All published articles of this journal are available on ScienceDirect.
Prevalence and Patterns of Non-syndromic Hypodontia in Permanent Dentition among the Nepalese Population: A Radiographic Study and Literature Review
Abstract
Introduction
Odontogenesis is a complex process involving interactions between odontogenic and ecto-mesenchymal cells, mediated by growth factors and signaling pathways. Disruptions in these pathways lead to various dental anomalies. This study aimed to evaluate the prevalence and patterns of non-syndromic hypodontia among the Nepalese population.
Methods
A total of 5,075 panoramic radiographs taken between 2012 and 2020 were retrospectively reviewed. The mean age of the study subjects was 20.17 ± 5.51 years (range: 8 to 40 age), comprising 1,805 males (35.56%) and 3,270 females (64.43%). Hypodontia was diagnosed based on the absence of crown calcification of permanent teeth. Prevalence, distribution, and symmetry of hypodontia were assessed, with categorical associations analyzed using the Chi-square test (p<0.05).
Results
The study analyzed 5,075 panoramic radiographs, consisting of 1,805 males (35.56%) and 3,270 females (64.43%). Hypodontia was identified in 400 subjects, 200 males (50%) and 200 females (50%), representing 7.88% of the population. A total of 655 missing teeth were recorded, 45.8% in females and 54.2% in males. Despite an equal number of affected males and females, a statistically significant association was found between gender and overall hypodontia prevalence in the sample (p < 0.05), with males showing a higher likelihood of being affected. Maxillary lateral incisors were the most affected (47.33%), followed by mandibular second premolars (19.08%) and maxillary first premolars (17.56%). The maxillary arch had a significantly higher prevalence of hypodontia than the mandibular arch (p < 0.05). Unilateral hypodontia was more prevalent than bilateral hypodontia (p < 0.05). The most common associated dental anomalies were rotated adjacent teeth and retained deciduous teeth, but they were not statistically significant (p> 0.05).
Conclusion
The prevalence of hypodontia among the Nepalese population was 7.8%. The findings of this study align with global trends, particularly the higher frequency of hypodontia in the maxillary lateral incisors.
1. INTRODUCTION
Odontogenesis, or tooth development, is an intricate process encompassing a series of sequential and reciprocal interactions between odontogenic and ecto-mesenchymal cells derived from the stomadeal epithelium and cranial neural crest cells, respectively [1]. These interactions are intermediated by growth and transcription factors, signal receptors, and numerous soluble morphogens [2]. The developing tooth endures a multitude of morphological, histological, and biochemical transformations to attain physiological and functional maturity [3].
The impediment of typically impeccable phenomena of odontogenesis leads to the emergence of numerous dental anomalies [4]. Tooth agenesis (TA) is one of the prevalent developmental anomalies impacting human dentition. It is defined as the developmental absence of one or more teeth from the ‘normal’ set of human dentition, typically excluding permanent third molars. The number of developmentally absent teeth further classifies TA into three distinct types: hypodontia (absence of 1–5 teeth), oligodontia (absence of more than 6 teeth), and anodontia (agenesis of all teeth) [5].
Hypodontia, also referred to as ‘selective tooth agenesis’ or ‘congenital tooth absence’, predominantly affects permanent dentition rather than deciduous dentition [6]. The lack of a tooth's eruption in the oral cavity, in conjunction with the absence of radiographic evidence supporting its existence within the anticipated period, suggests a diagnosis of hypodontia [7]. This anomaly can manifest itself as a part of a genetic syndrome (like anhidrotic ectodermal dysplasia, Down syndrome, Ehlers-Danlos syndrome, Van der Woude syndrome, etc.) or as an isolated trait of the non-syndromic familial form [5].
Brook's unifying etiological model for anomalies in tooth number and size posits that hypodontia arises from complex interactions among genetic, epigenetic, and environmental influences throughout the process of odontogenesis [8]. Various environmental variables, including radiation, chemotherapeutic agents, and infections, can impede this process. However, the genetic element prevails over the environmental variables in the etiology of hypodontia. Molecular investigations substantiate this assertion by linking it to mutations in genes active during the initial stages of odontogenesis, such as paired box 9 (PAX9), muscle segment homeobox 1 (MSX1), axis inhibitor 2 (AXIN2), and ectodysplasin A (EDA) [9]. Furthermore, epigenetic alterations, such as DNA methylation and histone modification, influence a network of interrelated signaling pathways that encompass odontogenesis, subsequently leading to hypodontia [10].
Non-syndromic hypodontia is reported to be relatively more prevalent than its syndromic counterpart [11]. Khalaf et al. [12] conducted a meta-analysis and estimated the overall prevalence rate of this anomaly to be 6.4%, with a statistically significant difference across various continents. For this anomaly, Africa reported the highest prevalence rate of 13.4%. Europe recorded a prevalence rate of 7%, followed closely by Asia and Australia, both at 6.3%. In contrast, North America exhibited a lower rate of 5.0%, while Latin America and the Caribbean had an even lesser prevalence at 4.4%. Furthermore, this analysis showed that hypodontia was more widespread in females, with a total female: male ratio of 1.22:1. In addition, it was predominantly observed in mandibular second premolars, followed by maxillary lateral incisors and maxillary second premolars. A meta-analysis conducted by Polder et al. [13] further highlighted that unilateral hypodontia is more prevalent than its bilateral counterpart.
The prevalence of hypodontia is known to vary based on factors, such as patients' ethnicity, sampling techniques, diagnostic criteria, chronological age, and sample size [11]. Hence, the present study evaluated the prevalence and pattern of non-syndromic hypodontia of permanent teeth in a subgroup of the Nepalese population. Additionally, a targeted literature review was carried out to compare the prevalence patterns, diagnostic methods, and demographic variations observed in different populations worldwide. Furthermore, this comparative analysis sought to provide a broader understanding of hypodontia trends and their epidemiological significance.
This study aimed to address a critical gap in the existing body of literature, with the anticipation that its findings would provide a robust foundation to inform and guide future research endeavors.
