All published articles of this journal are available on ScienceDirect.
Assessing the Mandibular Foramen: A Cone Beam Computed Tomography (CBCT) Study on Location, Morphology, and Clinical Relevance
Abstract
Introduction
The mandibular foramen (MF) is a common anatomical landmark in dentistry that is located slightly posterior to the midpoint of the anterior-posterior dimension of the ramus and at or below the level of the occlusal plane in the dentulous mandible. This study aimed to assess the location, height, shape, diameter, and relationship to the occlusal plane of MF in the adult population using CBCT and compare our findings with those of previous publications.
Methods
In this retrospective cross-sectional study, a total of eight hundred and thirteen CBCT images were collected from the teaching hospital database of Umm Al-Qura University’s Dental Medicine department, with 135 images meeting the inclusion criteria. The participants’ ages ranged from 20 to 76 years.
Results
The mean MF-CLP angle was 41.9° on the left and 42.3° on the right. The median MF height was 2.89 mm on the right and 2.85 mm on the left. The shapes of the observed MFs were predominantly round (52%) and oval (48%). No significant differences in MF height and angle were found between genders.
Discussion
The orthopanogram (OPG) is the most used radiographic imaging technique in dental practice. Despite this, OPGs are not reliable enough to accurately assess the location of the MF.
Conclusion
The observed MF height and MF–CLP angle suggest that inserting the needle at a height of less than 10 mm from the occlusal plane at an acute angle through the contralateral side is recommended for enhancing the success of inferior alveolar nerve blocks.
1. INTRODUCTION
The mandibular foramen (MF) is a common anatomical landmark in dentistry that is located slightly posterior to the midpoint of the anterior-posterior dimension of the ramus and at or below the level of the occlusal plane in the dentulous mandible [1]. The MF represents the path of the inferior alveolar nerve that branches from the posterior division of the mandibular nerve and enters the MF, then runs downward and forward through the inferior alveolar canal and gives off terminal branches of the mental and incisive nerves [2].
Zhou et al. evaluated 121 hemi-mandibular cone-beam computed tomography (CBCT) models to assess the anatomical landmarks of the mandibular ramus. They revealed that 84.3% of MF were below the level of the occlusal plane and 12.4% were above [3]. In children, the MF is located below the occlusal plane and grows in bilateral symmetry postero-superiorly until it reaches the level of the occlusal plane by adolescence [4]. Another study used CBCT to assess MF location by measuring the angle of the contralateral premolar (CLP) contact area to the MF in millimeters. It concluded that MF is located significantly more than 6 mm above the occlusal plane [5]. Additionally, CBCT data from 50 patients at the Kyung Hee University Dental Hospital revealed that MF was oval and located anterior to the center of the ramus in males and the center of the ramus in females [6]. Moreover, Park & Lee concluded that MF position in relation to the occlusal plane was slightly below the occlusal plane in the normal occlusion and skeletal class II malocclusion groups, while in the skeletal class III malocclusion group, MF was above the occlusal plane [7]. A sample consisting of 30 dry human mandibles indicated that the mandibular lingula had a trapezoidal shape, while the MF was oval [8]. The MF location plays a crucial role in the success of inferior alveolar nerve blocks [6], which are widely used in dental practice. During administration, dentists are guided by intra-oral landmarks that can differ from one patient to another [5].
Several studies have noted inferior alveolar nerve block failure when administered as local anesthesia in the mouth, which may be related to the anatomical locations of the mandibular foramen based on individual anatomy [9].
Class III malocclusion is a prevalent maxillofacial deformity [10]. Sagittal split ramus osteotomy has recently become a popular treatment for deformities such as mandibular retrognathism and prognathism. The accurate determination of MF location strengthens the fracture line of the ramus and protects the inferior alveolar nerve [3]. Dental surgical procedures that involve the removal of the ramus and the medial aspect are carried out without vision, thus risking damage to the nerves and blood vessels that supply the mandible [11]. In addition, few studies have analyzed the location of the mandibular foramen using CBCT in this region of Saudi Arabia. Therefore, this study aims to assess the location, height, shape, diameter, and angle in relation to the occlusal plane of the mandible in the adult population using CBCT and compare our findings to previous publications.
2. MATERIALS AND METHODS
2.1. Ethical Considerations
Ethical approval was obtained from the Institutional Review Board at Umm Al-Qura University, Faculty of Dentistry (Approval No. HAPO-02-K-012-2023-11-1864).
