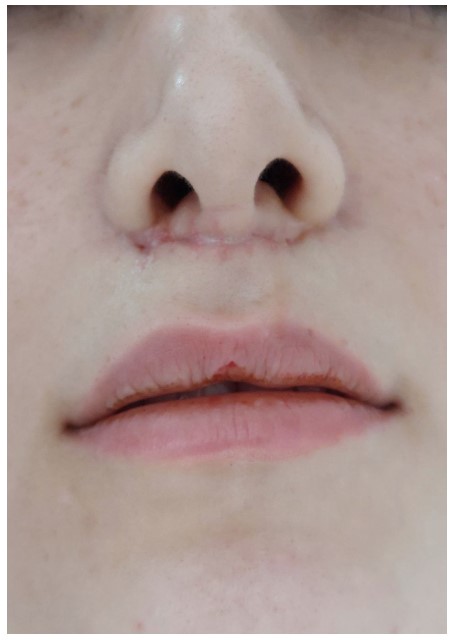
Scar quality assessment after one week.
Scar quality assessment after one month.

Scar quality assessment after three months.
Upper lip height: Upper lip height was estimated by measuring the distance between the inferior vermilion border and the vermilion border at rest using a fine ruler (Fig).
Red lip volume: The vertical distance from the vermilion border to the stomion inferius was measured at rest (Fig).
Upper lip height assessment after one week.
Red lip volume measurement.
Upper anterior tooth exposure: Exposure was estimated during a normal, full smile using a fine ruler graduated in millimeters. The distance between the inferior lip border and the upper tooth margins was recorded (Fig. 10).
Evaluations were performed at specific time points: one week, three months, and six months postoperatively (Fig. 11).

Anterior tooth exposure measurement.

Clinical outcome after six months.
2.6. Statistical Analysis
All data were analyzed using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY). Quantitative data (e.g., age, lip height, vermilion volume) were expressed as means ± standard deviations (SD). Qualitative data (e.g., gender distribution) were expressed as frequencies and percentages.
The normality of the data distribution for continuous variables was confirmed using the Shapiro-Wilk test. To compare the pre-operative measurements with the post-operative measurements at each follow-up interval (one week, one month, three months, six months) for normally distributed data (lip height, vermilion volume, tooth exposure), a paired-samples t-test was used.
For the analysis of scar quality, as assessed by the ordinal Vancouver Scar Scale scores, the non-parametric Wilcoxon signed-rank test was used for pairwise comparisons between different time points. The Friedman test, a non-parametric alternative to the one-way ANOVA for repeated measures, was used to assess the overall change in VSS scores across all four follow-up time points.
A p-value of less than 0.05 was considered statistically significant.
3. RESULTS
3.1. Sample Demographics
The study included a total of 20 patients with a mean age of 32.5 ± 6.4 years. The cohort consisted of 19 females (95%) and 1 male (5%).
Regarding the sagittal and vertical skeletal patterns, which were part of the initial patient assessment, the distribution was as follows: The majority of patients (n=16, 80%) presented with a Class I skeletal relationship. A Class II pattern was observed in 3 patients (15%), and a Class III pattern was found in 1 patient (5%). Vertically, 14 patients (70%) had an average lower anterior facial height (LAFH 50-55%), 5 patients (25%) had an increased LAFH (>55%), and 1 patient (5%) had a decreased LAFH (<50%). All patients, regardless of skeletal pattern, had upper lip lengths that met the inclusion criteria and did not exhibit the severe skeletal discrepancies defined in the exclusion criteria.
3.2. Upper Lip Height
A significant reduction in upper lip height was observed following the modified lip lift procedure. The mean preoperative height was 21.80 ± 1.30 mm. This decreased to 15.65 ± 0.93 mm at one week postoperatively (mean difference: -6.15 mm; 95% CI: -6.71 to -5.59; p<0.001). A slight rebound was noted at the 3-month (16.85 ± 0.93 mm) and 6-month (16.95 ± 0.89 mm) assessments; however, the improvement from baseline remained highly statistically significant (mean difference at 6 months: -4.85 mm; 95% CI: -5.42 to -4.28; p<0.001), demonstrating excellent long-term stability. The changes between all postoperative time points were also statistically significant (p<0.05), as detailed in Tables 1 and 2.
3.3. Vermilion Lip Volume
The procedure resulted in a substantial and stable increase in vermilion volume. The mean preoperative measurement was 2.10 ± 0.79 mm. Postoperatively, volume increased to 5.65 ± 0.75 mm (mean difference: +3.55 mm; 95% CI: 3.16 to 3.94; p<0.001). This result was maintained at the 6-month follow-up, confirming a permanent enhancement without significant regression (p<0.001 for all comparisons to baseline). The data are presented in Table 1, and the statistical analysis is shown in Table 3 (Fig. 10).