2. MATERIALS AND METHODS
2.1. Study Design
This is a retrospective cross-sectional study that was conducted at the University Hospital of Kathmandu University School of Medical Sciences, Dhulikhel (Kavre, Nepal), utilizing panoramic radiographs. The study adhered to the principles of the Declaration of Helsinki and received approval from the Institutional Review Board (IRB Protocol approval no. 61/19).
2.2. Study Population
This study employed a convenience sampling approach to select panoramic radiographs from the digital archives of the Department of Oral Radiology. Given the retrospective nature of the study, this sampling method was deemed appropriate as it allowed for efficient data collection from a pre-existing institutional dataset spanning eight years (2012–2020). Convenience sampling, while non-random, provided access to a substantial and diverse sample, facilitating a comprehensive evaluation of the prevalence and patterns of hypodontia within the study population.
The selection of radiographs was based on strict inclusion and exclusion criteria to ensure the validity and reliability of the findings. The inclusion criteria comprised panoramic radiographs of individuals aged 8 to 40 years with permanent dentition and no history of systemic syndromes or craniofacial abnormalities. To maintain diagnostic accuracy, only high-quality radiographs free from distortion or artifacts were considered. Conversely, the exclusion criteria encompassed radiographs that exhibited missing teeth due to trauma, extractions, or orthodontic treatment, as these factors could confound the assessment of congenital tooth absence. Additionally, radiographs of individuals diagnosed with syndromic conditions known to affect dental development were excluded to maintain the study’s focus on non-syndromic hypodontia.
Following the application of these criteria, a total of 5,075 panoramic radiographs were included in the study, comprising 1,805 males (35.56%) and 3,270 females (64.43%) aged 8 to 40 (20.17 ± 5.51) years. While convenience sampling does not provide randomization, its application in this study enabled the inclusion of a large dataset over an extended timeframe, thereby reducing potential biases and enhancing the study’s statistical robustness.
Hypodontia was diagnosed by the absence of crown calcification of one or more permanent teeth (excluding third molars) on radiographic examination. The teeth evaluated included all permanent maxillary and mandibular teeth from the central incisors to the second molars (i.e., teeth numbered 11–17, 21–27, 31–37, and 41–47 according to the FDI two-digit system). A diagnosis of hypodontia was established when there was no radiographic evidence of crown calcification for a given tooth and no documented history of its extraction, loss due to trauma, or orthodontic removal.
Two independent observers (SD and DR) meticulously evaluated all panoramic radiographs to ensure diagnostic accuracy, with any discrepancies resolved through mutual consensus. For each confirmed case of hypodontia, comprehensive data were recorded, including demographic details, such as age (in years) and gender (male or female). Dental variables encompassed the presence or absence of permanent teeth (excluding third molars), the location of missing teeth (maxillary vs. mandibular arch), the specific type of missing teeth (e.g., lateral incisors, second premolars, or first premolars), and the pattern of occurrence (unilateral or bilateral). Additionally, associated dental anomalies were documented where applicable.
2.3. Statistical Analysis
The data was collected and processed utilizing SPSS software, version 21 (IBM Corp., Armonk, N.Y., USA). Descriptive and inferential statistics were used to analyze the data, with descriptive statistics specifically applied to summarize the study variables. Prevalence was calculated as a percentage, and patterns were categorized by tooth type, arch (maxillary or mandibular), and symmetry (unilateral or bilateral). Categorical variables association was determined by the Chi-square test with a significance threshold of 0.05.
3. RESULTS
The study analyzed 5,075 panoramic radiographs, comprising 1,805 males (35.56%) and 3,270 females (64.43%). Hypodontia was identified in 400 subjects: 200 males (50%) and 200 females (50%). A total of 655 permanent teeth (excluding third molars) were missing, with 45.8% (300 teeth) in females and 54.2% (355 teeth) in males.
Although the number of males and females with hypodontia was equal, the overall sample had an unequal gender distribution. Therefore, a Chi-square test was carried out to assess the association between gender and the prevalence of hypodontia in the total population. The result was statistically significant (p < 0.05), indicating that males had a significantly higher likelihood of presenting with hypodontia than females when considering the sample’s gender composition (Table 1). No cases of oligodontia or anodontia were observed within the investigated cohort.
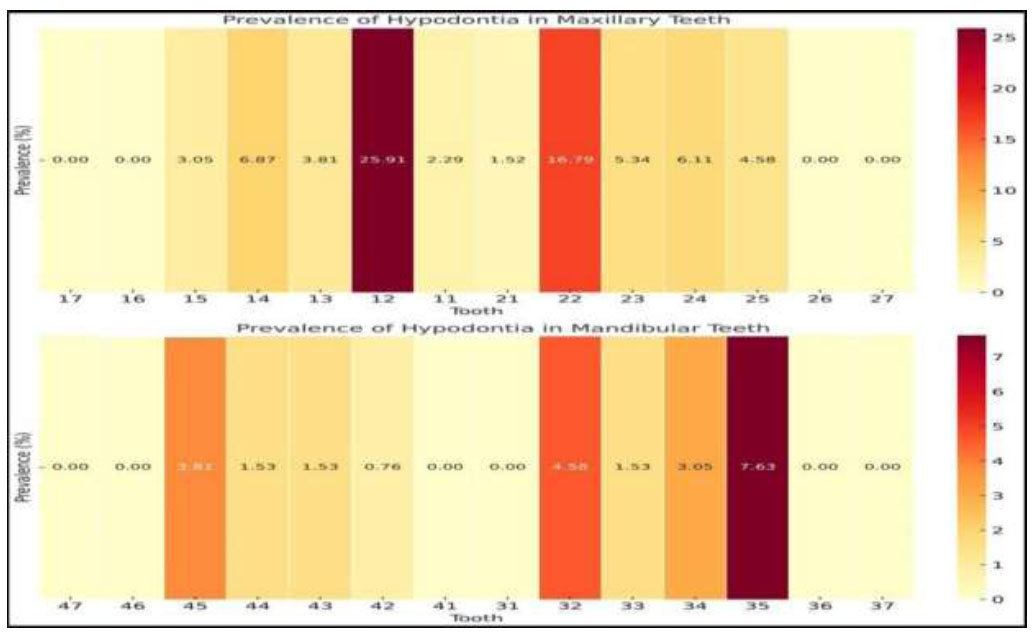
Out of a total of 655 missing permanent teeth, the lateral incisors were the most frequently affected, comprising 47.33% of cases. This was followed by the second premolars (19.08%) and the first premolars (17.56%). Hypodontia was less common in canines (12.21%) and rare in central incisors (3.82%), with no incidences reported for molars (Fig. 1).
