All published articles of this journal are available on ScienceDirect.
Efficacy of Three Mouthwashes on Candida albicans in Patients with Denture Stomatitis: In Vivo Study
Abstract
Introduction
The oral mucosa provides an optimal environment for the colonization of microorganisms and fungi, exhibiting a variety of biological habitats. The accumulation of biofilm on dentures significantly contributes to the development of denture stomatitis. Mouthwashes have been proven to exhibit an antiseptic effect and are widely used due to their antimicrobial effects. This research aims to examine the antibacterial efficacy of three types of mouthwashes as denture cleansers for people with denture stomatitis.
Methods
Sixty patients were chosen from removable prosthodontics clinics and were categorized into groups treated with three different types of commercial mouthwashes (Tantum Verde, Hextol mouthwash, and Orovex). Subsequently, swabs were collected from each patient, and the fungal growth of Candida albicans was evaluated.
Results
All studied mouthwashes (Tantum Verde, Hextol mouthwash, and Orovex) effectively decreased the quantity of bacteria on dentures. Mouthwashes containing chlorhexidine showed better results on the inhibition of the growth of C. albicans in comparison to other mouthwashes.
Discussion
Maintaining proper oral hygiene for dentures is crucial for preventing and treating denture stomatitis. Chemical disinfectants are recognized for their significance over mechanical cleaning, such as effective disinfection and simplicity. Mouthwashes serve as an efficient method for cleaning dentures, and prolonged use may impact the material characteristics of the dentures, including surface roughness and coloration.
Conclusions
Tantum Verde, Hextol, and Orovex mouthwashes are effective in decreasing the C. albicans on dentures. The chlorhexidine mouthwashes show better results than other mouthwashes. Furthermore, using a wider array of microorganisms in future investigations might provide a more thorough comprehension of their involvement in denture-related complications.
1. INTRODUCTION
Denture Stomatitis (DS), also known as chronic erythematous candidiasis, is a chronic inflammatory condition of the oral mucosa that affects over 50% of individuals wearing dentures [1]. DS commonly affects the palatal mucosa and is more common in older populations, with women having a higher prevalence than men. The etiology of this condition is multifactorial, including trauma induced by dentures, long-term use, inadequate hygiene, eating habits, and systemic variables [2, 3]. DS is more likely to be seen in individuals with acrylic (polymethylmethacrylate, PMMA) dentures [4]. DS is also observed in healthy, younger adults who wear dentures [1, 4].
The causative factor for the DS is the microbial film [5, 6]. PMMA dentures are rapidly colonized by bacteria and Candida species, such as Staphylococcus or Enterobacteriaceae species. These microbial reservoirs can cause DS and aspiration pneumonia, particularly in older individuals [7, 8].
For the dependent elderly people, dental and denture hygiene is often inadequate. Denture hygiene is a common concern among elderly individuals living in shelters and disabled denture users [3]. Saliva plays a dual role in the adherence of Candida to PMMA [6, 9]. It serves a cleansing function and contains antimicrobial components such as immunoglobulins, lysozymes, glycoproteins, peroxidase, and lactoferrin. These chemicals engage with Candida species, diminishing their adherence and colonization [10]. Decreased salivary secretion increases the adhesion of Candida to the denture base and surrounding mucosal surfaces, ultimately progressing to the hyphal form, penetrating the mucosal tissue, and inducing inflammation, clinically referred to as DS [2]. The removable prosthesis is a major risk factor for developing DS, including poor oral hygiene and persistent use of dentures [5, 6, 11].
Mouthwashes are used to preserve optimal oral health and for cleaning dentures. Chlorhexidine gluconate (CHX) is a potent antiseptic agent that is effective against several bacterial spores, fungi, and viruses [5, 12]. It has been reported that there is microbiological and clinical efficacy of chlorine dioxide (ClO2) as a topical antiseptic and disinfection agent used for the treatment of candidiasis in elderly patients [13]. CHX is useful in the treatment of DS. However, the brown appearance of acrylic dentures soaked in CHX can be a significant barrier to utilizing it as a daily disinfection agent [12]. Benzydamine and benzydamine-containing MoWs reduced C. albicans adhesion and biofilm formation. Some of these effects are correlated with changes in QS molecule secretion [14]. Hence, this study aimed to compare the antimicrobial effects of three types of mouthwashes as denture cleaners in denture stomatitis patients. Tantum Verde, Hextol, and Orovex mouthwashes were used in this study. The hypothesis was that there was no difference in antimicrobial effects among the three types of mouthwashes as denture cleaners in denture stomatitis patients.