3.4. Upper Anterior Teeth Exposure
Tooth exposure during a natural smile improved significantly. The mean exposure increased from 0.25 ± 0.44 mm preoperatively to 2.00 ± 0.65 mm postoperatively (mean difference: +1.75 mm; 95% CI: 1.45 to 2.05; p<0.001). This result remained stable throughout the entire 6-month follow-up period, indicating a durable aesthetic improvement. Statistical results are shown in Table 3.
| Comparison | Mean Difference | p-value | Clinical Interpretation |
|---|---|---|---|
| Pre-op vs. 1 Week Post-op | +6.15 mm | <0.001 | Highly significant |
| Pre-op vs. 3 Months Post-op | +4.95 mm | <0.001 | Maintained significant improvement |
| Pre-op vs. 6 Months Post-op | +4.85 mm | <0.001 | Long-term stability |
| 1 Week vs. 3 Months Post-op | -1.20 mm | 0.012 | Small but significant rebound |
| 1 Week vs. 6 Months Post-op | -1.30 mm | 0.005 | Small but significant rebound |
| 3 Months vs. 6 Months Post-op | -0.10 mm | 0.997 | Complete stabilization |
| Variable | Time Period | Mean | Standard Deviation (±) | Median | Range |
|---|---|---|---|---|---|
| Upper Lip Height | Preoperative | 21.80 | ±1.30 | 22 | 20-24 |
| 1 Week Postop | 15.65 | ±0.93 | 16 | 14-17 | |
| 3 Months Postop | 16.85 | ±0.93 | 17 | 16-19 | |
| 6 Months Postop | 16.95 | ±0.89 | 17 | 16-19 | |
| Red lip volume | Preoperative | 2.10 | ±0.79 | 2 | (1–3) |
| Postoperative | 5.65 | ±0.75 | 6 | (5–7) | |
| Upper anterior tooth exposure | Preoperative | 0.25 | ±0.44 | 0 | (0-1) |
| Postoperative | 2.00 | ±0.65 | 2 | (1-3) |
| Varible | Comparison | t-value | p-value | Statistical Significance |
|---|---|---|---|---|
| Red Lip Volume | Pre-op vs. Post-op | 15.72 | <0.001 | Significant |
| Upper Anterior Teeth Exposure | Pre-op vs. Post-op | -3.92 | <0.001 | Significant |
| - | 1 Week Postop | 1 Month Postop | 3 Months Postop |
|---|---|---|---|
| Pigmentation | 1.65 ± 0.49 | 0.70 ± 0.47 | 0.55 ± 0.51 |
| Vascularity | 1.15 ± 0.37 | 0.60 ± 0.50 | 0.40 ± 0.50 |
| Height | 1.00 ± 0.00 | 0.65 ± 0.49 | 0.45 ± 0.51 |
| Pliability | 1.30 ± 0.47 | 1.00 ± 0.00 | 1.00 ± 0.00 |
| Total | 5.10 ± 0.72 | 2.95 ± 0.83 | 2.4 ± 1.05 |
| Parameter | Z-value / p-value | Mean Difference | Clinical Interpretation |
|---|---|---|---|
| Pigmentation | -3.78 / <0.001 | -1.10 | Highly significant improvement |
| Vascularity | -3.54 / <0.001 | -0.75 | Marked reduction in redness |
| Height | -3.21 / 0.001 | -0.55 | Significant flattening |
| Pliability | -2.45 / 0.014 | -0.30 | Moderate softening of scar tissue |
| Comparison | Z-value | p-value | Mean Difference | Clinical Interpretation |
|---|---|---|---|---|
| 1 Week vs. 1 Month | -3.82 | <0.001 | -2.15 | Rapid early improvement |
| 1 Week vs. 3 Months | -3.92 | <0.001 | -2.70 | Continued significant progression |
| 1 Month vs. 3 Months | -2.71 | 0.007 | -0.55 | Slower but still significant gains |
| Time Point | Excellent (0-3) | Good (4-6) | Fair (7-9) | Poor (10-12) | Clinical Interpretation |
|---|---|---|---|---|---|
| 1 Week | 0% | 100% | 0% | 0% | All scars initially rate as "Good" |
| 1 Month | 15% | 85% | 0% | 0% | Early emergence of "Excellent" results |
| 3 Months | 35% | 65% | 0% | 0% | Progressive improvement to superior outcomes |
3.5. Surgical Scar Quality
Scar quality, assessed by the Vancouver Scar Scale (VSS), showed significant and progressive improvement across all subscales (pigmentation, vascularity, height, pliability) over time (Tables 4-6). The total VSS score decreased from 5.10 ± 0.72 at one week to 2.95 ± 0.83 at one month, and further to 2.40 ± 1.05 at three months (p<0.001 for all pairwise comparisons, Table 5). This clinical improvement is reflected in the categorical distribution of scars: no scars were rated “Excellent” at one week, while 35% achieved an “Excellent” rating (VSS 0-3) by three months, with the remaining 65% rated as “Good” (VSS 4-6) (Table 7).