| Gender | Female | Male | Total | χ2 Test | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tooth Region | Maxillary | Mandible | Sub-total % |
Maxillary | Mandible | Sub-total % |
- | |||||
| Right Side (%) |
Left Side (%) |
Right Side (%) |
Left Side (%) |
Right Side (%) |
Left Side (%) |
Right Side (%) |
Left Side (%) |
- | ||||
| Central Incisors | 5 (0.76) |
5 (0.76) |
0 (0) |
0 (0) |
10 (1.53) | 10 (1.53) | 5 (0.76) |
0 (0) |
0 (0) |
15 (2.29) |
25 (3.82) |
χ2 = 4.62, df = 1, p = 0.032* |
| Lateral Incisors | 90 (13.74) |
55 (8.39) |
0 (0) |
5 (0.76) | 150 (22.9) |
75 (11.45) |
55 (8.39) |
5 (0.76) |
25 (3.82) |
160 (24.43) |
310 (47.33) |
|
| Canines | 0 (0) |
20 (3.05) |
10 (1.53) |
10 (1.53) |
40 (6.11) |
25 (3.82) |
15 (2.29) |
0 (0) |
0 (0) |
40 (6.11) |
80 (12.21) |
|
| First Premolar | 20 (3.05) |
15 (2.29) |
5 (0.76) | 10 (1.53) |
50 (7.63) |
25 (3.82) |
25 (3.82) |
5 (0.76) |
10 (1.53) |
65 (9.92) |
115 (17.56) |
|
| Second Premolar | 5 (0.76) |
10 (1.53) |
10 (1.53) |
25 (3.82) |
50 (7.63) |
15 (2.29) |
20 (3.05) |
15 (2.29) |
25 (3.82) |
75 (11.45) |
125 (19.08) |
|
| First Molar | 0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
|
| Second Molar | 0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
|
| Total | 120 (18.32) | 105 (16.03) | 25 (3.82) |
50 (7.63) |
300 (45.8) |
150 (22.9) |
120 (18.32) |
25 (3.82) |
60 (9.16) |
355 (54.2) |
655 (100) |
|
Tooth-wise prevalence of hypodontia.
| Tooth Region | Female | Male | Total (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maxilla (%) |
Mandible (%) |
Sub-total % |
Maxilla (%) |
Mandible (%) |
Sub-total (%) |
- | |||||
| Unilateral (%) |
Bilateral (%) |
Unilateral (%) |
Bilateral (%) |
Unilateral (%) |
Bilateral (%) |
Unilateral (%) |
Bilateral (%) |
||||
| Central Incisors | 8 (1.22) |
2 (0.30) |
0 (0) |
0 (0) |
10 (1.53) |
11 (1.68) |
4 (0.61) |
0 (0) |
0 (0) |
15 (2.29) |
25 (3.82) |
| Lateral Incisors | 123 (18.78) |
22 (3.56) |
5 (0.76) |
0 (0) |
150 (22.9) |
88 (13.44) |
42 (6.41) |
28 (4.27) |
2 (0.31) |
160 (24.43) |
310 (47.32) |
| Canines | 18 (2.75) |
2 (0.30) |
18 (2.75) |
2 (0.31) |
40 (6.11) |
38 (5.80) |
2 (0.31) |
0 (0) |
0 (0) |
40 (6.11) |
80 (12.21) |
| First Premolar | 23 (3.51) |
12 (1.83) |
15 (2.29) |
0 (0) |
50 (7.63) |
36 (5.49) |
14 (2.14) |
11 (1.68) |
4 (0.61) |
65 (9.92) |
115 (17.56) |
| Second Premolar | 7 (1.07) |
8 (1.22) |
21 (2.29) |
14 (2.14) |
50 (7.63) |
33 (5.04) |
2 (0.31) |
34 (5.19) |
6 (0.92) |
75 (11.45) |
125 (19.08) |
| First Molar | 0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
| Second Molar | 0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
| Total | 179 (27.33) |
46 (7.02) |
59 (9.01) |
16 (2.44) |
300 (45.8) |
206 (31.45) |
64 (9.77) |
73 (11.14) |
12 (1.83) |
355 (54.19) |
655 (100) |
Furthermore, hypodontia exhibited a significantly higher prevalence in the maxillary arch in contrast to the mandibular arch (p < 0.05). Unilateral hypodontia was significantly more prevalent than bilateral hypodontia in both genders (p < 0.05) (Table 2). Furthermore, the study identified dental anomalies in individuals with hypodontia, such as rotated adjacent teeth and retained deciduous teeth (Fig. 2). However, these observations were not statistically significant.