2. MATERIALS AND METHODS
2.2. Study Subjects
The research received approval from the Institutional Review Board and Ethics Committee of the Faculty of Dentistry at Sinai University, El Arish, Egypt (approval number: Proth 1-8-022). Informed consent was obtained from all patients before the study.
A group of complete denture-wearing patients were studied at the Removable Prosthodontic Clinic at Suez Canal University for 6 months. The patients were examined for denture stomatitis (erythema involving part or whole denture-bearing mucosa).
The patients were selected according to the following inclusion criteria.
- Use of a denture for over a year.
- Dentures with C. albicans.
- The patient’s age between 50 and 80 years.
- No systemic diseases.
The patients were excluded according to the following exclusion criteria:
- Denture fabricated less than a year.
- Patient with clean dentures without C. albicans.
- The patient’s age below 50 and above 80 years.
- Presence of systemic diseases requiring medication that affects the oral bacterial flora.
Sample size calculation:
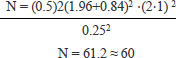 |
Where:
95% confidence is approximately 1.96.
80% power is approximately 0.84.
a standard deviation (σ) of the outcome is 1.
The expected difference between group means is 0.5.
A total of 60 patients (37 females and 23 males) were selected based on the inclusion criteria and were divided randomly into three groups (n = 20).
2.3. Study Details
Step 1. The patients’ dentures were cleaned by asking patients to soak them in denture cleanser for 8 hours. The patients were advised to use the denture and were not allowed to clean their dentures for 3 days.
Step 2. After the disinfection, the complete dentures were immersed in sterile distilled water for 3 minutes, and then swab samples were taken.
Step 3. The complete dentures were then treated with one mouthwash randomly. Twenty dentures were soaked in Tantum mouthwash (Tantum Verde, Eipico Egyptian INT., under license of A.C.R. spa Italy), 20 dentures were soaked in Hextol mouthwash (The Arab Drug Company (ADCO) – A.R.E), and 20 dentures in Orovex mouth (Macro Group, Egypt) as shown in Fig. (1). Each denture group was soaked for 30 minutes, which is a common method for reducing microbial contamination, especially significant microbial reduction, including Candida, Staphylococcus, and Streptococcus species [15, 16].
Step 4. Swabs were taken from the maxillary denture (palatal surface) and were cultured in a Dextrose agar medium, followed by microscopy examinations.
The solutions are labeled randomly as S1, S2, and S3 by a technician. The researcher conducting the microbiological analysis is unaware of the disinfectant types used.
2.4. Candidal Count
Candida colony count was carried out at 37ºC in aerobic conditions after incubation for 48 hours. Finally, C. albicans was differentiated from other species, which was done by its production of filaments and growth on corn meal agar. Figs. (2-4) show the Candida growth before and after the use of Tantum, Hextol, and Orovex mouthwashes. One investigator carried out all the microbiological procedures. The samples (30 µl/disc) were analyzed using the disc diffusion method against Candida collection isolates from different patients’ swabs [17]. Following incubation, the zone of inhibition (ZOI) around each disc is measured using a calibrated ruler in millimeters (mm). Results are evaluated against CLSI breakpoints for classification as susceptible (S), intermediate (I), or resistant (R). A significant zone of inhibition indicates that Candida is prone to the antifungal agent. Minimal or absent zone of inhibition (ZOI) indicates that Candida exhibits resistance to the antifungal agent.

Various types of mouthwashes (Tantum Verde, Hextol mouthwash, Orovex mouth) were used in this study.