4. DISCUSSION
Our current study represents an important step in evaluating the effectiveness of the modified upper lip lift technique. Its results demonstrated significant and stable improvements in several key variables, including upper lip height, vermilion volume, anterior tooth exposure, and scar quality. The study recorded an average reduction in upper lip length from 21.8 mm to 15.65 mm postoperatively, a significant increase in vermilion volume from 2.10 mm to 5.65 mm, and an improvement in anterior tooth exposure from 0.25 mm to 2 mm. Scar quality also improved, with a Vancouver Scale score decreasing from 5.10 to 2.40 over three months. These results reflect the precision of the surgical design and its effectiveness in achieving a balance between aesthetic and functional effects. In terms of improving the upper lip height, our results are consistent with those of similar surgical studies that have confirmed the effectiveness of surgical techniques in shortening a long lip. However, our study achieved faster stabilization of results, with no statistically significant changes observed between the third and sixth month measurements. This stability suggests that surgical modifications are more effective in stabilizing tissues compared to traditional techniques, which may exhibit some minor changes in the medium term due to tissue changes or internal tension.
Our modified technique builds upon the foundational “bullhorn” design first described by Cardoso and Sperli and later popularized by others [16, 17]. However, a key distinction lies in our approach to tissue handling and tension management. Traditional techniques often rely on skin excision and direct dermal closure, which can place excessive tension on the suture line, leading to visible scarring, widening, or even nasal base effacement, as critically noted by Talei [18]. Our technique, emphasizing a deep-plane sub-SMAS release, directly addresses this pitfall. By dissecting in a plane above the orbicularis oris and below the SMAS, we achieve a significant release of deep tissue tethers. This allows the advanced lip flap to be suspended under minimal tension to the stable pyriform ligament, a concept supported by anatomical studies [19]. This approach mirrors the principles of modern deep-plane facelift surgery, where release and re-suspension of structural layers yield more natural and durable results than skin-only techniques. Consequently, our high degree of scar satisfaction (VSS improving to 2.40) contrasts favorably with the “unacceptable aesthetic sequelae” and atrophic scarring that Talei associates with high-tension closures and techniques that violate the nasal sill [18].
With regard to increasing the volume of the red lip, our results are superior to those recorded in studies that relied on filler injections, as our technique achieved a more permanent increase without the need for repeated sessions [6, 10]. Furthermore, the absence of absorption of the injected material, as is the case with techniques such as autologous fat injection or silicone gel, makes the results more predictable, reducing the burden on the patient in terms of the number of visits and costs [20].
With regard to the extent of exposure of the anterior teeth, our results showed greater improvement compared to studies that used non-surgical techniques or less precise surgical techniques in determining the cleft location and force distribution. While some studies have reported increases of 1-1.5 mm using filler injections, our technique was able to achieve 2 mm, the desired exposure for most patients, without causing pathological deformities or unnatural changes in appearance [11, 21, 22].
In terms of scar quality, our study demonstrated significant improvement across time periods, with the overall scar score decreasing from 5.10 after one week to 2.40 after three months. This improvement reflects the effectiveness of the surgical modifications in concealing the surgical line within the natural subnasal creases, as well as the use of absorbable sutures to reduce tension on the wound. Compared to traditional techniques, which often score higher on the Vancouver Scale, our technique offers a more effective solution in reducing scarring complications [11, 12, 23, 24].
In addition, the results showed significant stability over the medium term (6 months), supporting the idea that this technique provides a permanent solution compared to non-surgical options that require periodic maintenance. The absence of major complications such as infection or permanent deformities also enhances the safety aspect of the technique, a key factor in determining the appropriate procedure for patients [12-14].
Compared to other studies that used different techniques, such as autologous fat transfer or the use of sutures, our modified technique provided more consistent and stable results, with a significant reduction in the need for subsequent interventions. Furthermore, complete control over lip shape and volume during surgery gives the surgeon greater freedom to design the final outcome compared to techniques that rely on tissue interaction with the injected material [11, 22, 12, 25].