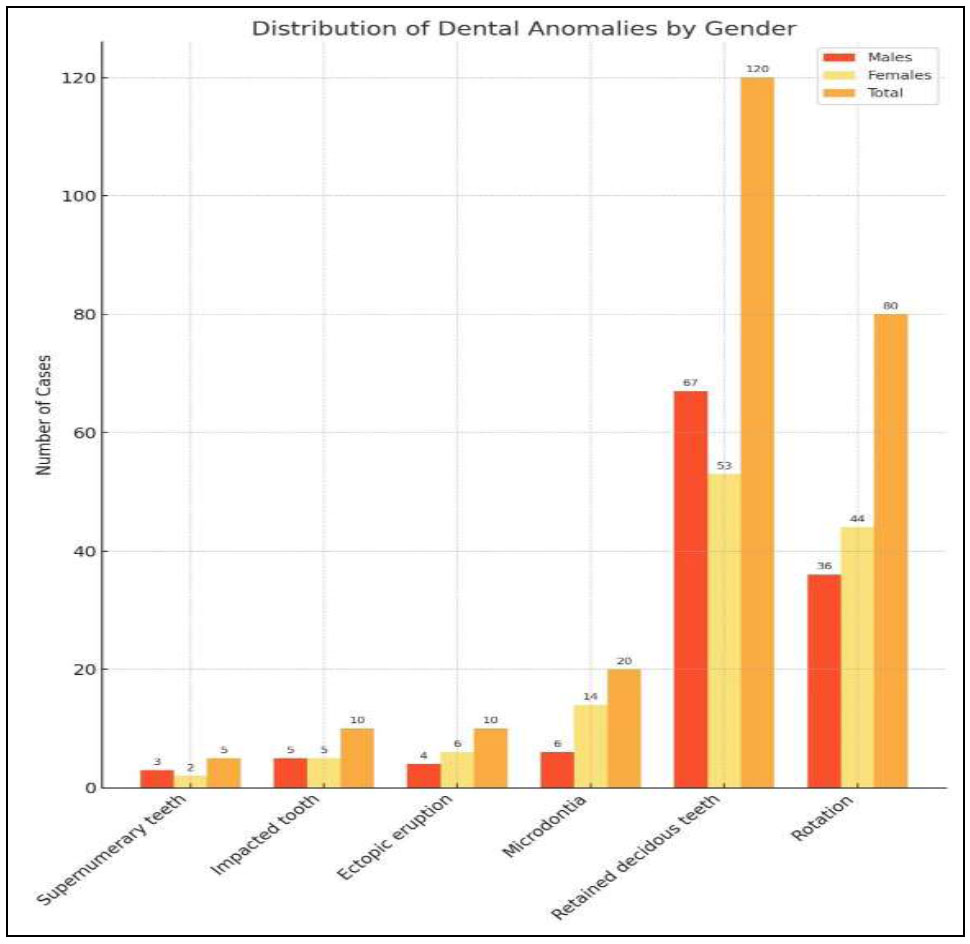
Graph depicting associated anomalies within the subjects with hypodontia.
4. DISCUSSION
Hypodontia, recognized as the most prevalent craniofacial anomaly, affects approximately one-fourth of the global population. Its varied genetic and phenotypic manifestations have consistently driven researchers to conduct extensive epidemiological, analytical, and molecular studies aimed at a deeper understanding of this condition [1]. Although numerous studies have explored the prevalence and patterns of hypodontia, there remains a notable lack of data specific to the Nepalese population. To address this gap, the present investigation was undertaken to determine the prevalence of this anomaly within a defined subgroup of the Nepalese population. As part of this study, a targeted literature review was conducted to synthesize existing research on hypodontia. It was performed using keywords, such as “tooth agenesis,” “hypodontia,” “dental agenesis,” “congenitally missing teeth,” and “dental anomalies” across databases, including PubMed, Google Scholar, and Scopus. Studies were selected based on specific inclusion and exclusion criteria: only prevalence-based studies on hypodontia or tooth agenesis (excluding third molars) with a sample size of 200 or more, published between 2000 and 2024 in English, were considered. Studies focusing on syndromic cases of hypodontia, those with a sample size below 200, non-English publications, case reports, review articles, and studies lacking clear diagnostic criteria were excluded to ensure methodological consistency and comparability.
Studies were further categorized based on the methodology used for hypodontia diagnosis, including radiographic assessments (panoramic or intraoral radiographs), clinical examinations, and journal-reported findings. Additionally, the type of study design (cross-sectional, retrospective, or prospective) was documented to assess the reliability of the findings. The reviewed literature was critically analyzed to compare prevalence rates, gender distribution patterns, and tooth-type involvement across different populations. The insights gained from this literature contribute to a broader understanding of hypodontia trends and provide a comparative framework for evaluating the Nepalese cohort.
A summary of the literature review illustrating the prevalence pattern among different demographics is presented in Table 3 [14-89].
|
Reference Study |
Publication Year | Country | Study Type | Evaluation Method |
Age Range (Years) |
Total Sample Size | Hypodontia % | Distribution between the Genders % | Most Frequently Reported Hypodontia | |
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||
| Present Study | 2024 | Nepal | Cross-sectional (Retrospective) |
Radiographs (panoramic) |
8-40 | 5075 | 7.8 | 3.9 | 3.9 | 12>22>35>14> 24>23>25,32> 13,45>15,34> 11>43,44,21, 33>42 |
| Cavare A et al. [14] | 2024 | France | Retrospective | Radiographs (panoramic) |
9-21 | 4569 | 7.9 | 3.13 | 4.16 | 35>45>12>22>45>12>22>42>15>25>41 |
| Katanaki et al. [15] | 2024 | Greece | Retrospective | Radiographs (panoramic) |
9-16 | 621 | 5.3 | 2.41 | 2.89 | 35,45>12,22,31,41>33,43>15,25> 37,47 |
| Meistere et al. [16] | 2024 | Latvia | Cross-sectional | Radiographs (panoramic) |
11-14 | 2692 | 9.3 | 3.6 | 5.9 | 35,45>12,22>15,25 |
| Kanchanasevee et al. [17] | 2023 | Thailand | Cross-sectional (retrospective) |
Radiographs (panoramic) |
15.96 ±0.83 | 1090 | 9.3 | 3.39 | 5.87 | 45,35>42,32>22,12 |
| Schonberger et al. [18] | 2023 | Israel | Cross-sectional (retrospective) |
Clinical examination, intraoral photographs, dental models, and radiographs (panoramic) |
10–25 | 3000 | 10.86 | 4.63 | 6.23 | 12,22>35,45>15,25 |
| Vinjolli et al. [19] | 2023 | Albania | Cross-sectional (retrospective) |
Radiographs (panoramic) |
15.1±5.5 | 779 | 24.39 | 9.62 | 14.76 | 12>22>35>4515>25 |
| Gupta et al. [20] | 2022 | Nepal | Retrospective | Radiographs (panoramic) |
16.42 ± 3.428 | 601 | 7.48 | Not Specified | 12,22>32,42>31,41>35,45>15,25 | |
| Eshgian N. et al. [21] |
2021 | America | Retrospective | Radiographs (panoramic) |
Not Specified | 1101 | 2.08 | 0.72 | 1.36 | 14,15,24,25> 12,22,32,42> 34,35,44,45 |
| Yagnam, K et al. [22] | 2020 | Chile | Cross-sectional | Radiographs (panoramic) |