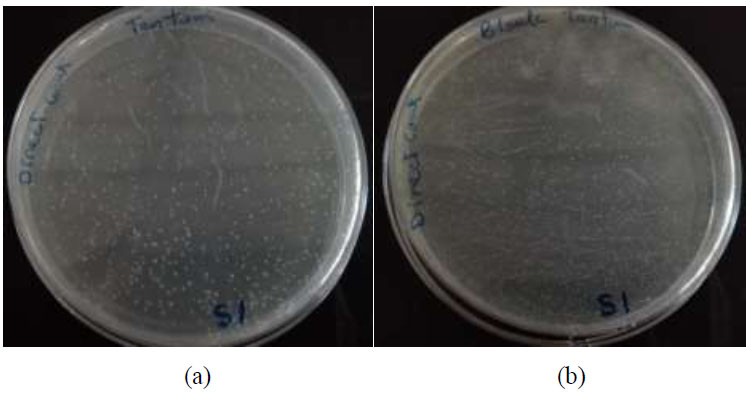
Candida growth before (a) and after (b) the use of Tantum mouthwash.
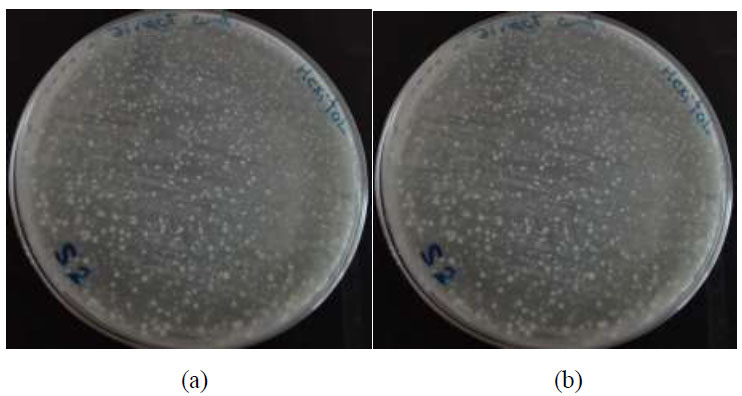
Candida growth before (a) and after (b) the use of Hextol mouthwash.
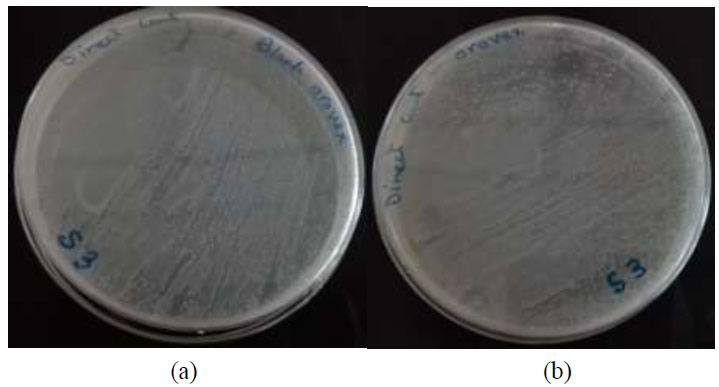
Candida growth before (a) and after (b) the use of Orovex mouthwash.
2.5. Statistical Analysis
Descriptive statistics were calculated for all three types of mouthwashes (Tantum Verde, Hextol mouthwash, and Orovex). Data were analyzed using SPSS 18 and multiple comparisons were performedusing One-way ANOVA and post hoc using the Scheffe Test at the significance level of 0.05.
3. RESULTS
The differences in Candida growth before and after the treatment of three mouthwashes were examined. All mouthwashes showed a reduction in the number of C. albicans CFU. Table 1 shows the results of descriptive statistics, and Table 2 shows the multiple comparisons of the results. Fig. (5) shows the line chart showing the different effects of the three tested mouthwashes. Hextol mouthwash showed the most effective method used in the study by inhibiting or decreasing the growth of Candida in comparison to the used types of mouthwashes. It showed a significant difference between the Hextol group and both the Tantum and Orovex groups. The Orovex mouthwash showed less efficacy on Candida than the Hextol mouthwash, and the least effective was the Tantum mouthwash.