The stability of our results at the 6-month follow-up underscores the durability of this technique. By fixing the advanced soft tissue to the stable pyriform ligament, we mitigate the effects of gravity and tissue relaxation over time, providing a long-lasting solution that non-surgical options cannot match. Furthermore, the modified upper lip lift should not be viewed as an isolated procedure but as an integral component of holistic perioral and midface rejuvenation [17]. As Winslow emphasizes, addressing the aging lip is crucial for a complete lower facial rejuvenation, as rhytidectomy alone does not correct lip elongation, volume loss, or rhytids [26]. Our technique can be effectively combined with other procedures such as facelifts, rhinoplasty, or skin resurfacing (e.g., laser or peels) to address the multifaceted nature of facial aging comprehensively, maximizing patient satisfaction.
While our study focused on the aesthetic and functional improvements of a modified upper lip lift in a cosmetic context, it is crucial to acknowledge that the parameters we measured, specifically, upper maxillary gingival display, are not merely aesthetic concerns but are also critical functional and diagnostic indicators in the field of orthognathic surgery. Excessive maxillary gingival display, often termed a “gummy smile,” is a well-established clinical finding that can signify underlying skeletal discrepancies, such as vertical maxillary excess [27]. However, we excluded these severe skeletal deformities [15] from our study sample as management may require orthognathic surgery. According to the Index of Orthognathic Functional Treatment Need (IOFTN) [28], significant maxillary gingival display is a validated criterion that can indicate a high priority for orthognathic surgical intervention to correct the underlying dentofacial deformity and restore functional harmony. Therefore, while our technique effectively and safely enhances tooth exposure for aesthetic purposes in patients with appropriate indications, it is not a substitute for orthognathic surgery in cases where the underlying etiology is skeletal. Surgeons must exercise careful patient selection to ensure that a lip lift is performed for the correct indications, avoiding its use as a camouflage for a condition that requires definitive skeletal correction. This distinction is vital for achieving optimal long-term functional and aesthetic outcomes for the patient [29].
The most significant limitations of this study are its relatively small, unmatched sample size (n=20) and its short-term follow-up period of six months. The limited cohort restricts the generalizability of our findings to a broader population, as it may not fully capture the range of anatomical variations and potential complications. Furthermore, while the six-month data demonstrates promising stability, it is insufficient to evaluate the truly long-term outcomes of the procedure, as well as the perennial evolution of scar quality, and the potential for late tissue relaxation, considering the fact that upper lip length tends to increase with age [30]. Therefore, a longer observation period, extending to one year or more, would be necessary to conclusively confirm the durability of the surgical modifications [1, 2].
Despite these constraints, our study has notable strengths, including its prospective design and the use of objective, validated measurement tools to quantify outcomes. The multiple, standardized follow-up points provide a robust dataset for analyzing the dynamic healing process within the studied timeframe. Future research should prioritize more diverse patient cohorts, include detailed facial skeletal discrepancy assessment, and extended follow-up periods to validate these preliminary findings and establish the technique's long-term efficacy and safety profile.
CONCLUSION
Based on present findings, using the modified upper lip lift technique, the upper lip height was accurately shortened from an average of 21.8 mm to 15.65 mm postoperatively, with clear stability over the six-month follow-up period. A significant increase in vermilion lip volume was also observed, from 2.10 mm to 5.65 mm, contributing to improved lip fullness and aesthetic appearance. Additionally, the exposure of the upper anterior teeth improved from 0.25 mm to 2.00 mm, which is considered a desirable range from an aesthetic and functional perspective.
In terms of scarring, the results showed a gradual improvement in scar quality, with the Vancouver Scar Scale score decreasing from 5.10 after one week to 2.40 after three months, with no unacceptable scarring or permanent deformity. The microincision design within the natural subnasal creases significantly reduced the scar. Overall, the technique has proven highly effective and safe, with high patient satisfaction, making it a reliable and preferred option compared to traditional techniques or non-surgical procedures in terms of stability and long-term results. However, longer-term follow-ups and a more diverse sample would be recommended for future studies.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contributions to the paper as follows: A.K. and Z.A.: Contributed to study conception and design; Y.N.: was responsible for methodology; G.A.: carried out the investigation; S.E.H.: Performed data collection. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| VSS | = Vancouver Scar Scale |
| IOFTN | = Index of Orthognathic Functional Treatment Need |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Formal approval was granted by the Institutional Ethics Committee of Tishreen University, Latakia, Syria (Ethical Permission No. 127 on September 20, 2022).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patients for publication of this study.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