Not Specified | 9207 | 3.02 | 1.12 | 1.9 | 35,45>12,22 |
| Kumar D et al. [23] | 2020 | India | Cross-sectional | Radiographs (panoramic) |
12-28 | 1100 | 11.6 | 5.8 | 5.8 | 12,22>31,41>35,45 |
| Fahim And Elabbasy [24] |
2020 | Egypt | Cross-sectional (retrospective) |
Radiographs (panoramic) |
14-25 | 435 | 10.1 | 7.6 | 2.5 | 12,22>35,45>15,25 |
| Pallikaraki G et al. [25] |
2020 | Greece | Cross-sectional (retrospective) |
Radiographs (panoramic) |
7-17 | 1200 | 6.6 | 2.8 | 3.8 | 34,44>15,25,14,24>35,45 |
| Bandaru BK et al. [26] | 2019 | India | Cross-sectional | Clinical examination | 3-15 | 5000 | 0.8 | 0.6 | 0.2 | 12,22 |
| Aragón HN et al. [27] |
2019 | Argentina | Cross-sectional (retrospective) |
Radiographs (panoramic) |
7-11 | 223 | 4.48 | 2.24 | 2.24 | 35,45>12,22,15,25 >31,41 |
| Haghanifar S., et al. [28] |
2019 | Iran | Cross-sectional (retrospective) |
Radiographs (panoramic) |
Not Specified | 8018 | 1.67 | 0.54 | 1.13 | 12,22>15,25 |
| Chandak R et al. [29] |
2019 | India | Cross-sectional (retrospective) |
Radiographs (panoramic) |
12-36 | 1000 | 1.9 | 0.9 | 1 | Not specified |
| Gurbuz O. [30] |
2019 | Turkey | Cross-sectional | Clinical and Radiographical (panoramic) examination |
12-93 | 2203 | 3.4 | 1.27 | 2.13 | Not specified |
| Aldhorae KA [31] |
2019 | Yemen | Cross-sectional (retrospective) |
Radiographs (panoramic) |
9-52 | 1202 | 7.48 | 3.24 | 4.24 | 12,22 |
| Fernandez CCA et al. [32] |
2018 | Brazil | Cross-sectional (retrospective) |
Pre-orthodontic records | > 8 | 1047 | 7.44 | 2.67 | 4.77 | 24>22>21 |
| Baron C et al. [33] |
2018 | France | Cross-sectional (retrospective) |
Intraoral photographs and radiographs (panoramic) |
15.23 | 551 | 5.2 | 1.4 | 3.8 | 35,45>15,25>12,22 |
| Hekmatfar S et al. [34] | 2018 | Iran | Cross-sectional (retrospective) |
Radiographs (panoramic) |
Not specified | 1800 | 3.72 | 2.05 | 1.67 | 35,45>12,22 |
| Anitha et al. [35] |
2018 | India | Cross-sectional | Clinical examination | 10-70 | 7018 | 0.28 | Not specified | ||
| Roslan AA et al. [36] | 2018 | Malaysia | Cross-sectional (retrospective) |
Dental models, and radiographs (panoramic) |
Not specified | 370 | 7 | Not specified | 32,42>35,45 | |
| Chandrika V. et al. [37] | 2018 | India | Cross-sectional (retrospective) |
Dental models, and radiographs (panoramic) |
12-30 | 600 | 3 | 0.33 | 2.67 | 12,22>15,25>35,45 |
| Sola A. et al. [38] | 2018 | Spain | Cross-sectional (retrospective) |
Radiographs (panoramic) |
7-11 | 2500 | 3.48 | 1.8 | 1.6 | 35, 45 > 12, 22 |
| Zakaria H et al. [39] | 2018 | UAE | Cross-sectional (retrospective) |
Radiographs (panoramic) |
Not specified | 2925 | 1.26 | 0.65 | 0.61 | Not specified |
| Ifesanya J.U et al. [40] | 2018 | Nigeria | Cross-sectional (retrospective) |
Radiographs (panoramic) |
10-46 | 216 | 10.2 | Not specified | 35,45>12,22>14,15 >32,42 |
|
| Goutham B et al. [41] | 2017 | India | Cross-sectional (retrospective) |
Radiographs (panoramic) |
18-62 | 1080 | 4.07 | 2.22 | 1.85 | Not specified |
| Almaz M.E. et al. [42] |
2017 | Turkey | Cross-sectional | Clinical and radiographical (panoramic) examination |
1-15 | 9173 | 0.52 | 0.21 | 0.31 | 35,45 |
| Laganà G. et al. [43] |
2017 | Italy | Cross-sectional (retrospective) |
Radiographs (panoramic) |
8-12 | 4706 | 6.69 | 3.35 | 3.34 | 45 |
| Gracco ALT. et al. [44] |
2017 | Italy | Cross-sectional (retrospective) |
Radiographs (panoramic) |
9 - 16 | 4006 | 9 | 4.2 | 5.1 | 35,45 > 12, 22> 15,25 > 14,24 |
| Badrov J. et al. [45] |
2017 | Croatia | Cross-sectional (retrospective) |
Pre-orthodontic records | 6-15 | 4430 | 7.8 | 3.4 | 4.4 | 34,45>12,22>15,25 |
| Al-Sheraydah NA et al. [46] |
2017 | Iraq | Cross-sectional | Clinical examination | 15 | 1000 | 4.6 | 1.3 | 3.3 | Not specified |
| Abdulkareem GB. [47] |
2016 | Sudan | Cross-sectional (retrospective) |
Radiographs (panoramic) |
18-45 | 1225 | 8 | 1.55 | 6.45 | 35,45>15,25>12,22 >32,42 |
| Kumar A [48] | 2016 | India | Cross-sectional | Clinical and radiographical (panoramic) examination |
14-60 | 1500 | 12.8 | 6.6 | 6.2 | Not specified |
| Saberi EA et al. [49] | 2016 | Iran | Cross-sectional (retrospective) |
Radiographs (panoramic) |
Not specified | 1172 | 1.1 | 0.59 | 0.51 | 12,22>35,45>32,42 |