| Groups | N | Mean | Std. Deviation | Std. Error | 95% Confidence Interval for Mean | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Hextol | 20 | 15.50 | 5.359 | 1.695 | 11.67 | 19.33 | 8 | 25 |
| Orovex | 20 | 7.40 | 4.222 | 1.335 | 4.38 | 10.42 | 0 | 11 |
| Tantum | 20 | 1.80 | 2.898 | 0.917 | -0.27 | 3.87 | 0 | 6 |
| (I) Group | (J) Group | Mean Difference (I-J) | Std. Error | p-value |
|---|---|---|---|---|
| Hextol | Orovex | 8.100* | 1.914 | 0.001* |
| Tantum | 13.700* | 1.914 | <0.001* | |
| Orovex | Hextol | -8.100* | 1.914 | 0.001* |
| Tantum | 5.600* | 1.914 | 0.024* | |
| Tantum | Hextol | -13.700* | 1.914 | <0.001* |
| Orovex | -5.600* | 1.914 | 0.024* |
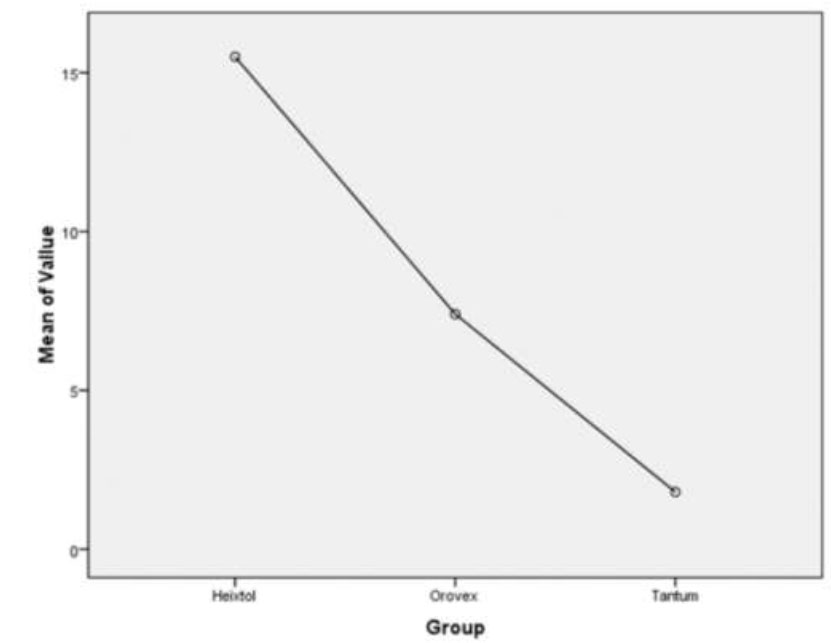
The line chart illustrates the different effects of the three tested mouthwashes.
4. DISCUSSION
The accumulation of biofilm on dentures significantly contributes to the development of denture stomatitis [15]. Furthermore, it has been determined that mechanical cleaning of dentures is inadequate in effectively decreasing the quantity of bacteria present in dentures and the palate [6]. Nevertheless, certain investigations have demonstrated that not all disinfectants exhibit efficacy against the primary pathogen responsible for denture-related issues, namely Candida [12]. Consequently, it has been proposed that all disinfectants should undergo examination in both laboratory settings and living organisms to resolve any discrepancies between investigations [13]. The saliva of most denture users contains these yeasts, which have a strong attraction to adhere to methacrylate resin. Maintaining proper oral hygiene for dentures is crucial for preventing and treating denture stomatitis [18, 19].
Chemical disinfectants are recognized for their many benefits over mechanical cleaning, such as effective disinfection and simplicity [3, 20]. After 30 minutes of immersion, Hextol was found to be more efficacious than Orovex and Tantum in diminishing Candida. Hextol contains CHX, which inhibits bacterial colonization of the teeth and the development of gingivitis [12, 13]. CHX exhibits antimicrobial properties against bacteria, fungi, and viruses responsible for several oral illnesses. The antibacterial actions of CHX in vitro are solely attributed to the modification of cell membrane permeability [21]. This statement is supported by a study that stated that immersing complete dentures in a 0.5% sodium hypochlorite or 0.12% CHX solution for 10 minutes weekly significantly decreased bacterial viability on complete dentures [22]. The CHX-based mouthwashes can be recommended for long-term use, but the side effects of the CHX need to be informed to the patient, i.e., there is a risk of denture discoloration that needs to be informed to the patient [23, 24].
Also, Orovex mouthwash was effective in the inhibition of Candida due to the CHX in its composition and the presence of thyme, which has been proven to have antifungal effects [19, 24]. Thyme possesses significant amounts of carvacrol, thymol, and thymoquinone, making it suitable for the therapeutic management of DS. Carvacrol is one of the major components of Origanum Syriacum’s anti-fungal effectiveness [25].
