All published articles of this journal are available on ScienceDirect.
Complex Odontoma Hampering the Eruption of a Mandibular Second Molar: A Case Report
Abstract
Introduction
Odontoma is the most prevalent odontogenic tumor and can manifest as compound or complex lesions based on its morphologic features, location, and contents. They are incidentally discovered during routine dental examination and are often associated with an impacted tooth.
Case Presentation
Herein, we present a case of a 14-year-old female who reported to the clinic for orthodontic treatment. Intraoral examination revealed an unerupted mandibular right second molar associated with a slight bony expansion in the region. Radiographic examination revealed a heterogeneous, densely radiopaque mass surrounded by a radiolucent capsule coronal to the unerupted tooth, suggestive of an odontoma. The mass was surgically removed, and a diagnosis of complex odontoma was reached after the histopathological findings of haphazardly arranged enamel and dentine. The enamel appeared as empty spaces surrounded by dentine, while the pulp tissue was scattered, presenting as loose connective tissue interspersed with fibrous connective tissue and a band of odontoblastic layer.
Conclusion
Early diagnosis of an odontoma, followed by prompt treatment, will aid in preventing complications in the future.
1. INTRODUCTION
Odontoma (OD) is considered the most common odontogenic tumor, with an incidence rate of 35% to 76% [1-3]. It was first described by Pierre Paul Broca in 1867, with further characterization and discussion by Thoma and Goldman in 1946 [4]. It is often described as a hamartoma of the dental tissue rather than a true neoplasm. Odontomas are incidentally discovered during routine dental examinations, unless symptomatic with evident swelling [5, 6]. The most prevalent location is the anterior maxilla, and the tumor is often associated with an impacted tooth [7]. Although the morphology of an odontoma differs from that of a normal tooth, it still contains the structures of enamel, dentin, and cementum [4]. OD is composed of epithelium and odontogenic ectomesenchyme, often associated with mineralized dental tissues [5].
Panoramic radiography is valuable for the early detection and diagnosis of odontomas; however, cone-beam computed tomography (CBCT) scanning may offer detailed information about the lesion, its relationship with adjacent teeth and structures, and the surrounding bone condition [8]. According to the latest edition of the World Health Organization (WHO) Classification of Head and Neck Tumors, odontomas are divided into two types: compound and complex [9]. The compound odontoma is usually located in the anterior regions of the maxilla. Radiographically, it resembles the tooth structure, consisting of enamel, dentin, and cementum, surrounded by a radiolucent zone. Conversely, complex-type odontomas typically occur in the posterior region and appear as a conglomerate of heterogeneous, radio-opaque masses on the radiograph. From a clinical perspective, an odontoma is categorized into three types: intraosseous (central), extraosseous (peripheral or soft tissue), and erupted [10]. The treatment approaches for odontomas vary from observation to surgical excision, depending on their location, size, and proximity to adjacent structures. Herein, we present an interesting case of a complex odontoma coronally positioned in the lower second molar in a young female patient.
2. CASE REPORT
A 14-year-old female patient who visited the diagnostic clinic at the King Khalid University College of Dentistry (KKUOCD) for a regular check-up expressed a desire to undergo orthodontic treatment for crowded teeth and a narrow upper jaw. Intraoral examination revealed an unerupted mandibular right second molar associated with a slight bony expansion in the region. The maxillary left second premolar was also unerupted. The medical history of the patient was unremarkable.
An orthopantomogram revealed the presence of a radiopaque mass coronal to the unerupted mandibular right second molar (Fig. 1). Subsequently, an intraoral periapical radiograph was taken for a better view of the area. A heterogeneous, densely radiopaque mass surrounded by a radiolucent capsule (size, 10 × 5 mm) was seen on the radiograph, suggestive of a complex odontoma (Fig. 2). The differential diagnoses included a calcifying epithelial odontogenic tumor (CEOT) or an ameloblastic fibro-odontoma.
The patient was referred to the oral surgery unit for surgical removal of the mass. At the next visit, informed consent for the study of the case was obtained from the patient’s guardian, and the patient was admitted to the unit for the surgical removal of the mass. The mass was removed under local anesthesia (mepivacaine 0.020 g/mL; Fig. 3), measured with a caliper, and submitted to the pathology laboratory at the KKUOCD for a confirmed diagnosis. It measured 10 mm in size (Fig. 4) and displayed a mixture of hard and soft tissues with haphazardly arranged dentine histopathologically (Fig. 5A). The enamel was disorganized and appeared as empty spaces surrounded by dentine, while the pulp tissue presented as scattered areas of loose connective tissue interspersed with fibrous connective tissue and a band of odontoblastic layer (Fig. 5B). Based on these findings, the patient was diagnosed with a complex odontoma.