| Dang HQ et al. [50] | 2016 | Australia | Cross-sectional (prospective) |
Radiographs (panoramic) |
6-18 | 1050 | 4.28 | 2 | 2.28 | 35,45>12,22>15,25 >37,47>32,42>34,44 |
| Hashim HA et al. [51] |
2016 | Qatar | Cross-sectional (retrospective) |
Pre-orthodontic records | 11-36 | 1000 | 7.8 | 2.4 | 5.4 | 12,22>34,45>15,25 >32,42 |
| Yassin SM [52] |
2016 | Saudi Arabia | Cross-sectional (retrospective) |
Clinical and Radiographical (panoramic) examination |
Not specified | 1252 | 9.66 | 4.23 | 5.43 | 35,45>12,22 |
| Yamunadevi A et al. [53] |
2015 | India | Cross-sectional | Clinical examination | 17-21 | 244 | 2 | 0 | 2 | 12,22 |
| Abu-Hussein M et al. [54] |
2015 | Israel | Cross-sectional (retrospective) |
Radiographs (panoramic; intraoral periapical) |
12-39 | 2200 | 2.59 | 1.09 | 1.50 | 35,45>12,22>15,25 >31,41 |
| Vani N.V. et al. [55] | 2015 | Saudi Arabia | Cross-sectional (retrospective) |
Radiographs (panoramic) |
18-40 | 1000 | 5.2 | 2.2 | 3 | 12,22>35,45,34,44 >14,24,15,25 |
| Tantanaporn KW. [56] |
2015 | Thailand | Cross-sectional (prospective) |
Clinical and radiographical (Panoramic) examination |
13-30 | 638 | 13.16 | 2.82 | 10.34 | 31,32,41,42>34,35,44,45>11,12,21,22 |
| Shokri A. et al. [57] | 2014 | Iran | Cross-sectional | Radiographs (panoramic) |
7-35 | 1649 | 5.7 | Not specified | 12,22>35,45>15,25 | |
| Bozga A et al. [58] |
2014 | Romania | Cross-sectional | Pre-orthodontic records | 6-41 | 518 | 6.7 | 3.3 | 3.4 | 35,45 >12,22 >15,25 > 31,41 > 37,47 >32,42 |
| Gonçalves-FIlho AS et al. [59] | 2014 | Brazil | Cross-sectional | Dental records | 2-30 | 487 | 6.16 | 2.26 | 3.9 | Not specified |
| Herrera Atoche JR et al. [60] | 2014 | Mexico | Retrospective | Pre-orthodontic records | 9-20 | 690 | 5.82 | 2.09 | 3.73 | 35,45 |
| Karadas M et al. [61] | 2014 | Turkey | Retrospective | Radiographs (panoramic) |
8- 16 | 2722 | 3.89 | 1.51 | 2.38 | 12,22>35,45>31,41,15,25 |
| Mani SA et al. [62] | 2014 | Malaysia | Retrospective | Radiographs (panoramic) |
12-16 | 834 | 7.3 | 3.4 | 3.9 | 12,22 >15,25,35,45 >13,23 |
| Al-Amiri A et al. [63] | 2013 | America | Cross-sectional (retrospective) |
Pre-orthodontic records | Not specified | 496 | 9.5 | Not specified | 35,45>12,22>15,25 | |
| Cunha MGM et al. [64] |
2013 | Brazil | Cross-sectional (retrospective) |
Radiographs (panoramic) |
4-12 | 523 | 8.9 | 2.1 | 6.8 | Anodontia |
| Diab H. [65] |
2013 | Saudi Arabia | Cross-sectional (retrospective) |
Radiographs (panoramic) |
25.3-26.8 | 350 | 15.4 | 7.14 | 8.28 | 12,22,32,42>15,25,35,45> |
| Trakinienė G. et al. [66] |
2013 | Lithuania | Retrospective | Pre-orthodontic records | 10-39 | 824 | 17.11 | 4.85 | 12.26 | 35,45 |
| Campoy MD et al. [67] |
2013 | Portugal | Retrospective | Dental records | 7-21 | 2888 | 6.1 | Not specified | ||
| Rathi MK et al. [68] | 2013 | Pakistan | Retrospective | Radiographs (panoramic) |
Not specified | 570 | 6.8 | 3.3 | 3.5 | 35,45 |
| Afify AR. et al. [69] |
2012 | Saudi Arabia | Cross-sectional (retrospective) |
Dental records | 12-30 | 878 | 4.66 | 2.39 | 2.27 | 34,35,44,45>13,23 |
| Sogra Y et al. [70] |
2012 | Iran | Retrospective | Radiographs (panoramic) |
Not specified | 1590 | 10 | 1.26 | 8.74 | 12,22>35,45 |
| Asec Coelho et al. [71] |
2012 | Portugal | Retrospective | Radiographs (panoramic) |
6-15 | 1438 | 8 | 3.9 | 4.1 | 35,45> 12, 22 > 15,25 |
| Medina AC [72] |
2012 | Venezuela | Cross-sectional | Dental records | 5-11 | 607 | 4.1 | 1.5 | 2.6 | 12,22 > 35,45 > 15,25 >32,42 > 37,47 |
| Fnaish M M [73] | 2011 | Jordan | Prospective | Clinical and radiographic examinations | 5-12 | 3600 | 8.8 | 3.4 | 5.4 | 35,45>15,25>12,22 |
| Gupta SK et al. [74] | 2011 | India | Cross-sectional | Clinical examination, dental models, and radiographs |
Not specified | 1123 | 4.54 | 2.31 | 2.23 | 12,22>31,41>11,21,14,15,25,24 |
| Kazanci F et al. [75] | 2011 | Turkey | Cross-sectional | Clinical examination, dental models, and radiographs |
9-25 | 3165 | 4.5 | 1.3 | 3.2 | 12,22>35,45>31,41 >15,25 |
| Behr M. et al. [76] |
2011 | Germany | Retrospective | Dental records | 5-44 | 1353 | 12.6 | 6.3 | 6.3 | 35>45>22>12>15>25 |
| Kim YH [77] |
2011 | Korea | Retrospective | Clinical examination, dental models, and radiographs |
9-30 | 3055 | 11.3 | 3.7 | 7.6 | 35,45>32,42>15,25 |
| Aktan AM et al. [78] |