2.2. Study Group
In this retrospective cross-sectional study, a total of 813 CBCT images were collected from the Umm Al-Qura University Faculty of Dental Medicine’s teaching hospital database. Data were collected from [15/11/2023] to [13/12/2023] and 135 images meeting the inclusion criteria (65 males and 70 Females). The patients’ ages ranged from 20 to 76 years, with a mean age of 32.92.
Sample size was determined through an online calculator (Epitools) based on 80% power, 5% precision, and a 95% confidence interval [12]. Post-hoc power analysis was performed using G*power software to ensure reliability of the data [13]. Calibration was performed using 12 images that met the inclusion criteria and were subsequently excluded from the study results. An experienced specialist trained the observers on two images; the rest were analyzed by each observer. Good-quality CBCT images with visible anatomical structures were included. Those with malformations, malocclusions, bony lesions, orthodontic appliances, histories of orthognathic surgery or orthodontic treatment, missing teeth, mixed dentitions, and histories of mandibular fractures were excluded.
2.3. Radiographical Analysis
Radiographs were taken using a CBCT scanner (I-CAT 17-19 Imaging Science International LLC., Hatfield, PA, USA). Images were carried out in standard mode, with an exposure time of 26.9 seconds (360°) and a thickness of 1 mm slices. In addition, voxel size ranged from 125-250 µm, and exposure volume was 160 mm x 170 mm. Any significant tilting of the head was corrected on the coronal view before proceeding with measurements. Furthermore, all necessary adjustments were performed to orient the occlusal plane horizontally, ensuring consistency in subsequent measurements. Scans were analyzed using the viewing software ImplaStaion™ v.5.1819.1800. Investigations were carried out in a darkened room using a diagnostic monitor with a resolution of 1920 x 1080. All images were descriptively analyzed and measured by three observers. The radiographic analysis was carried out as follows:
- MF–CLP angle: The coronal view was used to adjust the sagittal plane to the inferior border of MF; then, the axial plane was adjusted to match the level of and come into contact with the mandibular premolars. Afterwards, from the axial view, a straight line was drawn between the contact areas of premolars, and another line from the CLP contact area to the MF was created (Fig. 1).
- MF height: In the sagittal view, the axial plane was adjusted on the buccal cusp tip of the mandibular first premolar and mesiobuccal cusp tip of the mandibular first molar (Fig. 2A), then from the coronal view, a line was drawn from the inferior border of MF to the axial plane (Fig. 2B).
- MF diameter: The axial view was used for measurement (Fig. 3).
2.4. Statistical Analysis
Statistical analyses of all measurements were conducted using SPSS® version 29.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics, the independent sample t-test, the Mann–Whitney U test, and the Pearson correlation test were used to assess the significance of variations in each variable based on age and sex. A significance level of p < 0.05 was utilized as the level of statistical significance. The intra-class correlation coefficient test was used to assess inter-examiner agreement.
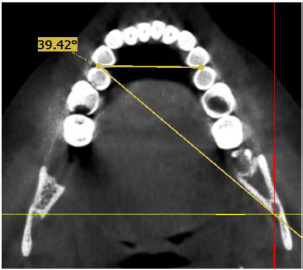
Axial view demonstrating CLP angle.
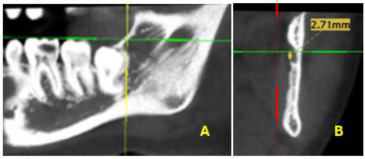
A) Identification of occlusal plane on the sagittal view. B) Measurment of height from occlusal plane to lower border of MF on the coronal view.
3. RESULT
Excellent agreement between observers was found. The mean MF–CLP angle for the left side was 41.9° ± 2.7°, while the same angle was found to be 42.3° ± 3.2° for the right side. The median MF height for the right and left sides was 2.89 with an interquartile range (IQR): 0.25–5.3 and 2.85 with an IQR of 0.68–5.5, respectively (Table 1). The shape of the MF was commonly found to be either round (52%) or oval (48%). A non-significant difference between genders in terms of the MF-CLP angle for the right (p = 0.68) and left sides (p = 0.95) was found. Additionally, no significant difference was found between genders in the MF height for the right (p = 0.25) and left (p = 0.2) sides. While a significant positive correlation between age and the MF–CLP angle on the right side was found (p = 0.015), the correlation on the left side was not statistically significant (p = 0.06). Moreover, a positive, non-significant correlation was found between age and MF height on the right (p = 0.44) and left sides (p = 0.35).