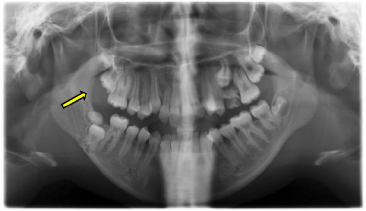
Panoramic radiography illustrating the presence of a radiopaque mass in the right posterior region hampering the eruption of the second molar (yellow arrow).
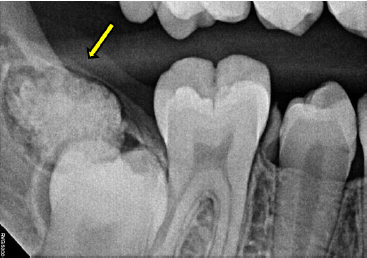
Periapical radiograph showing the heterogeneous, densely radiopaque character of the mass surrounded by a radiolucent capsule (yellow arrow).

Image showing the surgical procedure. The mass was exposed for removal.
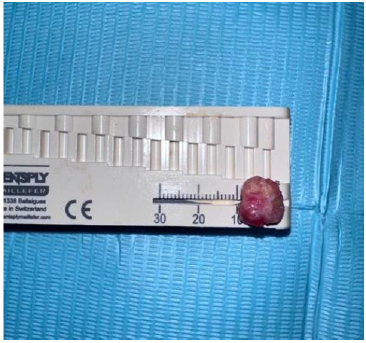
Mass measuring 10 mm after removal.
The patient was recalled for a post-surgical check-up of the site 10 days after the surgery. A periapical radiograph taken to assess the bone and the surrounding tooth revealed complete removal of the lesion (Fig. 6). Another appointment was taken to surgically remove the retained maxillary left deciduous molar, and subsequent orthodontic consultation was planned for teeth alignment.
3. DISCUSSION
Odontoma is the most common odontogenic tumor encountered in the oral cavity [11]. They are generally asymptomatic and are discovered during routine radiographic investigations, which can hinder the eruption of the teeth. However, sometimes, they may cause site-related symptoms, such as mispositioning of teeth, extraoral swelling, infection, localized inflammation, and pain [11]. A recent study in Sharjah reported the case of a female patient who complained of unspecified pain and pressure in the anterior region of the oral cavity [12]. Further examinations revealed a swelling on the labial surface that inhibited the eruption of the canine. Likewise, Ahammed et al. reported the case of a complex odontoma in the maxillary canine region in a 5-year-old who complained of swelling in the region [13]. Odontomas are commonly seen in young adults during the second decade of life [4]. A recent study comprising 4267 white patients reported a mean age of 14 [14]. The sex predilection for odontomas varies across studies [15], with some indicating a slight female predominance [16, 17], others suggesting a male predominance [18, 19], and some reporting no significant gender difference [20, 21].
Although the etiology of an odontoma remains largely unknown, it is thought that odontoblastic hyperactivity [22], interference with mechanisms by which genes control tooth formation, mutations in relevant genes, and the inheritance of those abnormal genes may be involved [23, 24]. Furthermore, aberrant activation of the Wnt/β-catenin signaling pathway and associations with syndromes such as basal cell nevus syndrome, Gardner syndrome, familial colonic adenomatosis, Tangier disease, or Hermann syndrome are also thought to be involved in the etiology of odontoma [11, 25, 26].
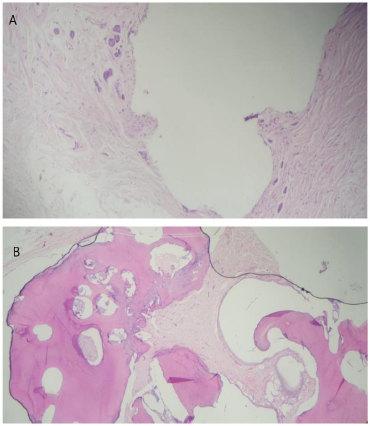
Histopathologic features of the mass. A). A mixture of hard and soft tissues with haphazardly arranged dentine presenting as tubular structures and lacking proper orientations. B). The enamel is presented as disorganized, empty spaces surrounded by dentine. Pulp tissue is observed as scattered areas of loose connective tissue interspersed with fibrous connective tissue and a band of odontoblastic layer.

Periapical radiograph taken during patient recall to investigate the surgical site. We noticed proper bone healing and recovery of the surgical site from radiography.
The compound type is more common than the complex type and is diagnosed earlier, likely due to the maxillary anterior permanent teeth being most commonly affected [11]. Complex odontomas are more frequently seen in the posterior mandibular region [27-29]. The intraosseous type is most frequently encountered, followed by the extraosseous type [30]. The peripheral type is considered the rarest entity, usually presenting as asymptomatic lesions with limited growth [31]. A few rare cases of a large symptomatic eruption odontome have been reported in Saudi patients [32, 33].