2010 | Turkey | Retrospective | Radiographs (panoramic) |
5 – 37 | 100,577 | 1.47 | 0.62 | 0.85 | 35,45>12,22 |
| Vahid-Dastjerdi E et al. [79] | 2010 | Iran | Retrospective | Dental models, and radiographs (panoramic, intraoral periapical) |
9-27 | 1751 | 9.1 | 4.2 | 4.9 | 12,22>15,25>32,42> 35,45 |
| Celikoglu M et al. [80] |
2010 | Turkey | Retrospective | Radiographs (panoramic) |
10 - 25 | 3341 | 4.6 | 1.5 | 3.1 | 12,22>35,45>31,41 |
| Hashem AA et al. [81] |
2010 | Ireland | Retrospective | Clinical examination and radiographs (panoramic) |
7-50 | 168 | 11.3 | Not specified | 35,45>15,25>12,22 | |
| Gomes RR [82] |
2010 | Brazil | Retrospective | Pre-orthodontic records | 10-15.7 | 1049 | 6.3 | 2.5 | 3.8 | 12,22 |
| CJ Chung et al. [83] | 2008 | Korea | Retrospective | Dental models, and radiographs (panoramic) |
Not Specified | 1622 | 11.2 | 5.5 | 5.7 | 32,42>35,45 |
| Goya, H. A. et al. [84] | 2008 | Japan | Retrospective | Radiographs (panoramic) |
3-17 | 2072 | 8.4 | 4.1 | 4.3 | 35,45 > 12, 22> 15,25 |
| Endo et al. [85] |
2006 | Japan | Retrospective | Radiographs (panoramic) |
5 -15 | 3358 | 8.5 | 3.2 | 5.3 | 35,45> 12, 22, 32, 42 > 15, 25 |
| Gábris K et al. [86] |
2006 | Hungary | Retrospective | Radiographs (panoramic) |
6-18 | 2219 | 14.69 | Not specified | 12,22>35,45>15,25 >31,41 |
|
| Silva Meza R. [87] |
2003 | Mexico | Retrospective | Radiographs (panoramic) |
9-20 | 668 | 2.7 | Not specified | 12, 22>35,45 | |
| Ng'ang'a RN and Ng'ang'a PM [88] |
2001 | Kenya | Retrospective | Radiographs (panoramic) |
8-15 | 615 | 6.3 | 3.9 | 2.4 | 35,45>15,25>12,22 |
| Backman B. and Wahlin Y.B. [89] |
2001 | Switzerland | Cross-sectional | Clinical examination and radiographs (bitewing, intraoral periapical, extraoral) |
7 | 739 | 7.4 | 3.2 | 4.2 | 35,45 > 15,25 |
The prevalence of hypodontia observed in this study was 7.8%, a finding consistent with investigations from France (7.9%), Yemen (7.48%), Brazil (7.44%), Croatia (7.8%), Qatar (7.8%), Malaysia (7.3%), and Switzerland (7.4%) [14, 31, 32, 45, 51, 62, 89]. This notable uniformity across various geographic regions highlights the probable influence of shared genetic predispositions and environmental factors, such as familial history, dietary influences, and exposure to environmental teratogens, contributing to the manifestation of this condition. Nevertheless, the prevalence rate observed in the present study surpasses the estimates reported in the meta-analysis by Khalaf et al. [12], which determined the global prevalence of this anomaly to be 6.4% and the Asian prevalence to be 6.3%. The literature reviewed in the present study further underscores notable variability in the prevalence of this abnormality, with reported frequencies ranging from 0.28% in the Indian population to 17.11% in the Albanian population [19, 35]. This variation in prevalence rates can be attributed to several factors, including patients' ethnicity, sampling techniques, diagnostic criteria, chronological age, and sample size, as highlighted by Shimizu T and Maeda T [11]. The disparity in methodologies and sample sizes influencing the prevalence rate of hypodontia is exemplified by five distinct Iranian studies, where prevalence rates span from 1.1% to 10% [28, 34, 49, 57, 70, 79].
The present study identified a notable variation in the distribution of hypodontia between males and females across different tooth types. This finding challenges prior research that suggested an equivalent predisposition to hypodontia among genders. Studies by Kumar D et al. [23], Hugo Norberto Aragón et al. [27], and Behr et al. [76] reported no significant gender differences in hypodontia prevalence within populations from India, Argentina, and Germany, respectively. Similarly, investigations conducted in the UAE [39], Romania [58], and Pakistan [68] found no statistical association between gender and hypodontia occurrence. However, a meta-analysis by Polder et al. [13] indicated a higher prevalence of hypodontia among females, who were approximately 1.4 times more likely to exhibit the condition than males. Additional studies from France [14], Turkey [30], Brazil [32], Sudan [47], Qatar [51], Thailand [56], Lithuania [66], Iran [70], and Korea [77] have also highlighted gender-based variability in hypodontia prevalence.