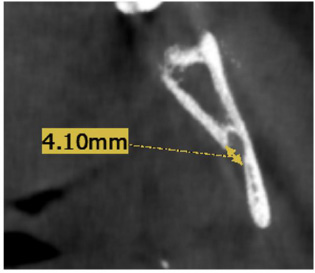
Diameter measurement of MF carried out on the axial view.
4. DISCUSSION
The orthopanogram (OPG) is the most commonly used radiographic imaging technique in dental practice. Despite this, OPGs are not reliable enough to accurately assess the location of the MF [14]. Moreover, inferior alveolar nerve (IAN) block failure rate has been reported to be 20%–25—this was attributed to operator technique, anatomical variations, the psychological status of the patient, the presence of infection, limited mouth opening, loss of teeth, proximity to other accessory nerves and branches, and changes in the patient’s operative posture causing the anatomical key sites to rotate and shift [1, 15, 16].
In this study of 135 CBCT scans, MF was commonly located 2.76 mm above the occlusal plane. This finding aligns with a previous study reporting on the MF’s vertical distance from the occlusal plane [17, 18] and contrasts with results published by Blacher et al., which registered MF height as 9.85 mm [5]. This may be related to variations in patients’ ethnicity and the measuring techniques employed. Moreover, Thangavelu et al. found that the MF was frequently located slightly below the occlusal plane [1]. This study found no significant difference between the genders in relation to MF height.
| Variables | Mean (SD)/ Median(IQR) |
p-value | CI Lower | CI Upper |
|---|---|---|---|---|
| Right MF angle (°) | 42.3 ± 3.2 | 0.68 | 41.83 | 42.91 |
| Left MF angle (°) | 41.9 ± 2.7 | 0.95 | 41.30 | 42.20 |
| Right MF height (mm) | 2.89* (0.25-5.3) |
0.25 | 2.1 | 3.43 |
| Left MF height (mm) | 2.85* (0.68-5.5) |
0.2 | 2.1 | 3.32 |
In contrast, Ahn et al. reported a significant difference in MF height between genders with males having a higher MF than females. This study analyzed data from adults; thus, no significant differences relative to age were found [6].
The MF-CLP angle was registered at 42°, similar to previous studies [5, 17]. However, while wide variations in angle have been reported, this can mainly be attributed to ethnicity [18, 19]. No significant differences in MF-CLP angle were found between genders for both sides, in agreement with the results reported in a study [17].
As to shape, the MF was found to be most commonly round (52%) and oval (48%), which contrasts with a previous publication reporting that oval geometry was more prevalent than round geometry. This discrepancy can be attributed to variations in methodology and sample size [8].
The current study is limited in terms of an insufficient number of CBCT images from adolescents, which hindered a comparison of the mandibular foramen location across different age groups.
Further studies are needed to identify other anatomical factors that affect the location of the MF, such as growth, the rotation of the mandible, and skeletal profiles. Additionally, anatomical variations with clinical implications, such as dental and skeletal abnormalities, should be investigated. Moreover, the use of a convenience sample from a single institution may limit the generalizability of the findings. This study is free from bias, as the sample selection followed strict inclusion criteria, measurements were conducted independently, and reliability was ensured through statistical validation.
CONCLUSION
The study found that variability in the position and morphology of the MF may influence the effectiveness of local anesthetic administration. Considering the observed results for the MF height and the MF–CLP angle in the sample analyzed in this study, inserting the needle at a height of less than 10 mm from the occlusal plane and at an acute angle through the contralateral side is recommended. This approach is expected to increase the likelihood of success for traditional inferior alveolar nerve blocks while also reducing the risk of failure, which can lead to multiple injections and increased patient discomfort. A significant positive correlation between age and the MF–CLP angle on the right side was found, while the correlation on the left side was not statistically significant. Although the difference between the genders was non-significant, further studies are needed to confirm these findings.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: A.O.G.: Study conception and design; O.A., A.H.A., K.A.: Data collection, analysis, drafting of manuscript; S.N.S.: Analysis and interpretation of results; F.H.B.: Methodology; A.K.D.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| MF | = Mandibular Foramen |
| OPG | = Orthopanogram |
| CBCT | = Cone-beam Computed Tomography |
| CLP | = Contralateral Premolar |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Institutional Review Board at Umm Al-Qura University, Faculty of Dentistry, Saudi Arabia (Approval No.HAPO-02-K-012-2023-11-1864).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [A.H.A] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