In the current case study, the lesion was detected during a routine radiographic examination, with the odontoma measuring 10 mm, which was within the typical range (10–30 mm) reported in the literature [17, 22]. Panoramic radiographs have been successfully used to detect and examine odontomas [17, 18, 34]. Radiographically, odontomas present as a dense, radiopaque lesion surrounded by a thin radiolucent zone; numerous tooth-like structures are generally observed in compound odontomas, whereas complex odontomas present as disorganized masses of calcified tissue [9]. In the present case study, the patient presented with a heterogeneous radiopaque mass surrounded by a radiolucent capsule located coronal to the unerupted mandibular right second molar.
Histopathologically, a compound odontoma presents with demineralized enamel, dentin, cement, and pulp arranged in an organized manner and bounded by a connective tissue capsule [4]. Alternatively, the complex odontoma consists of a haphazard mass of dental tissues and does not resemble a tooth [28]. In the current case study, the lesion presented as a mixture of hard and soft tissues with haphazardly arranged enamel and dentine. The enamel appeared as empty spaces surrounded by dentine, while the pulp tissue was scattered, appearing as loose connective tissue interspersed with fibrous connective tissue and a band of odontoblastic layer. A complex odontoma may appear similar to fibro-osseous lesions, CEOTs, fibrous dysplasia, and chronic osteomyelitis [35]. In the coronal region, it should be differentiated from adenomatoid odontogenic tumors, CEOT, ameloblastic fibro-dentinoma, or odonto-ameloblastoma [11]. A definitive odontoma diagnosis is usually reached after the surgical removal and pathological examination of the mass.
The treatment of odontomas can range from simple monitoring to surgical excision, depending on their location, size, and proximity to adjacent structures. For example, in the case of impacted teeth, treatment may involve surveillance, surgical removal of the odontoma, followed by orthodontic treatment, or surgery followed by monitoring for spontaneous eruption of the tooth [12]. If left untreated, the odontoma may lead to delayed eruption or impaction of the affected tooth. In some cases, the odontoma may erupt into the oral cavity, causing pain, inflammation, and abscess formation [4]. Surgical removal, along with the capsule under local or general anesthesia, is the treatment of choice for this disorder. Blinder et al. [36] recommended a lingual approach for the excision of odontomas in the mandibular angle region to prevent iatrogenic mandibular angle fractures during tooth extraction associated with the odontoma. Furthermore, a two-stage surgical removal of large complex odontomas with a gap of three months in between has been recommended to promote bone consolidation [37].
In the current study, the mass was surgically removed at the oral surgery unit in our hospital, and an appointment was scheduled to remove the retained maxillary left deciduous molar, followed by a subsequent orthodontic consultation for teeth alignment. A similar case of odontoma associated with impaction of the mandibular right permanent canine was recently reported in a 17-year-old Saudi female, wherein the odontoma was surgically removed, followed by orthodontic traction of the permanent tooth [38].
CONCLUSION
This report presents an interesting case of a complex odontoma in a young female that was discovered during a routine examination and successfully treated by surgical removal. These benign tumors, although frequently asymptomatic, can lead to issues such as delayed or impacted teeth, malocclusion, and even cyst formation if left untreated. Surgical removal is the standard treatment, and early intervention can minimize potential problems and enhance treatment outcomes. Thus, prompt diagnosis and management of odontomas are crucial in preventing further complications to permanent teeth.
Despite its clinical relevance, this report has some limitations. The patient follow-up was limited, restricting insights into long-term outcomes. Although the diagnosis was based on clinical, radiographic, and histopathologic findings, the lack of additional confirmatory tests, such as genetic testing, may be a limiting factor. Furthermore, this case report is limited by its lack of novelty, as similar reports have been described in the literature. Nevertheless, it provides useful confirmation of the reported findings and underscores the importance of comprehensive examinations, prompt diagnosis, and effective management of odontomas, thereby contributing to ongoing clinical education.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: N.A.H.: Conceptualization; R.A.A.: Investigation; S.A.A.: Visualization; M.H.: Validation; M.L.: Histopathology diagnosis; H.A.M.: Histopathology processing and diagnosis; H.A.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| OD | = Odontoma |
| CBCT | = Cone beam computed tomography |
| KKUCOD | = King Khalid University College of Dentistry |
| WHO | = World Health Organization |
| CEOT | = Calcifying epithelial odontogenic tumor |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was obtained from the ethics committee of King Khalid University, College of Dentistry, with registration number (IRB/REG/2024-2025/28).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient’s guardian for publication of this case report and any accompanying images.
ACKNOWLEDGEMENTS
Declared none.