The findings of the present study revealed a markedly higher prevalence of hypodontia in the maxillary arch (75.57%) compared to the mandibular arch (24.43%). This observation corroborates the conclusions drawn by Khalaf et al. [12] in their comprehensive meta-analysis, which similarly reported a greater propensity for hypodontia in the maxilla relative to the mandible. In contrast, investigations conducted within French [14], Thai [17], and Latvian [16] populations have demonstrated a higher prevalence of hypodontia in the mandibular arch.
Our investigation identified the maxillary lateral incisors as the most frequently affected teeth in cases of hypodontia. This finding aligns with previous studies conducted on populations from Egypt [24], Iran [28, 49, 57, 70, 79], Yemen [31], Qatar [51], Saudi Arabia [55, 65], Turkey [75, 61, 80], and Malaysia [62]. However, meta-analyses by Khalaf et al. [12] and Polder et al. [13] reported the mandibular second premolar as the most commonly affected tooth globally. Furthermore, in the present study, hypodontia involving mandibular incisors was notably rare or absent, contrasting with their higher prevalence in Chinese and Japanese populations as reported in prior literature [90, 91].
In the present study, hypodontia predominantly manifested in its mild form, with either one (60%) or two (30%) missing teeth. This finding aligns with meta-analyses by Khalaf et al. [12] and Polder et al. [13], which estimated the prevalence of mild forms of hypodontia to be the highest, accounting for 81.6% and 83% of total cases, respectively. Moreover, this trend is consistent with observations reported in studies by Goya et al. [84] and Endo et al. [85], further corroborating the predominance of mild form of hypodontia across diverse populations.
Consistent with the meta-analyses conducted by Polder et al. [13], the present study demonstrated a higher prevalence of unilateral hypodontia compared to its bilateral counterpart. However, this finding contrasts with studies conducted on Italian [44], Japanese [85, 85], and Mexican [87] populations, where bilateral hypodontia was either more prevalent or exhibited an equal prevalence to unilateral hypodontia. In the present study, bilateral hypodontia was predominantly observed in the maxillary lateral incisors, maxillary first premolars, and mandibular second premolars. These findings align with the observations of previous studies conducted by Gracco et al. [38], Goya et al. [84], and Kirzioglu [86], which reported bilateral hypodontia involving the same teeth, albeit in a differing order of prevalence.
Given the functional and aesthetic implications of hypodontia, particularly in cases of multiple missing teeth, timely and strategic management is critical. A multidisciplinary approach involving orthodontists, oral surgeons, and prosthodontists is essential to ensure optimal outcomes. Preservation of alveolar bone is a key factor in treatment planning, often achieved through orthodontic strategies, such as delayed extraction of retained primary teeth and implant site switching, which help maintain bone volume and prepare sites for future implant placement [92]. In situations where bone loss has occurred, surgical interventions like bone grafting or distraction osteogenesis may be necessary [93]. Preventive orthodontic techniques, including space opening and the use of rigid bonded retainers, can further support alveolar ridge preservation and implant site stability. Individualized treatment planning and coordination among specialties are paramount, particularly as technological advancements continue to expand the possibilities in hypodontia management [94, 95].
There are some limitations in the research. While this study provides valuable epidemiological data on hypodontia in the Nepalese population, several limitations must be acknowledged. First, as a single-center study utilizing convenience sampling, the findings may not fully represent the entire Nepalese population. Second, the retrospective design relied solely on panoramic radiographs, without clinical examinations or genetic analysis, limiting insights into etiological factors. Third, the exclusion of individuals with syndromic conditions and prior orthodontic treatment may have introduced selection bias. Fourth, while the study assessed hypodontia prevalence and patterns, it did not evaluate its functional, esthetic, or psychosocial impact. Lastly, although associated dental anomalies were noted, their statistical significance and clinical correlations require further investigation.
CONCLUSION
This study presents a comprehensive assessment of the prevalence and pattern of non-syndromic hypodontia among the Nepalese population, adding a critical data point to the global body of literature on dental anomalies. With a prevalence of 7.8%, hypodontia appears to be relatively common within this subgroup, with distinct demographic and anatomical patterns. The condition was significantly more prevalent in males, particularly affecting the maxillary arch and most frequently involving the maxillary lateral incisors. Unilateral hypodontia was found to be more common than bilateral cases, and the majority of cases fell within the mild category, involving one or two missing teeth. These findings mirror many international studies yet also highlight regional variation, reinforcing the influence of ethnic, genetic, and environmental factors, as well as differences in sampling methodology and diagnostic criteria.
Despite key methodological strengths, including robust sample size and standardized radiographic protocols, the retrospective, single-center design and absence of clinical and genetic data limit both generalizability and etiological insight. These constraints underscore the need for multicenter, prospective investigations integrating clinical, radiographic, and molecular diagnostics. Such studies are critical to refine early detection, optimize individualized treatment planning, and inform public health interventions aligned with population-specific risk profiles.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: S.D.: Study conception, design, and data collection; S.D., D.R., M.N.M.S.: Draft manuscript.
LIST OF ABBREVIATIONS
| NSH | = Non-syndromic Hypodontia |
| TA | = Tooth Agenesis |
| DNA | = Deoxyribonucleic Acid |
| PAX9 | = Paired Box Gene 9 |
| MSX1 | = Muscle Segment Homeobox 1 |
| AXIN2 | = Axis Inhibitor 2 |
| EDA | = Ectodysplasin A |
| IRC | = Institutional Review Committee |
| SPSS | = Statistical Package for the Social Sciences |
| FDI | = Fédération Dentaire Internationale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval for this study was obtained from the Institutional Review Committee of Kathmandu University School of Medical Sciences (IRC-KUSMS), Nepal. Reference number: IRC-KUSMS-61/19.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was waived for this retrospective study due to the exclusive use of de-identified patient data, which posed no potential harm or impact on patient care.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this article is available in the “Zenodo Repository” at “https://doi.org/10.5281/zenodo.15364185”, reference number “15364185”.
ACKNOWLEDGEMENTS
Declared none.