This is in agreement with Pavarina et al. [26], who found CHX effective as a denture cleanser using different concentrations. Their study evaluated chemical agents for cleaning and disinfecting removable dental prostheses, finding that CHX, sodium hypochlorite, and alkaline peroxide effectively reduced microorganism growth. An in vitro study showed that CHX mouthwash without alcohol, such as Curasept, Meridol, Dentosan, and Parodontax, has the strongest effects against Candida biofilm formation, but Streptococcus also forms biofilms [27].
The main composition of the Tantum mouthwashes is benzydamine, which affects Candida growth in high concentrations but has decreased or no effect in low concentrations. The Tantum group has the least effect on Candida, which may be due to the decreased concentration of benzydamine. Studies indicated that benzydamine, at a dosage of 0.6%, effectively suppressed fungal viability regardless of the duration of contact. Additionally, treatment with 0.3% benzydamine resulted in a consistent 2-log reduction in fungal viability across all contact durations. There were no noticeable impacts on the survival of fungi following exposure to the lowest levels of benzydamine [14, 28].
The considerable decrease in the quantity of C. albicans seen in this study indicates that mouthwashes are an appropriate means of cleansing dentures for the general population. Further research can be performed to include various other bacteria and fungi. Additional research can be done to ascertain whether regular utilization of mouthwashes can decrease the elevated occurrence of people with denture stomatitis.
On the other hand, Lamfon et al. [29] studied denture biofilms and their susceptibility to Candida spp. in vitro. They found that single agents like miconazole, fluconazole, or CHX did not inhibit Candida growth. Combinations of miconazole and CHX reduced the growth of bacteria and Candida for several days.
The main drawback of using chemical cleansers is their effect on denture material properties. Using chemical cleansers for a month can significantly alter the surface roughness of the acrylic denture base. However, the curing protocol after polymerization is crucial for improving surface stability. The effect of chemical cleaners was more noticeable in long-term cycle curing, as short-term procedures tend to create roughness. Long-term cycle curing is recommended for reducing surface roughness [27]. Daily disinfection of dentures with CHX may not cause very serious side effects on the teeth in the short term, but in long-term use, changes in the color of denture have been reported [30].
There are some limitations in this research. The research focused only on C. albicans, a major pathogen in denture stomatitis. Nonetheless, other bacterial and fungal species potentially implicated in denture-associated oral infections were not taken into account. Broadening the study to include a greater variety of diseases may provide a more thorough understanding of the efficacy of various disinfectants. In addition, the study concentrated on the short-term effects of disinfectants, whereas the long-term implications, including changes to the properties of denture material and other side effects like discoloration, were not thoroughly investigated. Longitudinal studies are essential to evaluate the longevity and safety of disinfectants over prolonged durations.
CONCLUSION
In conclusion, the formation of biofilm on dentures significantly contributes to the onset of denture stomatitis, with Candida as a principal pathogen implicated. CHX-based treatments, such as Hextol and Orovex mouthwash, have shown substantial antifungal efficacy, especially against C. albicans. The use of thyme in Orovex significantly amplifies its antifungal efficacy, making it a suitable option for denture hygiene. The efficiency of disinfectants is contingent upon their composition and concentration, as shown by Tantum mouthwash, which has limited effects on Candida proliferation at lower doses of benzydamine. While mouthwashes serve as an efficient method for cleaning dentures, their prolonged use may impact the material characteristics of the dentures, including surface roughness and coloration. Furthermore, using a wider array of microorganisms in future investigations might provide a more thorough comprehension of their involvement in denture-related complications.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: S.Z.: The study conception and design were carried out; G.A.: Conceptualization was done; W.Y.A. and E.A.T.: Methodology was developed; D.R.: The analysis and interpretation of results were performed. The draft manuscript was prepared by NSI. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DS | = Denture stomatitis |
| C. albicans | = Candida albicans |
| PMMA | = Polymethyl methacrylate |
| CHX | = Chlorhexidine gluconate |
| ClO2 | = Chlorine dioxide |
| ANOVA | = Analysis of variance |
| SPSS | = Statistical package for social sciences |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research received approval from the Institutional Review Board and Ethics Committee of the Faculty of Dentistry at Sinai University, El Arish, Egypt (approval number: Proth 1-8-022).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
ACKNOWLEDGEMENTS
Declared none.


